For more than a century, insulin has stood as the singular lifeline for people living with type 1 diabetes — a condition once considered a swift death sentence before its discovery in 1921. But now, a surprising hormone long associated with appetite control may be poised to revolutionize how we treat one of diabetes’ deadliest complications: diabetic ketoacidosis (DKA).
In a new analysis published in the Journal of Clinical Investigation, researchers at the University of Washington (UW) have re-examined a once-overlooked discovery made more than a decade ago — that leptin, a hormone produced by body fat, can reverse DKA even in the total absence of insulin. The new findings propose a radical shift in our understanding of diabetes: that the brain, not just the pancreas, may play a central role in the life-threatening spiral of DKA.
Diabetic Ketoacidosis: A Crisis of Miscommunication
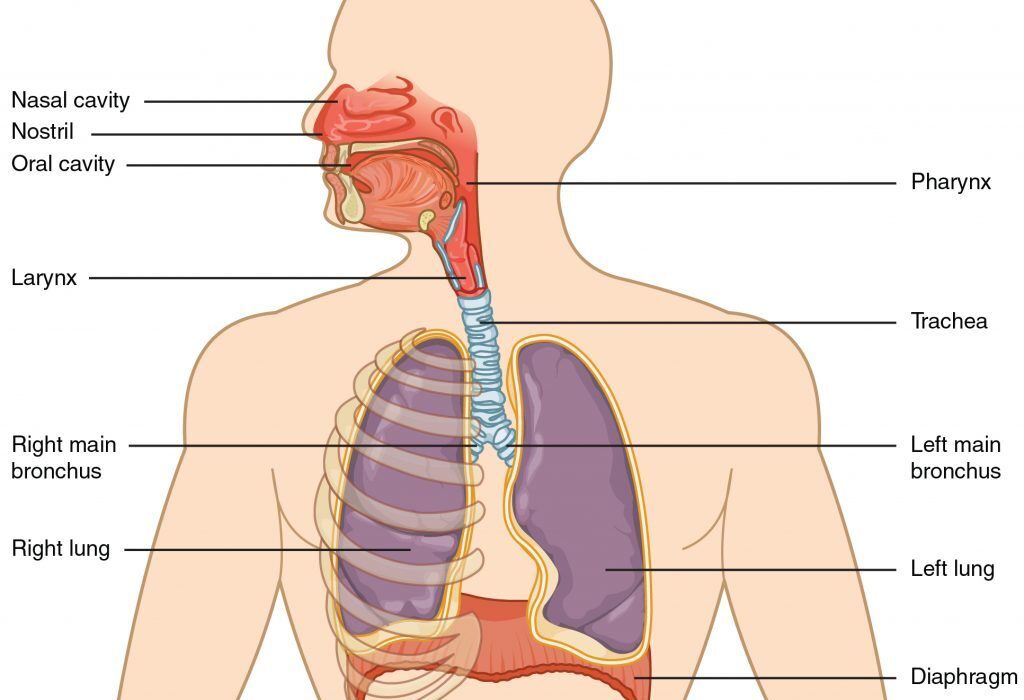
Diabetic ketoacidosis is a medical emergency. It occurs when the body can no longer produce insulin, typically in patients with type 1 diabetes. Without insulin, cells cannot absorb glucose, the body’s main fuel. In response, the body begins breaking down fat for energy, releasing ketones — acidic byproducts that, in high concentrations, make the blood dangerously acidic. This metabolic storm can cause vomiting, confusion, rapid breathing, and, if untreated, death.
Traditionally, insulin has been the only solution — restoring glucose uptake and halting ketone production. But this new research suggests something deeper is at work: the brain itself may be orchestrating the crisis.
The Brain’s Energy Command Center
Dr. Michael Schwartz, senior author of the new study and a professor of medicine at UW, describes the problem as a misunderstanding — not between people, but between the body and the brain.
“When the pancreas stops producing insulin, the brain misreads the situation,” said Schwartz. “It interprets the lack of insulin as a complete lack of fuel, even when glucose is actually present in the bloodstream.”
At the heart of this misinterpretation lies leptin, a hormone secreted by fat cells. Leptin’s job is to tell the brain — specifically the hypothalamus — how much energy is stored in the body. Low leptin levels signal an energy crisis, prompting the brain to activate survival mechanisms: releasing more glucose into the blood, encouraging fat breakdown, and even altering appetite.
In patients with type 1 diabetes, leptin levels fall dramatically when insulin disappears — even before DKA begins. The brain, unaware that this fuel shortage is only apparent, reacts as if the body is starving, triggering a dangerous chain reaction that raises blood sugar and ketone levels to catastrophic heights.
Leptin’s Astonishing Effect on DKA
This insight isn’t new — it began in 2011, when Schwartz and his team first experimented with leptin therapy in diabetic rodents. By delivering leptin directly into the brains of rats and mice with type 1 diabetes, they hoped to see if it could calm the brain’s “emergency response” to insulin loss.
