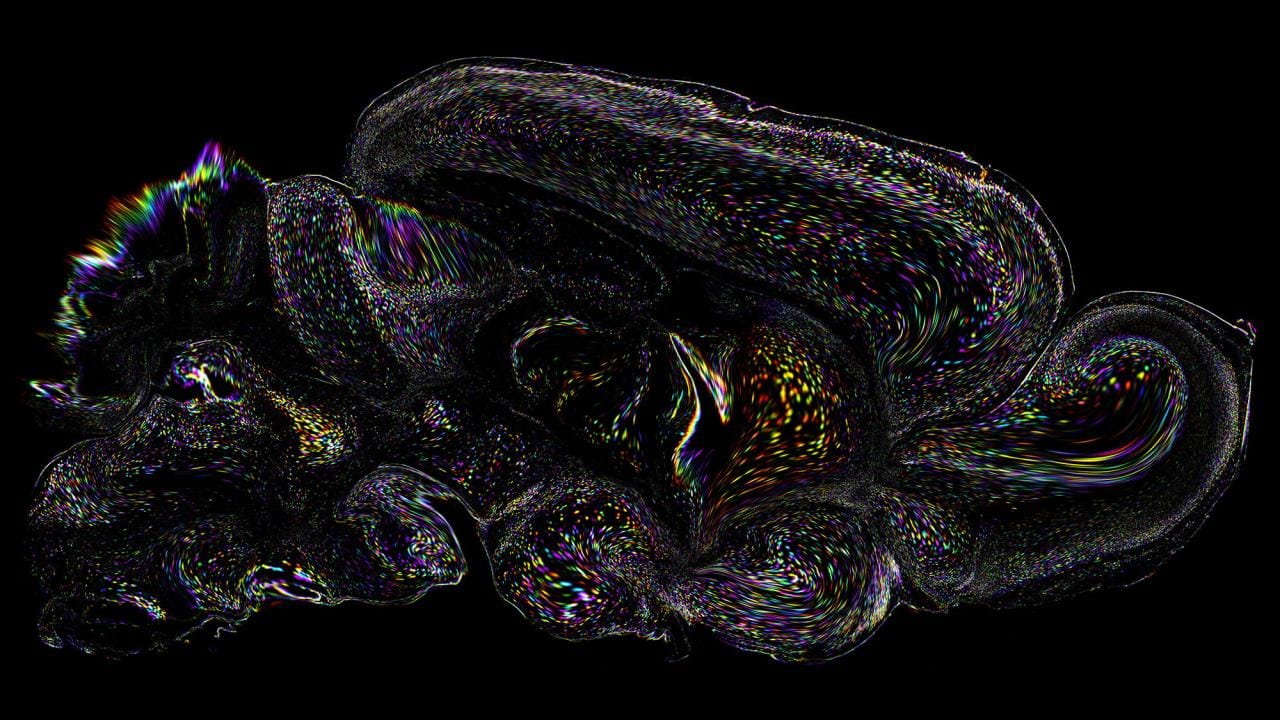
In the quiet corridors of the brain, where thoughts bloom and memories form, scientists are learning how to whisper to the mind without causing a psychedelic storm. In a groundbreaking study published August 4 in Nature Neuroscience, researchers at the University of California, Davis have peeled back another layer of the mystery surrounding psychedelic compounds—and in doing so, have illuminated a path toward safer, non-hallucinogenic treatments for depression and other mental health disorders.
Their discovery challenges long-standing dogmas in the field of psychedelic neuroscience. It turns out that the profound changes in brain structure and function attributed to psychedelics—the very properties that give them their therapeutic power—don’t necessarily require the hallucinations that make them controversial and difficult to manage in clinical settings.
The Promise of Psychedelics Beyond the Psychedelia
For decades, the idea that psychedelics could treat depression, PTSD, and anxiety was both alluring and elusive. Studies showed that drugs like psilocybin and DMT could produce lasting relief in patients suffering from severe mental illness—sometimes after just a single dose. But these benefits came tethered to intense hallucinogenic experiences, which can be psychologically destabilizing and limit the settings in which such drugs can safely be used.
