Imagine a storm brewing inside your head—a storm so powerful it can shut down your day, distort your senses, and make even the simplest sounds or beams of light feel unbearable. This is the reality of a migraine. Unlike ordinary headaches, migraines are complex neurological events that can affect the entire body, not just the head. They are unpredictable, often invisible to others, and deeply personal to those who endure them.
Migraines affect over one billion people worldwide, making them one of the most common—and most disabling—neurological conditions. Yet, despite their prevalence, migraines remain misunderstood. They are sometimes dismissed as “just bad headaches,” but in truth, they are a profound disorder of the nervous system that impacts quality of life, productivity, relationships, and emotional well-being.
To understand migraines fully, we must explore their causes, symptoms, diagnosis, and treatments through both the lens of science and the lived experience of those who face them.
What is a Migraine?
A migraine is a neurological condition characterized by recurrent episodes of intense, throbbing head pain, often accompanied by nausea, vomiting, and extreme sensitivity to light, sound, or smells. Migraines can last anywhere from a few hours to several days, and they often follow a recognizable pattern or cycle.
Migraines are more than “head pain.” They represent a dysfunction in the brain’s electrical and chemical signaling. The attacks can be so severe that they interfere with daily activities, forcing sufferers to retreat into dark, quiet rooms until the storm passes.
Unlike tension headaches or sinus headaches, migraines are often one-sided, pulsating, and disabling. They may also present with neurological disturbances called auras, which can include visual distortions, numbness, or difficulty speaking.
The Science of Migraine: What Causes It?
For decades, scientists believed migraines were simply vascular headaches caused by changes in blood flow to the brain. While blood vessels do play a role, modern research has revealed a more complex picture: migraines are primarily neurological, involving the brain’s networks of neurons, neurotransmitters, and sensory processing systems.
Genetic Predisposition
Migraines often run in families, suggesting a strong genetic component. If one parent has migraines, their child has about a 40% chance of developing them; if both parents do, the risk rises to 75%. Genome studies have identified several gene variations linked to migraines, particularly those that affect how the brain regulates pain and sensory input.
Neurological Triggers
Migraines begin in the brainstem and involve abnormal interactions between nerves and blood vessels. The trigeminal nerve—a major pain pathway in the face and head—becomes activated, releasing inflammatory substances that irritate blood vessels and amplify pain signals.
Another key player is serotonin, a neurotransmitter that helps regulate pain, mood, and blood vessel function. During a migraine, serotonin levels drop, which may trigger dilation of blood vessels and increased pain sensitivity.
Cortical Spreading Depression
Some migraines, especially those with aura, are thought to result from a phenomenon called cortical spreading depression—a wave of electrical activity that sweeps across the brain’s surface. This wave disrupts normal brain function, causing visual distortions, numbness, or speech difficulties.
Environmental and Lifestyle Triggers
While genetics set the stage, environmental and lifestyle factors often trigger the actual migraine attack. Common triggers include:
- Stress: Emotional or physical stress is one of the leading migraine triggers.
- Sleep disturbances: Too little or too much sleep can provoke attacks.
- Dietary factors: Certain foods and drinks—aged cheese, processed meats, red wine, caffeine, and artificial sweeteners—can act as triggers.
- Hormonal changes: Many women experience migraines linked to menstrual cycles, pregnancy, or menopause.
- Sensory overload: Bright lights, loud noises, strong smells, or screen time can set off migraines.
- Weather changes: Shifts in barometric pressure, humidity, or temperature are known to spark attacks.
Symptoms of Migraine
Migraine symptoms are diverse and can vary widely from person to person. However, most migraines progress through four distinct stages, though not everyone experiences them all.
1. Prodrome (Early Warning Signs)
Hours or even days before the migraine strikes, subtle changes may signal its approach. These include:
- Irritability or mood swings
- Cravings for certain foods
- Stiffness in the neck
- Fatigue or frequent yawning
- Constipation or diarrhea
These early warning signs give some people the opportunity to take preventive measures before the full-blown migraine begins.
