Inside every living cell lies a remarkable molecule—DNA. This intricate double helix carries the full set of instructions for building and maintaining life, written in a language of four chemical letters: A (adenine), T (thymine), C (cytosine), and G (guanine). Arranged in sequences forming genes, this code tells a cell how to make proteins, the molecular machines that carry out nearly every function in the body. These proteins control everything—from the color of our eyes to how our bodies respond to infections.
Yet, despite the precision of this molecular system, the code is not invincible. DNA is constantly being copied, repaired, exposed to environmental stressors, and bombarded by internal chemicals. And sometimes, through accident or influence, mistakes creep in. These mistakes—mutations—are like typographical errors in a critical instruction manual. Some are harmless, even beneficial. Others, however, can cause cells to go awry, unraveling the normal balance of life and triggering disease.
Understanding how mutations arise, how they affect cells, and why they sometimes lead to illness is one of the most fundamental quests in biology and medicine. It is a story that connects the deep mechanics of cellular life with the human experience of health and suffering.
What Is a Mutation?
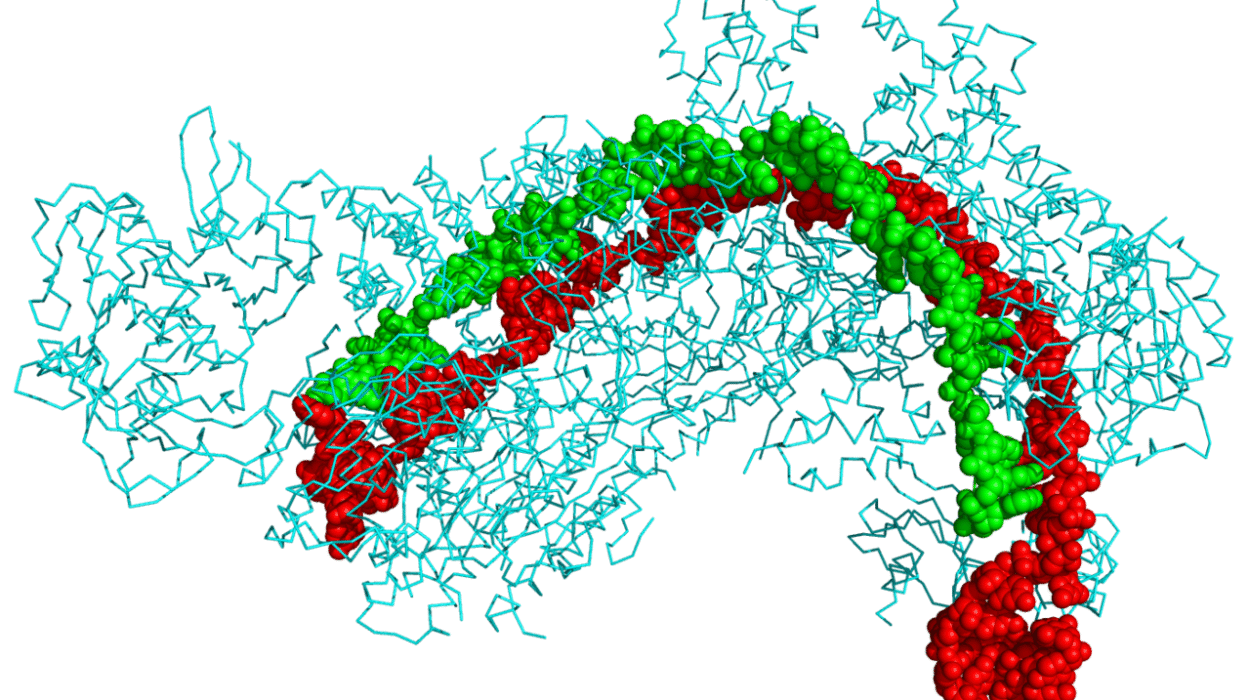
To grasp the impact of mutations, we must first understand what they are. A mutation is a permanent change in the DNA sequence of a gene. These changes can be as small as a single letter switched for another—called a point mutation—or as large as entire sections of a chromosome being deleted, duplicated, or rearranged.
Mutations can occur in many ways. Some are spontaneous, emerging from errors in DNA replication when a cell divides. Despite the cell’s advanced proofreading systems, tiny flaws occasionally escape correction. Other mutations are caused by external factors—radiation, chemicals, or viruses—that damage DNA directly. Even normal cellular metabolism generates by-products like reactive oxygen species, which can harm the genome over time.
