When a stroke strikes, it does so with brutal speed. In just minutes, brain cells begin to die, and with them, speech, movement, memory, and independence can be lost. Stroke is one of the world’s leading causes of death and long-term disability, and despite decades of research, treatment options remain limited. Nearly 90% of strokes are ischemic, caused by a blood clot choking off circulation to part of the brain. The best current treatment—clot-busting drugs—must be administered within four and a half hours of the first symptoms. For many patients, that critical window closes before they can get help.
But what if time were not the enemy? What if the brain, even days after an injury, could be coaxed into healing itself? This is the question that researchers from the Keck School of Medicine of USC, the University of Zurich, and ETH Zurich in Switzerland are daring to explore. Their experimental work suggests that stem cell therapy may offer a second chance at recovery for stroke survivors, long after the standard treatment window has passed.
Reprogramming Cells to Heal the Brain
The innovative approach relies on the remarkable versatility of stem cells. Ruslan Rust, Ph.D., assistant professor of research physiology and neuroscience at USC, and his colleagues started with ordinary human blood cells and reprogrammed them into neural stem cells—cells capable of developing into the specialized neurons that make up the brain.
In their study, published in Nature Communications, these stem cells were transplanted into the brains of mice one week after an ischemic stroke. For comparison, another group of mice with strokes underwent surgery but did not receive the transplants. Over the following weeks, the differences between the two groups became striking.
The transplanted mice showed signs of healing that extended far beyond what untreated mice experienced. Their brains displayed reduced inflammation, stronger growth of neurons and blood vessels, and increased connections between nerve cells. Even the blood-brain barrier—a vital filter that shields the brain from toxins and pathogens—was healthier in mice that received stem cells.
A Return of Movement and Function
To truly measure whether the mice recovered, the researchers needed more than just microscopic evidence—they needed to know if the animals could regain lost function. Using artificial intelligence to track subtle changes in movement, they monitored the mice as they walked and climbed a ladder with uneven rungs.
The results were both precise and inspiring. Mice that received stem cell transplants regained their fine motor skills within five weeks. Their gait improved significantly compared to untreated animals, and they demonstrated abilities that suggested a real return of coordination and control.
Rust emphasized that recovery in animal models is notoriously difficult to measure. “We needed to see these little differences,” he explained. “The unbiased view we got through this deep learning tool gave us a lot more detail about this complex process.”
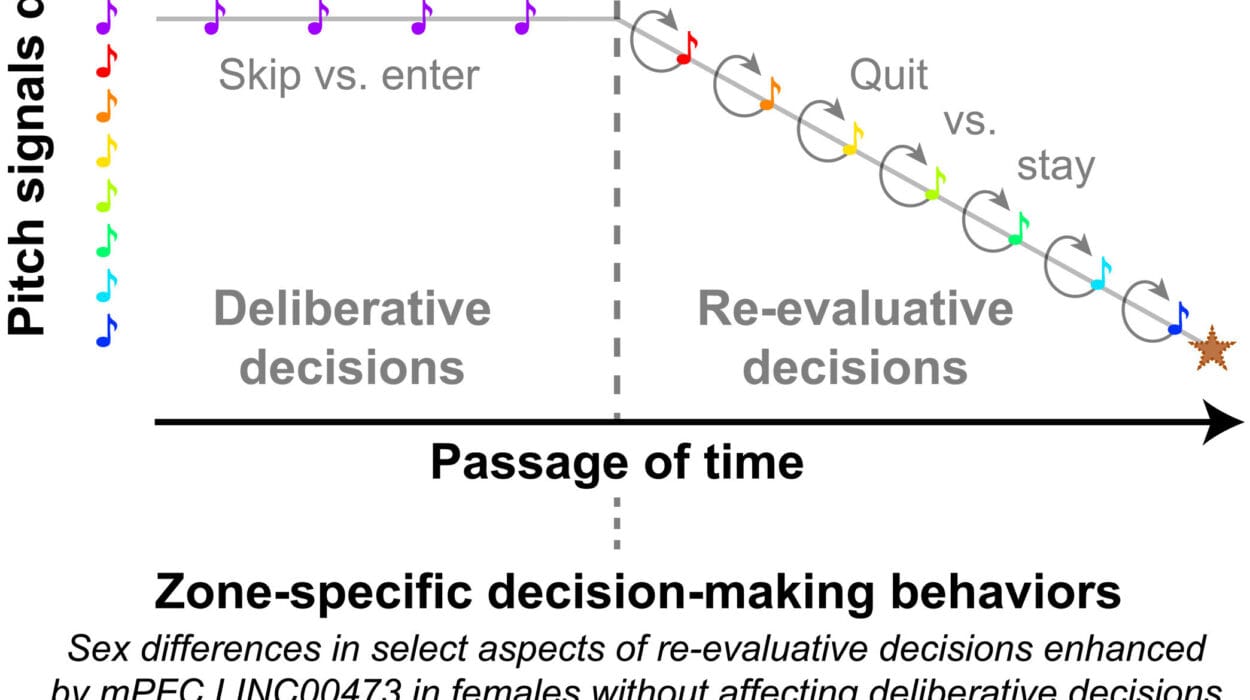
The Mystery of New Neurons
