Cortisol is often called the “stress hormone,” but this small molecule with a big reputation does so much more than fuel your fight-or-flight response. Secreted by the adrenal glands in response to signals from the brain, cortisol helps regulate blood sugar, metabolism, inflammation, immune response, and even memory. It’s a hormone of rhythm—rising in the morning to help you wake up and gradually declining through the day to allow you to rest. But for many women, cortisol doesn’t follow this elegant dance. Instead, it roars and lingers, whispering a constant message of stress, urgency, and unease throughout the body.
In the context of women’s health, cortisol has profound implications—from energy and weight gain to fertility, mental health, and chronic disease risk. Its influence is everywhere, quietly shaping the way women feel and function every day. The trouble begins when this essential hormone goes rogue—when chronic stress, poor sleep, hormonal fluctuations, or hidden inflammation push cortisol production into overdrive. Over time, what once protected the body begins to harm it, subtly but powerfully.
Understanding cortisol is not just about learning how to manage stress. It’s about decoding a hidden biological language that speaks to your immune system, your reproductive cycle, your emotions, and even your aging process. In this article, we’ll take a deep dive into how cortisol works, how it affects women differently than men, and how it weaves its way into nearly every aspect of female health.
Cortisol’s Daily Script: The Natural Rhythm of Stress
Every morning, just before you wake, your cortisol levels start to rise. This surge, known as the “cortisol awakening response,” is part of your body’s natural circadian rhythm. It gives you a boost of energy, increases alertness, and helps mobilize the fuel you need for the day ahead. In a healthy body, cortisol tapers off by the afternoon and reaches its lowest levels at night, allowing melatonin—your sleep hormone—to rise and lull you to sleep.
This daily rhythm isn’t random. It’s synchronized by your brain’s master clock in the hypothalamus and supported by the adrenal glands perched above your kidneys. When everything is in balance, cortisol works seamlessly with other hormones to help regulate appetite, maintain blood pressure, and moderate immune activity. It’s like the conductor of a symphony, keeping the orchestra of hormones, neurons, and systems in time.
But modern life often disrupts this rhythm. Irregular sleep patterns, late-night scrolling, skipped meals, and emotional stress all send confusing signals to the brain, which then misfires the command to produce cortisol. The result is cortisol out of sync: too high when it should be low, too low when you need energy, or stuck in overdrive around the clock.
Stress in a Female Body: The Gender Divide
While both men and women produce cortisol in response to stress, women tend to be more sensitive to its effects. This heightened sensitivity is partly biological and partly shaped by social and psychological stressors that disproportionately affect women. Hormonal fluctuations throughout the menstrual cycle, during pregnancy, and across menopause also influence how cortisol behaves and how the body responds to it.
Estrogen and progesterone—key female sex hormones—modulate cortisol’s activity in intricate ways. Estrogen can buffer the stress response, dampening the release of cortisol, while progesterone may have a more complex relationship, sometimes amplifying cortisol’s effects depending on the context and the phase of the menstrual cycle. This interplay means that a woman’s response to stress is never just about cortisol alone. It’s always filtered through the shifting hormonal tides of her body.
Research has also shown that women often experience more chronic stress than men, particularly related to caregiving, emotional labor, and societal expectations. This persistent low-grade stress can keep cortisol levels elevated over time, leading to a cascade of health effects—from fatigue and weight gain to anxiety and disrupted periods.