2. Aura (Neurological Disturbances)
About 25–30% of migraine sufferers experience an aura, which typically lasts 20–60 minutes. Auras can affect vision, speech, or sensation, and include:
- Visual symptoms: flashing lights, zigzag patterns, blind spots, tunnel vision
- Sensory symptoms: tingling or numbness in the face or hands
- Speech disturbances: difficulty finding words or slurred speech
- Motor symptoms (rare): temporary weakness on one side of the body
Aura symptoms can be alarming, sometimes mimicking stroke. However, they are usually reversible and fade before the headache phase.
3. Attack (Headache Phase)
The hallmark of migraine is the attack phase, which can last from 4 to 72 hours if untreated. Symptoms include:
- Intense, throbbing or pulsating head pain (often on one side)
- Pain that worsens with movement
- Sensitivity to light (photophobia), sound (phonophobia), or smells (osmophobia)
- Nausea and vomiting
- Blurred vision
- Lightheadedness or fainting in severe cases
4. Postdrome (Recovery Phase)
After the pain subsides, many people feel drained, weak, or mentally foggy—a state often called the “migraine hangover.” This phase can last up to a day and may include:
- Difficulty concentrating
- Fatigue
- Mood changes
- Sensitivity to light and sound
Diagnosis of Migraine
Because migraines share symptoms with other conditions, diagnosis requires careful evaluation. There is no single test for migraines; instead, doctors rely on medical history, symptom patterns, and ruling out other causes.
Medical History
Doctors typically begin by asking about:
- Frequency and duration of headaches
- Location and type of pain
- Associated symptoms (nausea, aura, sensitivity to light/sound)
- Family history of migraines
- Potential triggers (diet, stress, sleep, hormones)
Keeping a headache diary can be invaluable, recording when attacks occur, what precedes them, and how they progress.
Neurological Examination
A neurological exam helps ensure that the headaches are not caused by another condition such as a brain tumor, stroke, or infection. Doctors check reflexes, muscle strength, coordination, and sensory function.
Diagnostic Criteria
According to the International Classification of Headache Disorders (ICHD-3), a migraine diagnosis typically requires:
- At least five attacks
- Lasting 4–72 hours untreated
- At least two of the following: unilateral pain, pulsating quality, moderate-to-severe intensity, worsening with activity
- Accompanied by nausea/vomiting or sensitivity to light/sound
Imaging Tests
In some cases, MRI or CT scans may be ordered to rule out structural brain abnormalities. However, these are usually normal in people with migraines.
Treatment of Migraine
There is no universal cure for migraines, but treatments aim to reduce symptoms, shorten attacks, and prevent recurrence. Successful management often requires a combination of medications, lifestyle changes, and complementary therapies.
Acute Treatments (Stopping an Attack)
Acute treatments are taken at the first sign of a migraine to reduce intensity and duration. Options include:
- Over-the-counter pain relievers: aspirin, ibuprofen, or acetaminophen (best for mild attacks)
- Triptans: prescription drugs (such as sumatriptan, rizatriptan) that target serotonin receptors to narrow blood vessels and block pain pathways
- Ergotamines: older drugs effective for some, but with more side effects
- Anti-nausea medications: metoclopramide or prochlorperazine, especially useful when vomiting accompanies migraine
- Ditans and gepants: newer drug classes that act on specific migraine pathways without vascular side effects, helpful for those who cannot take triptans