When the researchers examined which brain cells were lost in stroke, they noticed a sharp reduction in GABAergic neurons—specialized cells that produce the neurotransmitter GABA. These neurons play a critical role in regulating brain activity and have been linked to stroke recovery in previous research.
Intriguingly, the transplanted stem cells seemed to become what the brain most needed. Many of them developed into GABAergic neurons, suggesting that the damaged brain environment itself may guide stem cells toward replacing what was lost.
The scientists also uncovered robust activity in signaling pathways tied to neuron regeneration and connection-building. This hints at a deeper biological dialogue: transplanted cells and host tissue working together to rebuild what stroke had destroyed.
Why Mechanisms Matter
Understanding these cellular mechanisms is not only intellectually fascinating—it may be the key to developing future therapies. Rust and his team point out that if we know which pathways drive recovery, we might enhance them with drugs, including medications already approved for other conditions. This could expand treatment possibilities well beyond transplantation, opening new doors to recovery.
“Mechanistic insight can be quite important if we seek to inform new therapies or improve emerging ones,” Rust said. “It could open up a whole new wave of therapies.”
Looking Toward the Future
While the results in mice are promising, important questions remain. How long will transplanted stem cells survive in the brain? Will their benefits endure for months or years? Can they adapt to the complexities of a human brain injured by stroke? The research team is now studying longer-term outcomes in animal models, with the hope of one day moving this work into human trials.
“If we can help people by transplanting stem cells into a human stroke patient, we want the cells to be there for the rest of their life,” Rust explained. “Our aim is to look across the whole lifetime of a mouse and see what happens with the cells, and whether recovery is sustained or even improves.”
A Glimpse of Hope Beyond the Golden Hour
For stroke survivors and their families, the idea of a treatment that could bring recovery even after days or weeks is nothing short of revolutionary. Currently, many patients miss the narrow treatment window, leaving them with lifelong impairments. Stem cell therapy, if proven safe and effective in humans, could rewrite the rules of stroke care—transforming what has long been seen as permanent damage into something reversible.
The journey from laboratory breakthrough to clinical therapy is long, but this research offers a glimpse of a future where the brain’s resilience can be harnessed more fully than ever before. It represents not only a scientific milestone but also a deeply human aspiration: the chance to restore lives interrupted by the sudden cruelty of stroke.
In the end, this work reminds us of the brain’s incredible potential to repair itself when given the right tools—and of science’s relentless pursuit of hope, even in the face of one of medicine’s most devastating challenges.
More information: Human iPSC-derived cell grafts promote functional recovery by molecular interaction with stroke-injured brain, Nature Communications (2025). DOI: 10.1038/S41467-025-63725-3