The Weighty Issue: Cortisol and Body Fat
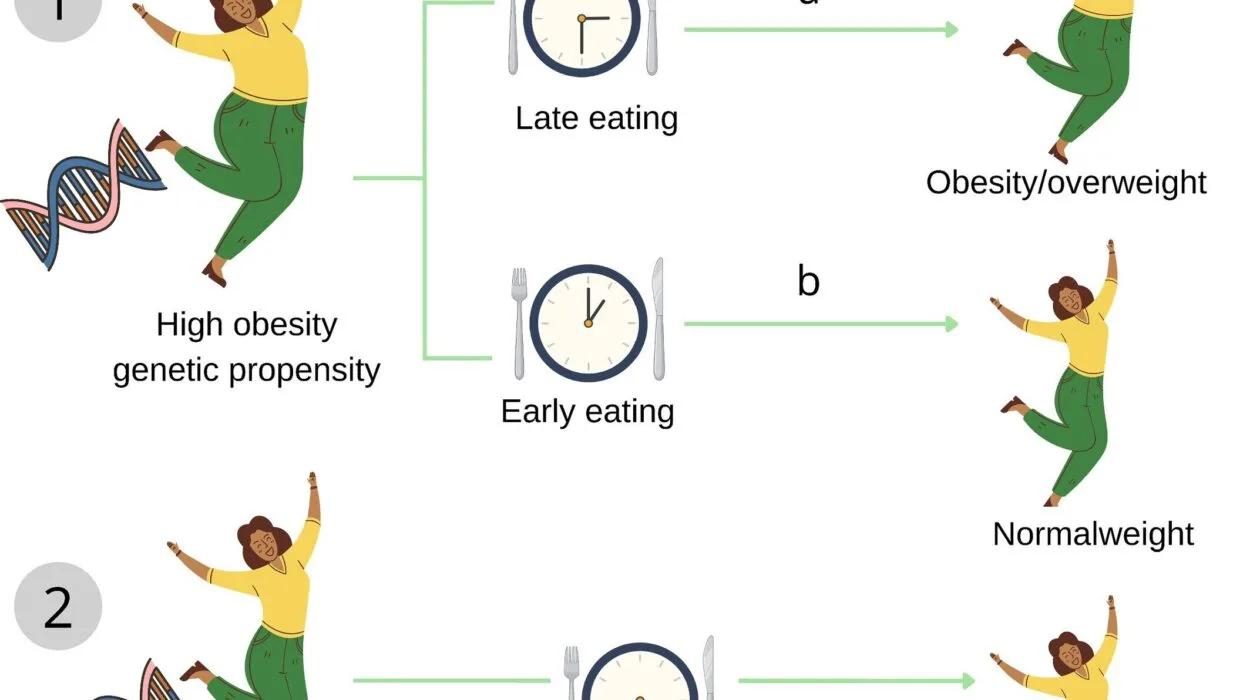
One of the most well-known effects of elevated cortisol is its role in weight gain, particularly around the abdomen. This isn’t just about calories in and out; it’s a hormonal signal. When cortisol is chronically elevated, it tells the body to store fat—especially visceral fat, the type that surrounds internal organs and is associated with higher risks of diabetes and heart disease.
Cortisol’s influence on fat storage is tied to its relationship with insulin and glucose. Under stress, the body enters a survival mode that prioritizes quick energy. Cortisol increases blood sugar levels and makes you more insulin resistant, meaning your cells become less responsive to insulin’s signal to absorb glucose. This can lead to increased hunger, cravings for sugary and fatty foods, and greater fat storage—especially if stress is ongoing.
For many women, this means that even with a healthy diet and regular exercise, stress can become a metabolic barrier. You might feel like you’re doing everything right, yet the scale won’t budge—or worse, it creeps upward. Understanding cortisol’s role in metabolism helps explain why managing stress and supporting adrenal health are just as important as diet and fitness in any weight management plan.
Sleep and the Cortisol Conundrum
Poor sleep and high cortisol go hand-in-hand, creating a vicious cycle. When cortisol levels remain elevated at night, they interfere with melatonin production and disrupt sleep quality. You may find it hard to fall asleep, wake frequently during the night, or wake up feeling unrefreshed—even after a full eight hours in bed.
Sleep deprivation, in turn, raises cortisol levels the next day. This triggers more stress, more cravings, more irritability, and more fatigue. The cycle continues, often unnoticed, until exhaustion becomes the new normal. For women, especially those juggling work, caregiving, and household responsibilities, sleep can become a casualty of modern life. But its cost is immense. Without adequate, restorative sleep, the entire hormonal orchestra falls out of tune.
Improving sleep hygiene—through consistent bedtime routines, light exposure during the day, and limiting screens at night—can help reset your cortisol rhythm. But in some cases, deeper interventions are needed, especially when insomnia is driven by underlying stress or hormonal imbalance.
Menstrual Mayhem: How Cortisol Disrupts the Cycle
High cortisol doesn’t just interfere with sleep and weight—it can also throw your menstrual cycle off course. Chronic stress can delay ovulation, shorten or lengthen the cycle, and even cause missed periods. This happens because cortisol communicates with the hypothalamus, the part of the brain that also regulates the reproductive hormones LH and FSH, which are crucial for ovulation and menstruation.
In extreme cases, this disruption is known as hypothalamic amenorrhea—when the brain stops signaling the ovaries to produce hormones, often due to chronic stress, under-eating, or excessive exercise. But even moderate cortisol dysregulation can cause symptoms like PMS, irregular periods, or worsened cramps.
The menstrual cycle is a delicate feedback loop that relies on balance. When cortisol is consistently elevated, the body prioritizes survival over reproduction. It’s as if the body is saying, “Now is not a safe time to conceive.” This ancient mechanism may have served our ancestors well in times of famine or danger, but in today’s world, it often backfires—especially when the stress is emotional, not physical.
