Every cell in the human body hums with life, carrying out the tasks that sustain our existence. At the heart of this orchestra is a language not spoken in words, but in shapes—proteins folded into precise structures, each a tiny marvel of biology. Proteins are the workhorses of the cell, ferrying messages, catalyzing reactions, building frameworks, and enforcing order. But what happens when these proteins lose their shape?
In recent years, scientists have begun to connect the dots between misfolded proteins and a range of age-related diseases. From cancer to cardiovascular disorders and type 2 diabetes, a troubling pattern has emerged: where there is chronic disease, there is often a failure in the machinery that ensures proteins fold correctly. Like a symphony gone out of tune, this silent disruption can lead to cellular chaos and, ultimately, to the breakdown of entire organ systems.
The Vulnerable Heart of the Pancreas
Among the most delicate and critical cells in the body are the insulin-producing β-cells of the pancreas, nestled in small clusters known as islets. These cells are responsible for releasing insulin, a hormone that allows the body to lower blood sugar levels by signaling cells to absorb glucose. Alongside insulin, β-cells also produce another protein—amylin—that plays a supporting role by regulating satiety after meals.
For people with type 2 diabetes, these β-cells become dysfunctional and die over time. For decades, researchers believed that the main source of stress in these cells came from the endoplasmic reticulum (ER)—a cellular factory responsible for synthesizing and trafficking proteins. Misfolded proteins in the ER were thought to trigger a cascade of stress responses that ultimately led to cell death. But a groundbreaking study from the University of Michigan has now revealed that this is only part of the story.
The Mitochondrial Mystery
In a study published in Nature Metabolism, researchers discovered that the mitochondria, often called the powerhouses of the cell, are also deeply involved in the protein misfolding crisis. This was an unexpected twist. Mitochondria were long known for their role in generating energy through oxidative phosphorylation, but this research revealed that they are also prone to the dangerous accumulation of misfolded proteins in the context of type 2 diabetes.
And this accumulation isn’t benign. It appears to be deadly.
Misfolded proteins in the mitochondria disrupt energy production, weaken the cell’s resilience, and ultimately drive the demise of β-cells. As these critical insulin-producing cells die off, the body loses its ability to regulate glucose, and blood sugar levels spiral out of control. What begins as a cellular housekeeping issue ends in systemic disease.
Cracks in the Cell’s Defense System
The researchers set out to investigate why β-cells in diabetic individuals are so susceptible to misfolded proteins. They turned their attention to a specific mitochondrial protein called LONP1—a molecular custodian tasked with identifying and degrading damaged or misfolded proteins within the mitochondria.
What they found was striking.
In pancreatic β-cells from individuals with type 2 diabetes, LONP1 was significantly reduced. Without this crucial component of the cellular quality control system, misfolded proteins accumulated unchecked. The cells, unable to cope with the rising burden of dysfunction, initiated self-destruct mechanisms. The study marks the first time LONP1 has been implicated in common metabolic diseases like diabetes, although it was previously linked to rare mitochondrial disorders.
The absence of LONP1 didn’t just correlate with disease—it seemed to cause it. Mice engineered to lack LONP1 developed high blood glucose levels and had far fewer β-cells than their healthy counterparts. When researchers reintroduced LONP1 into these mice, their blood sugar levels normalized and β-cell numbers improved.
The Hidden Parallel to Alzheimer’s
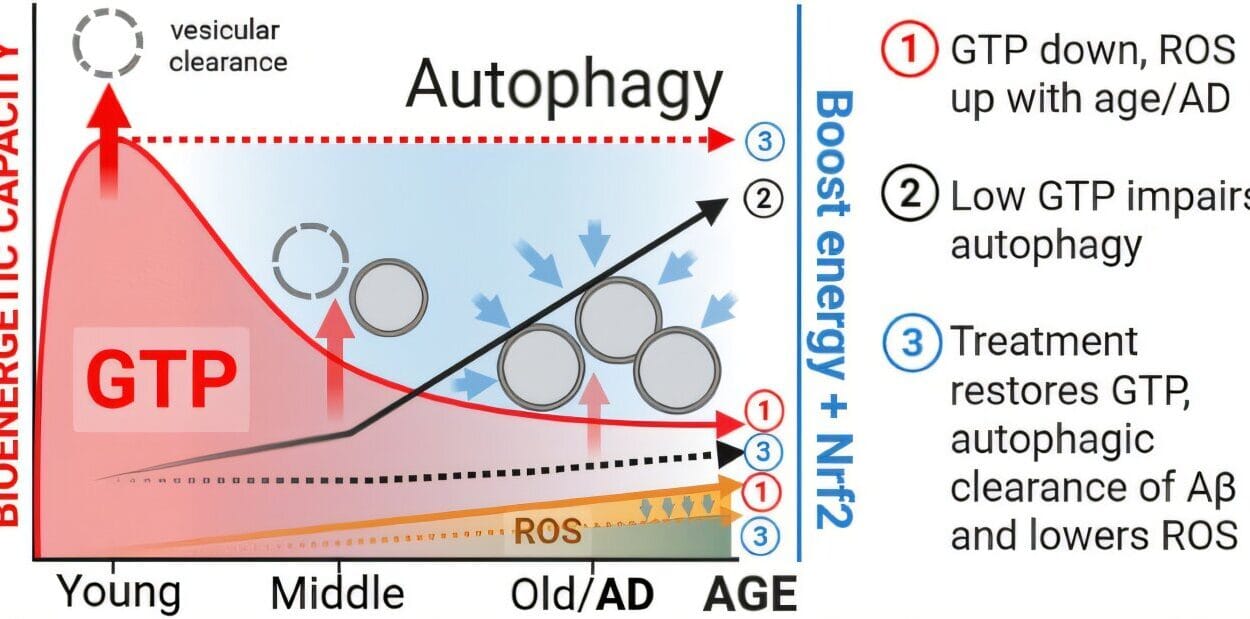
Perhaps even more fascinating is the parallel drawn between the protein misfolding seen in diabetic β-cells and that observed in neurodegenerative diseases like Alzheimer’s. In both conditions, amyloid aggregates are a key pathological hallmark. In Alzheimer’s, amyloid-beta forms sticky plaques in the brain. In type 2 diabetes, the culprit is amylin, which accumulates and clumps into amyloid structures within β-cells.