Understanding exactly how these drugs remodel the brain—how they coax it into forming new neural pathways, reconnecting regions silenced by trauma or stress—is the holy grail of psychedelic medicine. The challenge has always been to uncouple the “trip” from the treatment. That’s where the UC Davis research enters with a bang.
Led by David E. Olson, professor of chemistry and molecular medicine and director of the Institute for Psychedelics and Neurotherapeutics, the team has provided compelling evidence that psychedelics’ power to promote neuroplasticity—the brain’s ability to adapt, learn, and rebuild—is separate from the hallucinations that often accompany them.
A Tale of Two Molecules: Psychedelic vs. Non-Psychedelic
The research centered on two related molecules: 5-MeO-DMT, a powerful hallucinogenic compound found in certain toads and plants, and its synthetic analog tabernanthalog (TBG), which does not produce hallucinations.
Both compounds were tested in animal models to assess their effect on the brain’s structural plasticity—essentially, their ability to stimulate the growth of new dendritic spines, the small protrusions on neurons that enable communication between brain cells. These spines are often reduced or lost in people with depression, and restoring them has been a key aim of new antidepressant treatments, including ketamine.
The results were striking: TBG promoted dendritic growth and produced lasting antidepressant-like effects—without triggering hallucinations.
“It was kind of shocking,” said Olson. “TBG promoted plasticity, but the glutamate burst and immediate early genes were not required.”
This contradicts the dominant theory in the field, which holds that psychedelics work by creating a massive, short-lived surge of glutamate—the brain’s main excitatory neurotransmitter—followed by the activation of certain genes known to initiate plasticity. But in the case of TBG, neither of these elements seemed necessary.
Turning On Plasticity Without Turning Off Reality
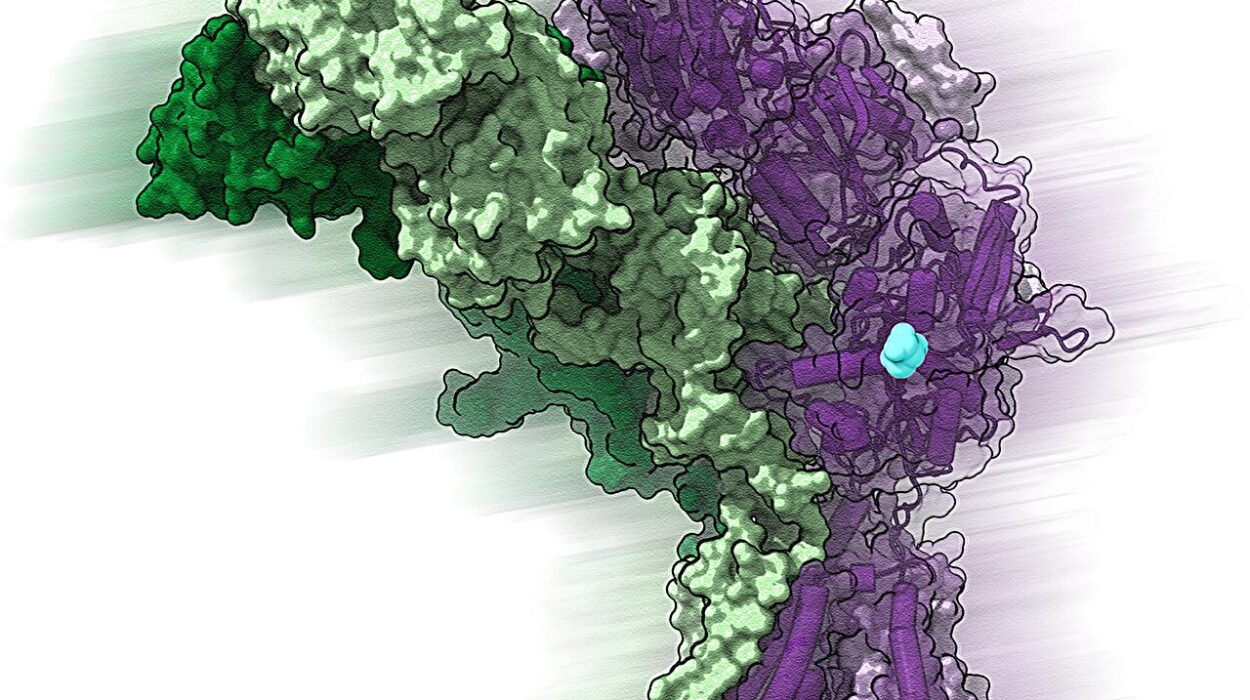
To understand how this works, the team used genetic and pharmacological tools to trace the exact pathway of activity triggered by both 5-MeO-DMT and TBG. Both compounds act on the 5-HT2A serotonin receptor, the classic “psychedelic receptor” in the brain. This receptor is known to play a key role in both hallucinations and neuroplasticity. The difference? How hard it gets turned on.