When a mutation arises, its effect depends largely on where it occurs and how it alters the gene. A mutation in a non-coding region may have no impact at all. But a mutation within a gene that codes for an essential protein may cause the resulting protein to fold incorrectly, lose its function, or behave abnormally—sometimes with devastating consequences.
The Ripple Effect Within the Cell
A mutated gene may produce a protein that is dysfunctional, absent, or hyperactive. Because proteins are at the heart of every cellular process, even a small change can ripple outward to affect the entire cell.
Consider the enzyme hexosaminidase A, essential for breaking down certain fatty molecules in the brain. In Tay-Sachs disease, a single mutation in the gene that encodes this enzyme leads to its malfunction. As a result, fatty substances accumulate in neurons, eventually destroying them. The effect begins subtly—perhaps missed developmental milestones in a child—but within a few years, the damage becomes profound and irreversible.
In another case, mutations in the gene CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) alter a channel that regulates the movement of salt and water in and out of cells. This leads to thick, sticky mucus in the lungs and pancreas, characteristic of cystic fibrosis. The cellular disruption may begin in early development, but the disease manifests as chronic infections, digestive problems, and progressive respiratory failure.
Such examples show how a microscopic change in DNA can alter the fate of an entire cell—and in turn, the fate of a person.
From Mutated Cells to Disease
Mutations don’t always cause disease, but when they do, it’s often because they disrupt a finely tuned balance within the cell. Sometimes, the cell responds by triggering apoptosis—programmed cell death—to prevent further harm. This self-destruct mechanism is a powerful fail-safe. But if a cell with a dangerous mutation bypasses apoptosis and continues dividing, it can become the seed of a disease.
In cancer, for instance, mutations accumulate in genes that regulate the cell cycle, repair DNA, or control cell death. The tumor suppressor gene TP53 is frequently mutated in cancers. Its normal function is to detect DNA damage and halt cell division, giving the cell time to repair itself. If the damage is too great, TP53 triggers cell death. But when TP53 itself is mutated, this protective mechanism fails. Cells divide uncontrollably, leading to tumor growth.
Another example is sickle cell anemia, where a single point mutation in the hemoglobin gene causes red blood cells to deform into a rigid, sickle-like shape. These misshapen cells clog blood vessels, causing pain, organ damage, and anemia. The root of the disease lies in a single amino acid substitution in the hemoglobin protein—a tiny change with massive physiological consequences.
Each disease caused by mutations follows its own trajectory, shaped by the nature of the mutation, the affected gene, and the role of that gene in the body. Sometimes, the damage is isolated. Other times, it sets off a chain reaction that affects multiple systems at once.
Inherited vs. Acquired Mutations
Mutations can be inherited or acquired. Inherited mutations are passed from parent to child and are present in every cell of the body. These mutations are responsible for many genetic disorders, including Huntington’s disease, Marfan syndrome, and Duchenne muscular dystrophy. In some cases, the inheritance pattern is dominant—one copy of the mutated gene is enough to cause the disease. In others, the pattern is recessive—two copies are required.
Acquired mutations, on the other hand, arise during a person’s lifetime. They may occur in a single cell and then spread as that cell divides. These somatic mutations are not passed on to offspring but can lead to diseases such as cancer. In fact, most cancers are the result of acquired mutations, often in combination with inherited risk factors.
The interplay between inherited and acquired mutations is complex. A person may inherit a mutation that predisposes them to cancer, like a BRCA1 mutation, and then acquire additional mutations over time that push a cell toward malignancy. In this way, disease becomes a multi-step process—like a series of falling dominoes—each mutation nudging the cell closer to dysfunction.
Silent, Harmless, and Beneficial Mutations
Not all mutations are harmful. In fact, most mutations are silent—they do not change the amino acid sequence of the protein and have no observable effect. Some mutations occur in non-coding regions of DNA or in ways that are neutral to protein function.
Occasionally, a mutation can even be beneficial. For instance, a mutation that confers resistance to malaria also causes sickle cell trait—a condition in which individuals carry one copy of the sickle cell gene but do not develop the disease. These individuals are less likely to suffer from severe malaria infections, giving them a survival advantage in regions where the disease is endemic.