These toxic aggregates disrupt normal cell function, trigger inflammation, and can set off cell death. The resemblance is more than superficial. It suggests a common thread—one in which aging, protein misfolding, and impaired cellular clean-up mechanisms converge to drive multiple forms of chronic disease.
Unbiased Discovery, Revolutionary Insights
Until recently, most research had focused exclusively on insulin and amylin as the misfolded villains within β-cells. But the Michigan researchers, led by Dr. Scott Soleimanpour, took a different path. They opted for an unbiased, comprehensive analysis, using advanced gene and protein sequencing tools to examine all the proteins expressed in both healthy and diabetic β-cells.
Their goal was not to confirm old assumptions, but to uncover new truths.
What they found was a sprawling network of misfolded proteins in diabetic cells—far beyond just insulin and amylin. Many of these misfolded proteins were linked to mitochondrial function, revealing a much larger, systemic breakdown of protein quality control than previously understood. The study has cracked open a new frontier in diabetes research, shifting focus from insulin deficiency to cellular failure at the proteomic level.
Implications for Treatment and Hope for Reversal
The implications of this research are profound. If misfolded proteins are a root cause of β-cell death in type 2 diabetes, then therapies aimed at restoring protein homeostasis—especially within mitochondria—could be transformative.
Restoring LONP1 function is one promising avenue. In the mice studies, the return of LONP1 reversed many of the diabetic traits. It suggests that even once β-cells begin to falter, there may be hope for recovery if the stress burden can be reduced. This goes against the long-held belief that β-cell loss in diabetes is irreversible.
Moreover, if scientists can develop drugs that either help misfolded proteins refold correctly or accelerate their removal, it may be possible to halt the progression of the disease entirely. Such treatments would not merely manage blood sugar—they would treat the underlying cause, potentially restoring normal insulin production.
A Disease of Time and Accumulation
Type 2 diabetes doesn’t strike overnight. It creeps in, building slowly, year after year. Dr. Soleimanpour and his team believe that the gradual accumulation of misfolded proteins may be a key factor in this progression. Early in life, cellular quality control systems function well. Misfolded proteins are swiftly eliminated, and β-cells remain healthy.
But as time goes on, and especially as people age, these defenses begin to falter. Misfolded proteins slip through the cracks. They start to pile up, creating stress, inflammation, and dysfunction. Eventually, the burden becomes too great. The β-cells, exhausted and overwhelmed, begin to die.
This understanding transforms how we view type 2 diabetes. It is not merely a lifestyle disease, nor is it solely a genetic fate. It is a biological tipping point, where the delicate balance between protein synthesis, folding, and degradation is lost. And with it, so is the body’s ability to regulate its most vital fuel: glucose.
The Promise of Early Intervention
Knowing that protein misfolding and mitochondrial dysfunction may precede overt diabetes opens the door to early intervention strategies. Imagine a future where blood tests can detect early signs of proteotoxic stress in pancreatic cells—long before blood sugar begins to rise. Such a test could prompt preventative treatment, much like cholesterol screenings are used to prevent heart disease today.
This research also underscores the importance of aging biology in the pathogenesis of chronic diseases. It suggests that interventions targeting mitochondrial health—such as certain antioxidants, metabolic therapies, or caloric restriction mimetics—could not only delay the onset of type 2 diabetes but possibly other age-associated diseases as well.
The Next Chapter: Healing from Within
The human body has remarkable powers of adaptation and regeneration. What this study from the University of Michigan shows is that even cells on the brink of death—cells once thought to be beyond repair—might be coaxed back to health if their internal environment can be restored.
It offers a new narrative for type 2 diabetes, one that moves beyond pills and injections toward a deeper understanding of the molecular and cellular breakdowns at its core. It offers hope that we are not helpless against this rising tide of chronic illness.
Science, at its best, not only explains but heals.
And in the misfolded strands of a single protein, we may have found a new path forward—not just for diabetes, but for the wider question of how to grow old without breaking down.
Reference: Jin Li et al, LONP1 regulation of mitochondrial protein folding provides insight into beta cell failure in type 2 diabetes, Nature Metabolism (2025). DOI: 10.1038/s42255-025-01333-7