Stroke, a sudden assault on the brain’s lifeblood, continues to rank among the leading causes of death and disability worldwide. With millions of lives forever changed each year—through paralysis, speech loss, and cognitive decline—the aftermath of a stroke often feels like a battle only half-won. Current treatments focus narrowly on restoring blood flow, and time is the cruelest factor: if you miss the narrow window, options rapidly fade. But what if healing could begin after that window closes?
In a groundbreaking new study, scientists at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine), have found that a class of drugs currently used in cancer therapy could be repurposed to limit brain damage and boost recovery following ischemic stroke. The key lies not in blood vessels, but in the brain’s own immune cells: microglia.
Rewiring the Brain’s First Responders
Led by Professor S. Thameem Dheen, Dr. Kevin Jayaraj, and Dr. Jai S. Polepalli, the NUS Medicine research team has revealed that histone deacetylase inhibitors (HDACi), drugs already being tested for cancer and Alzheimer’s, can switch microglia from harmful instigators of inflammation into protectors of neurons.
Published in the prestigious journal Glia, the study represents a major step forward in addressing what scientists call the “second wave” of brain injury—a storm of inflammation that occurs hours to days after stroke, causing additional damage even after the initial attack has passed.
“HDACi are already being explored in cancer and neurodegeneration therapy,” said Prof Dheen. “What we now show is that they can be repurposed to dampen inflammation in the brain and promote recovery in stroke, through a microglia-centric mechanism.”
Stroke, Inflammation, and the Search for Better Treatments
An ischemic stroke—where a blood vessel supplying the brain becomes blocked—triggers a chain reaction of devastation. Neurons die from lack of oxygen. Tissues swell. Immune cells rush in, releasing molecules meant to clean up damage but often worsening it instead.
Among the immune responders are microglia, specialized brain cells that act like paramedics and janitors. In healthy brains, they clear debris and help with neural repair. But after a stroke, microglia can turn against the tissue they’re meant to protect—amplifying inflammation, killing off vulnerable neurons, and slowing recovery.
Until now, few treatments have aimed to control this second wave of injury.
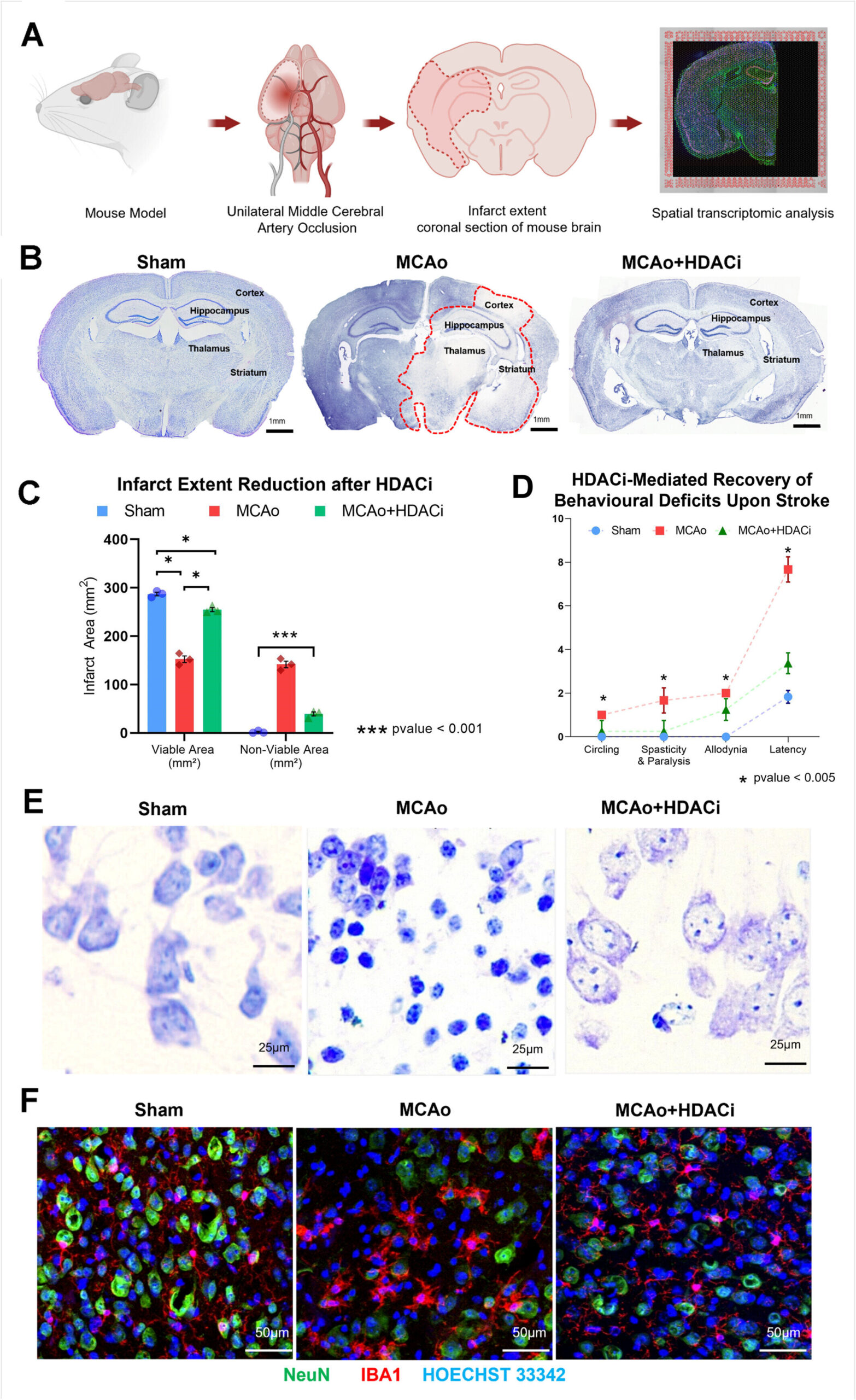
But the NUS researchers used cutting-edge tools like spatial transcriptomics—a method that maps gene activity across specific brain regions—to peer into the behavior of microglia following stroke and HDACi treatment. What they found was astonishing: in laboratory models, HDACi therapy not only slashed brain damage by 60%, but also reprogrammed microglia into repair mode.