Olson likens it to a faucet. A full agonist, like 5-MeO-DMT, blasts the water on at full force—creating both psychedelic experiences and brain rewiring. A partial agonist like TBG turns the faucet only partway. There’s no overwhelming flood, no mind-bending visuals—but the brain still gets the gentle push it needs to grow new connections.
That mild activation still triggers a cascade of intracellular signals, activating proteins like TrkB, mTOR, and AMPA receptors—familiar actors in the neuroplasticity playbook. The spines grow. The synapses strengthen. The mood lifts.
“Full agonists turn on hallucinations and they also turn on plasticity,” Olson explained. “Partial agonists only turn on the receptor part way and that seems to be sufficient to turn on plasticity.”
Connecting Plasticity to Emotional Healing
But can dendritic growth alone explain the therapeutic effects? The UC Davis team wanted to know if the physical changes in the brain were truly responsible for the psychological improvements seen in depression models.
They got their answer using an ingenious genetic technique: after dosing animals with TBG and observing increased dendritic spine growth in the prefrontal cortex—a region crucial for decision-making and emotion regulation—they used targeted laser light to selectively erase the new spines. The result was profound: when the spines disappeared, so did the antidepressant effects.
This is the first time such an experiment has been successfully carried out with a serotonergic psychedelic analog, strengthening the argument that neuroplasticity is not just a side effect, but a central mechanism for the antidepressant benefits.
“This is the first time that we’ve done this with a serotonergic agent,” Olson noted. “And we find that cortical neuroplasticity is at least responsible for some of the compound’s antidepressant-like effects.”
Redefining What Makes Psychedelics Work
The revelation that glutamate surges and immediate early gene activation are not required for neuroplasticity flips a key assumption in the psychedelic science community. These phenomena may be more closely tied to the hallucinatory effects of psychedelics rather than their healing potential.
John A. Gray, co-author and professor at UC Davis, underscored the importance of this paradigm shift: “Science is full of surprises. There is still so much we don’t know about how psychedelics impact the brain, and it feels like we learn something new every day.”
This study doesn’t just deepen our understanding of how psychedelics work—it opens the door to a future where non-hallucinogenic psychedelics could be used safely and effectively for widespread treatment of mental health disorders. No tripping. No unpredictable experiences. Just healing.
A Hopeful Future for Psychedelic Medicine
The implications are vast. Imagine a drug that brings the mental health benefits of LSD or psilocybin, but without the legal complications or need for supervised sessions. A pill that rewires the brain’s mood circuitry gently and precisely, without opening doors to other realms of consciousness.
TBG and other next-generation compounds being developed at UC Davis and elsewhere could one day fulfill that vision. By showing that neuroplasticity and hallucination can be biologically uncoupled, this research sets a new trajectory for psychiatric medicine—one that is grounded in evidence, safety, and accessibility.
There’s still much work to be done. Human clinical trials are the next big step. But the path forward is clearer than ever.
“By mapping these distinct pathways,” Olson said, “we can build compounds that maximize therapeutic benefit while minimizing side effects. That’s the future we’re working toward.”
In a world struggling with an epidemic of depression, anxiety, and trauma, the idea that we can heal the brain without breaking the mind is no longer just a dream. It’s becoming a scientific reality.
More information: The psychoplastogen tabernanthalog induces neuroplasticity without proximate immediate early gene activation, Nature Neuroscience (2025). DOI: 10.1038/s41593-025-02021-1