Fertility and the Stress Factor
The link between stress and fertility is well established, yet it’s often overlooked in fertility treatments and discussions. Women struggling to conceive may be advised to take supplements, track ovulation, and undergo hormone testing—without anyone asking about stress levels, sleep, or emotional well-being.
Yet cortisol affects every stage of the reproductive process—from ovulation and implantation to hormone production and egg quality. Elevated cortisol can reduce progesterone levels, delay ovulation, and even affect the uterine lining. It also interacts with thyroid function, which plays a vital role in fertility. Women with hypothyroidism often have elevated cortisol, and vice versa.
In assisted reproductive technology (ART) procedures like IVF, stress management can significantly impact outcomes. Studies have shown that women with lower stress levels during treatment have higher success rates. Mind-body practices like meditation, yoga, acupuncture, and even guided journaling have been shown to reduce cortisol levels and improve fertility outcomes.
Pregnancy, Postpartum, and Cortisol’s Quiet Influence
During pregnancy, cortisol levels naturally rise—especially in the third trimester—to support fetal development and prepare the body for labor. The placenta even produces its own form of corticotropin-releasing hormone (CRH), which stimulates cortisol production. In moderation, this is a healthy and necessary adaptation.
But if cortisol is chronically elevated before or during pregnancy, it can increase the risk of complications such as preeclampsia, preterm birth, and low birth weight. Cortisol also crosses the placenta and can influence fetal brain development, potentially setting the stage for stress sensitivity in the child’s future life.
After birth, cortisol levels should gradually decline, but for many new mothers, the stress doesn’t end. Sleep deprivation, hormonal shifts, and the demands of caregiving can keep cortisol high—contributing to postpartum mood disorders, anxiety, and fatigue. Supporting adrenal recovery during the postpartum period is critical but often neglected. Strategies like nourishment, sleep support, emotional validation, and community care are vital for bringing cortisol levels back into balance.
Cortisol, Perimenopause, and the Midlife Shift
As women enter their 40s and 50s, cortisol begins to play an even more central role in health and well-being. Estrogen and progesterone levels decline, and with them go many of the protective effects against stress. This hormonal shift means that women in perimenopause and menopause often experience more intense reactions to stress, poorer sleep, and stubborn weight gain—especially around the belly.
Without the calming influence of progesterone and the mood-stabilizing effects of estrogen, cortisol can wreak havoc. Anxiety, irritability, insomnia, brain fog, and mood swings often rise—fueled not just by hormonal decline but by an overactive stress response. This is also the time when chronic inflammation, insulin resistance, and cardiovascular risks increase—all influenced by cortisol’s activity.
Supporting adrenal health during perimenopause is crucial. This doesn’t mean eliminating stress altogether, but rather learning how to respond to it differently. Practices like meditation, breathwork, nature exposure, and even gentle strength training can help recalibrate the body’s stress response. Adaptogenic herbs like ashwagandha and rhodiola may also support cortisol balance during this transition, though they should be used with guidance.
The Mind-Body Bridge: Cortisol, Anxiety, and Depression
Cortisol’s impact on mental health is profound. High cortisol levels are associated with anxiety, irritability, and even depression. When cortisol is elevated for too long, it changes the structure and function of the brain—particularly in areas like the hippocampus and amygdala, which govern memory, fear, and mood.
Women are already more prone to anxiety and depression than men, partly due to hormonal fluctuations and social stressors. Add chronic cortisol elevation to the mix, and the risk increases. This is why stress management isn’t just about feeling better—it’s about protecting your brain and emotional health.
Fortunately, the brain is plastic. It can change and heal. Practices like mindfulness, cognitive-behavioral therapy, somatic experiencing, and regular exercise can reduce cortisol and support mental resilience. Social connection also plays a critical role. Oxytocin—the hormone of bonding and trust—can counteract cortisol’s effects, highlighting the importance of community, friendship, and affection in stress recovery.
Rewriting the Cortisol Story: A Holistic Path to Balance
There’s no single solution for cortisol imbalance. It’s a multifaceted issue that touches nearly every aspect of a woman’s life. But healing begins with awareness—with recognizing that stress is not just emotional or psychological. It’s deeply biological, and it’s written into your body in the language of hormones.
Rebalancing cortisol requires a holistic approach: quality sleep, nourishing food, regular movement, meaningful rest, emotional processing, and sometimes medical support. It means listening to the body’s whispers before they become screams. It means understanding that self-care is not indulgent—it’s essential biology.
Women are not fragile beings broken by stress. They are adaptive, powerful, and resilient. But even the strongest systems need support. By learning how cortisol affects your body, you can begin to respond differently—to your stress, your health, and your needs.
And in that response lies transformation.