At first, there was no change. But after four days, something remarkable happened: the animals’ blood glucose and ketone levels normalized completely. Even more astonishing, they stayed normal — no matter what the researchers did to manipulate their diets or glucose levels.
“The most amazing thing,” said Schwartz, “was that the blood sugars not only came down — they stayed down. If you tried to push them up, they came back down. If you tried to bring them down, they rebounded.”
It was as if the brain had recalibrated its understanding of the body’s energy state. In the absence of insulin, leptin appeared to have stepped in as a substitute signal, telling the brain that fuel stores were adequate — thereby halting the metabolic cascade that leads to DKA.
Why Was This Ignored?
Despite the implications, the 2011 findings were largely dismissed by the broader diabetes research community. At the time, the idea that DKA could be resolved without insulin — and that the brain was a key player — clashed with long-standing medical dogma.
But Schwartz and his colleagues didn’t give up. Over the years, additional studies and accumulating evidence continued to support their hypothesis. The new analysis in JCI draws on over a decade of this work, synthesizing rodent studies, hormonal analyses, and neurological data to build a compelling case that DKA is not just a matter of missing insulin — it’s a matter of a misinformed brain.
A New Era of Diabetes Treatment?
The implications of this work are staggering. If leptin can reliably prevent or reverse DKA, it could fundamentally change how type 1 diabetes is managed. Rather than focusing solely on replacing insulin, treatment might also involve resetting the brain’s response to energy signals.
“This is one of the most exciting discoveries of my career,” said Dr. Irl Hirsch, a co-author of the study and UW Medicine’s diabetes treatment and teaching chair. Hirsch, who has lived with type 1 diabetes since childhood, understands the burdens patients face — daily insulin injections, continuous blood sugar monitoring, and the constant threat of DKA.
“Don’t get me wrong,” he said. “The discovery of insulin 104 years ago is one of the greatest medical advances of the last century. But this — this is the next step. This might be a better way.”
Leptin and the Hypothalamic Switchboard
To understand how leptin works in this context, it helps to look at its role in the hypothalamus. This region of the brain is like an air traffic control center for energy use. When leptin levels are high — as in someone with abundant fat stores — the brain reduces appetite and limits energy mobilization. When leptin levels are low, the brain sounds the alarm, initiating hunger and metabolic responses that increase glucose and ketone production.
In type 1 diabetes, insulin loss leads to low leptin levels, which mislead the hypothalamus into thinking the body is starving. Administering leptin restores this signal, calming the brain and preventing it from driving the body into metabolic overdrive.
By acting on specific neurons in the hypothalamus — some of which are now being identified in animal studies — leptin could serve as a regulatory hormone, turning off the very circuits that trigger DKA in the first place.
Moving Toward Human Trials
Schwartz’s next step is to seek FDA approval for clinical trials in humans. The goal: to determine whether leptin could be a safe, effective treatment for people with type 1 diabetes, particularly those at risk of DKA.
The hope is not to replace insulin entirely — at least not yet — but to reduce the need for constant monitoring and to provide a failsafe mechanism for preventing DKA.
“If you could treat type 1 diabetes without daily insulin injections and constant blood sugar monitoring,” said Schwartz, “patients would say that is the greatest thing ever.”
A future where the brain, once considered a passive player in diabetes, becomes a therapeutic target could revolutionize treatment. Instead of fighting symptoms downstream, doctors might intervene at the neurological source — calming the storm before it begins.
A Paradigm Shift in Endocrinology
This new framework fundamentally challenges the prevailing view that insulin deficiency alone causes DKA. Instead, it positions the brain as both an instigator and a potential solution.
For decades, diabetes has been understood through the lens of pancreatic failure — the inability of beta cells to make insulin. But this work proposes a more holistic model, one in which the brain, fat tissue, and hormones like leptin form an interconnected system. When that system misfires, the result is not just high blood sugar, but a life-threatening cascade that begins with a simple misunderstanding.
Correct the message, and you may prevent the emergency.
Looking Ahead: Hope Beyond Insulin
While insulin remains essential, especially in acute care, the possibility that leptin or leptin-mimicking drugs could manage or even prevent DKA opens the door to a new era of diabetes care. And for millions of people living with type 1 diabetes, this represents more than scientific progress — it’s a promise of a freer, safer life.
A future where the brain understands what the body truly needs. Where treatment is not a daily burden, but a simple balance. Where the life-saving hormone of the 20th century, insulin, is joined by its long-overlooked partner: leptin.
As Hirsch puts it, “Insulin was the beginning. But this? This might be the next chapter.”
More information: Mirzadeh et al, An unexpected role for the brain in the pathogenesis of diabetic ketoacidosis, Journal of Clinical Investigation (2025). DOI: 10.1172/JCI196357