Preventive Treatments (Reducing Frequency)
For people with frequent or severe migraines, preventive strategies may be recommended:
- Medications:
- Beta-blockers (propranolol, metoprolol)
- Antidepressants (amitriptyline, venlafaxine)
- Anticonvulsants (topiramate, valproate)
- CGRP monoclonal antibodies (erenumab, fremanezumab) – targeted therapies blocking migraine-specific pathways
- Lifestyle approaches:
- Regular sleep and meal patterns
- Stress management (meditation, yoga, biofeedback)
- Avoidance of known triggers
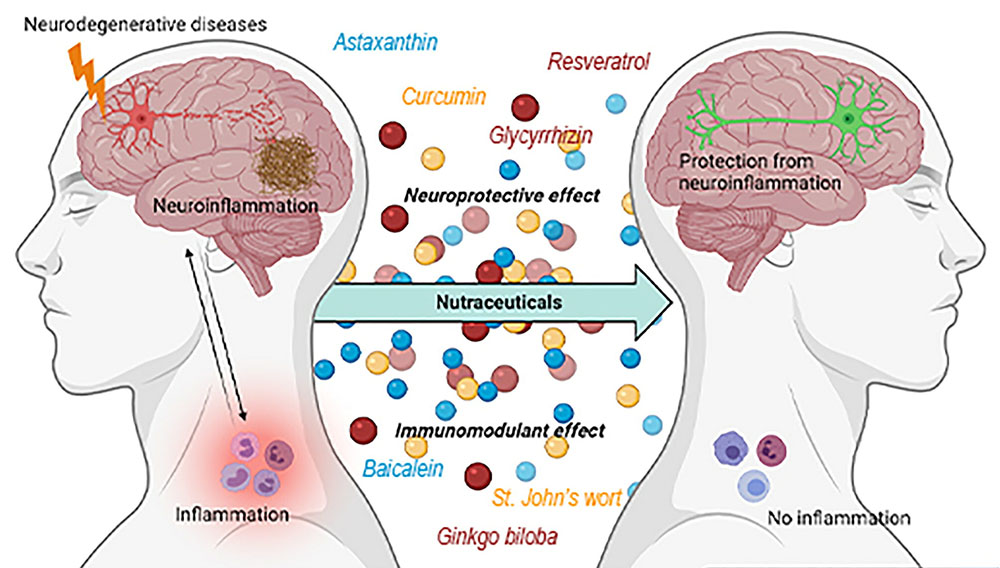
Non-Drug Therapies
Some patients find relief through complementary approaches:
- Acupuncture: shown to reduce frequency in some studies
- Cognitive behavioral therapy (CBT): helps manage stress and pain perception
- Supplements: magnesium, riboflavin (Vitamin B2), and coenzyme Q10 show promise for prevention
- Neuromodulation devices: wearable devices that stimulate nerves using electrical or magnetic impulses
Emergency Treatments
For severe migraines unresponsive to standard treatment, hospitalization may be necessary. Intravenous fluids, antiemetics, or strong pain medications can provide relief.
Living with Migraine: Beyond Medication
Migraine is not just a medical condition; it is a life condition. People who live with migraines must constantly balance daily activities with the risk of triggering an attack. The unpredictability can cause anxiety, missed work or school, and social isolation.
Support systems—family, friends, employers—play a crucial role in helping individuals manage this invisible illness. Advocacy and education are equally important, as greater awareness reduces stigma and ensures sufferers receive the empathy and accommodations they deserve.
Self-care is also vital. Identifying triggers, practicing relaxation techniques, staying hydrated, and maintaining healthy routines can make a significant difference.
When to Seek Medical Help
While many people manage migraines with over-the-counter drugs, professional medical evaluation is essential if:
- Headaches are frequent or disabling
- Headaches are sudden and severe (worst ever experienced)
- Symptoms include neurological changes (weakness, confusion, vision loss)
- Headaches change in pattern or intensity
Such symptoms could indicate a more serious condition requiring immediate medical attention.
The Future of Migraine Treatment
Research into migraines is advancing rapidly. Scientists are exploring:
- Genetic therapies to correct underlying predispositions
- Personalized medicine based on genetic and lifestyle profiles
- New drug classes targeting molecular pathways such as CGRP (calcitonin gene-related peptide)
- Digital health tools including smartphone apps for monitoring and predicting attacks
With growing awareness and scientific innovation, the future looks promising for more effective, targeted, and compassionate care for migraine sufferers.
Conclusion: Navigating the Storm
A migraine is more than a headache—it is a neurological storm that can hijack the body and mind. Yet, understanding its causes, recognizing its symptoms, and accessing effective treatments can transform the experience from one of helplessness to one of control.
Science continues to unravel the mysteries of this condition, offering new hope to millions who live with its shadow. But even today, with careful management, lifestyle adjustments, and support, people with migraines can lead vibrant, fulfilling lives.
Migraine may be a storm, but with the right knowledge and tools, it does not have to define the horizon.