Mapping the Brain’s Molecular Rebirth
To simulate stroke, researchers blocked blood flow in the middle cerebral artery of animal models. Then they introduced HDACi therapy and monitored what happened at both molecular and behavioral levels. The results were striking: not only did HDACi reduce tissue damage, but treated animals also showed improved performance in behavioral tests that measure memory, coordination, and emotional response.
At the cellular level, spatial transcriptomics revealed that microglia in HDACi-treated brains were no longer flooding the environment with inflammatory signals. Instead, they were expressing genes linked to neuroprotection, phagocytosis (clearing cellular debris), and cell survival.
Even more intriguing, these changes weren’t uniform across the brain. The effects were region-specific, with critical zones like the hippocampus—a structure involved in memory—showing particularly robust shifts in microglial behavior.
“Our study demonstrates for the first time that HDACi can restore neuroprotective gene activity in microglia in a region-specific manner across the brain, including critical areas such as the hippocampus,” explained Dr. Jayaraj. “This gives us new therapeutic targets for conditions where neuroinflammation plays a major role.”
From Cancer to Stroke Recovery
HDACi drugs work by modifying gene expression. They alter how tightly DNA is wound around histone proteins, essentially turning genes on or off without changing the genetic code. This ability to reprogram cells has made them useful in treating certain cancers and neurodegenerative diseases.
Now, thanks to this study, they’re being looked at through a new lens—as tools to fine-tune immune responses in the injured brain.
Professor Thiruma V. Arumugam, co-author of the study from La Trobe University in Australia, underscored the implications: “HDACi drugs precisely reprogram microglia in stroke-affected brain regions, transforming them from inflammatory agents to healing promoters. By targeting these immune cells, our study has the potential to address both acute damage and long-term recovery post-stroke.”
This dual-action approach—minimizing initial damage and boosting later repair—is a game-changer. Most current stroke therapies are limited by time; clot-busting drugs must be administered within hours, and beyond that window, options dwindle. But HDACi may offer a longer therapeutic horizon, acting days after stroke onset.
A New Chapter in Neurorehabilitation
The findings could transform not just how we treat stroke, but how we think about recovery. Instead of passively waiting for the brain to heal—or accepting irreversible damage—doctors might someday use medications to actively retrain the brain’s immune system.
The team’s next goal is to develop therapies that can operate beyond the acute phase of stroke. This means crafting strategies that work days or even weeks later, targeting glial cells like microglia to rebuild neural circuits, preserve brain function, and enhance rehabilitation outcomes.
In a world where stroke survivors often face a lifetime of disability, even modest improvements in recovery could transform millions of lives.
Hope Beyond Stroke
The implications ripple far beyond stroke. Microglial dysfunction has been implicated in diseases ranging from Alzheimer’s to multiple sclerosis and traumatic brain injury. If HDACi drugs can safely and effectively recalibrate microglia, they could become a cornerstone of future neurotherapies.
Still, challenges remain. Translating laboratory findings to human treatment requires careful clinical trials, safety evaluations, and long-term studies. Yet the momentum is clear. The door is now open to a future in which the brain’s own immune cells are not the enemies of recovery, but its architects.
“This is about more than just treating stroke,” said Prof Dheen. “It’s about changing how we harness the power of the brain’s own biology to heal itself.”
A Future Worth Fighting For
As scientists push forward, the promise of HDACi therapy reminds us that medical revolutions often come not from new inventions, but from seeing old tools in new ways. In the quiet, microscopic dance of genes and immune cells, hope is being rewritten—one brain at a time.
Stroke may strike swiftly and cruelly, but science is catching up. And thanks to the brilliant minds at NUS Medicine and their partners, a new story is being written—one where healing begins not with the clock, but with the cells that call the brain home.
Reference: Kevin Jayaraj et al, Spatial Transcriptomic Analysis Reveals HDAC Inhibition Modulates Microglial Dynamics to Protect Against Ischemic Stroke in Mice, Glia (2025). DOI: 10.1002/glia.70035