In rare cases, beneficial mutations can drive evolution, allowing a population to adapt to environmental changes. Over thousands of generations, such mutations contribute to the diversity and resilience of life. The same mechanisms that cause disease, in another context, can be a source of strength.
The Environment as a Mutagen
While some mutations are random, many are influenced by the environment. Ultraviolet (UV) radiation from the sun can cause mutations in skin cells, leading to melanoma. Tobacco smoke contains chemicals that bind to DNA and induce mutations in lung tissue. Industrial pollutants, household chemicals, and even food additives can all contribute to mutational burden.
Viruses also play a role. The human papillomavirus (HPV), for example, can insert its genetic material into host cells, disrupting genes that control the cell cycle. This can lead to cervical and other cancers. Similarly, hepatitis B and C viruses are linked to liver cancer through mechanisms involving chronic inflammation and genetic damage.
Understanding how the environment shapes the mutational landscape of our cells is essential for disease prevention. Public health campaigns, regulatory policies, and education can reduce exposure to harmful mutagens and lower the incidence of mutation-driven diseases.
Cellular Defense: DNA Repair Mechanisms
Thankfully, cells are not defenseless. They are equipped with a sophisticated array of DNA repair mechanisms that detect and fix errors before they cause harm. These include base excision repair, nucleotide excision repair, mismatch repair, and double-strand break repair.
When these systems function properly, they can correct most mutations before they become permanent. But when the repair systems themselves are mutated or overwhelmed, damage accumulates. This is seen in disorders like xeroderma pigmentosum, where a defect in DNA repair enzymes causes extreme sensitivity to sunlight and a high risk of skin cancer.
The ability of a cell to repair DNA is a critical factor in aging and cancer. As we age, repair efficiency declines, and mutations accumulate. Some researchers believe that improving DNA repair could extend lifespan and reduce age-related diseases—a tantalizing possibility still under investigation.
Personalized Medicine: Navigating the Genetic Landscape
In recent years, advances in genomic technology have revolutionized our ability to detect mutations and understand their consequences. Whole genome sequencing can reveal every mutation in a person’s DNA, offering a personalized map of genetic risk.
This information is already transforming medicine. In cancer treatment, for example, tumors are now sequenced to identify specific mutations, allowing doctors to tailor therapy to the molecular profile of the cancer. Drugs like imatinib (Gleevec) target mutated proteins in leukemia, offering precision treatment with fewer side effects.
For inherited diseases, genetic testing can identify carriers and predict disease risk. Prenatal and preimplantation genetic diagnosis offer parents the chance to make informed reproductive decisions. Gene therapy, still in its early stages, holds promise for correcting mutations at the source.
The dream of personalized medicine is to move beyond one-size-fits-all approaches and instead design treatments based on each individual’s unique genetic makeup. This approach brings hope—but also ethical challenges and questions about access, privacy, and equity.
The Future: CRISPR and Gene Editing
Perhaps the most groundbreaking development in mutation research is the advent of CRISPR-Cas9—a gene-editing tool that allows scientists to precisely modify DNA. By cutting out faulty genes and replacing them with healthy ones, CRISPR offers the possibility of curing genetic diseases at their root.
In 2020, scientists used CRISPR to treat sickle cell disease and beta-thalassemia in patients by editing their bone marrow stem cells. Early results were encouraging, raising the prospect of durable, one-time cures. Research is underway to apply similar techniques to muscular dystrophy, cystic fibrosis, and certain cancers.
However, with great power comes great responsibility. The ability to edit human embryos raises profound ethical concerns. Where do we draw the line between therapy and enhancement? Who decides what counts as a “normal” gene? These questions are as much about society as they are about science.
Conclusion: The Fragile Thread of Life
Mutations are a double-edged sword—sources of both disease and diversity, suffering and survival. They remind us that life is inherently fragile, its continuity dependent on the integrity of a code that is constantly under siege.
Yet they also reveal the resilience of biology. Despite the risks, cells endure. Mechanisms of repair, adaptation, and evolution protect life from extinction. And when these defenses fail, science steps in—to understand, to intervene, and, one day, perhaps to heal.
In studying how mutations affect cells and lead to disease, we confront the deepest questions of biology and medicine. But we also glimpse something profoundly human: the yearning to know why things go wrong—and the hope that we might one day make them right.