Every second, your body hosts microscopic dramas of staggering intensity. Cells replicate, immune defenses patrol, and invaders attempt to breach the fortress. Among the most cunning adversaries in this biological battlefield are bacteria—ancient, microscopic organisms that have learned to thrive almost everywhere, from the deep sea to the human gut. When these invaders cross the line between coexistence and harm, causing disease, we turn to one of the most powerful tools modern medicine has ever devised: antibiotics.
Antibiotics are not just chemicals in capsules; they are lifelines, shields, and weapons in the invisible war between humans and microbes. To understand how they work is to open a door into the microscopic theater of war, where strategy, timing, and molecular precision determine who lives and who dies. Their story is one of scientific triumph, evolutionary arms races, and a future that now hangs precariously in the balance.
What Makes Bacteria So Hard to Kill?
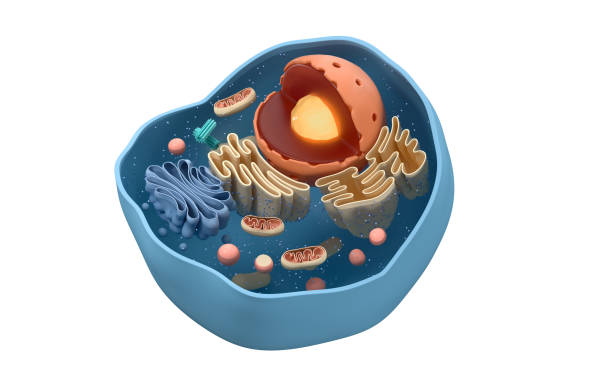
Bacteria are not miniature versions of human cells. They are structurally and genetically different in fundamental ways—and this is precisely what makes antibiotics effective, and selectively so. Unlike viruses, which must hijack a host’s cellular machinery to replicate, bacteria are living, self-sufficient organisms. They contain their own DNA, generate their own energy, and reproduce by themselves, often doubling every 20 minutes under ideal conditions.
They possess a rigid cell wall that maintains their shape, a cell membrane that acts as a gatekeeper, and ribosomes that synthesize proteins essential for survival. Their internal architecture is simple but elegant, honed by billions of years of evolution.
To destroy these organisms without harming human cells, antibiotics must be exquisitely selective. They target the features that make bacteria unique—exploiting their molecular weaknesses like expert marksmen. The precision of this attack is what makes antibiotics both miraculous and dangerous. Miraculous, because they can eliminate infections with minimal harm to us. Dangerous, because misuse fosters resistance, allowing bacteria to adapt and survive even our most potent weapons.
The Birth of a Medical Revolution
The modern antibiotic era began almost accidentally, with the discovery of penicillin by Alexander Fleming in 1928. Returning from vacation, he noticed a mold—Penicillium notatum—had contaminated one of his petri dishes and killed the surrounding Staphylococcus bacteria. Fleming had observed nature’s own microscopic warfare. But the world didn’t pay much attention until World War II, when penicillin was mass-produced and deployed to save soldiers from battlefield infections. What followed was nothing short of a revolution.
Diseases that once ravaged populations—tuberculosis, pneumonia, syphilis, plague—could now be tamed. Life expectancy soared. Surgery became safer. Medical confidence swelled. The 20th century became a golden age of antibiotic discovery. But the magic, it turned out, was not in the drug alone. It was in understanding how it worked.
Crippling the Bacterial Fortress: Attacking the Cell Wall
One of the most elegant strategies antibiotics use is the disruption of the bacterial cell wall. This structure is a rigid, protective shell made of a molecule called peptidoglycan. It’s critical for the bacteria’s survival—especially in hypotonic environments like the human body where osmotic pressure threatens to burst unprotected cells.
Penicillin and its cousins—the beta-lactam antibiotics—target this very weakness. They bind to enzymes called penicillin-binding proteins (PBPs), which are essential for building and repairing the peptidoglycan wall. When PBPs are disabled, bacteria cannot reinforce their walls, leaving them vulnerable to internal pressure. The cell swells, bursts, and dies—a phenomenon known as lysis.
What makes this approach so ingenious is its specificity. Human cells do not have cell walls or PBPs, so beta-lactam antibiotics kill bacteria without harming us. However, not all bacteria fall prey to this tactic. Gram-negative bacteria, with an extra outer membrane, are more resistant. To breach this, scientists developed cephalosporins, carbapenems, and monobactams—each a variation on the beta-lactam theme, designed to outmaneuver bacterial defenses.
Sabotaging the Factory: Inhibiting Protein Synthesis
Bacteria rely on ribosomes—tiny molecular machines—to translate genetic instructions into proteins. These ribosomes are structurally different from those found in human cells. This difference allows another class of antibiotics to work by jamming the gears of the bacterial factory.
Drugs like tetracyclines, macrolides (such as erythromycin), and aminoglycosides (like streptomycin) bind to different parts of the bacterial ribosome, interrupting protein synthesis at various stages. Some stop the ribosome from reading the mRNA blueprint; others prevent new proteins from being released.
When protein production halts, the bacteria can no longer grow, reproduce, or repair themselves. Depending on the drug and dose, the result may be bacteriostatic—stopping bacterial growth—or bactericidal—killing the organism outright.
The beauty of this method lies in its precision: it targets a machinery absent in human cells, minimizing collateral damage. But it is not without side effects. Because mitochondria (our cellular power plants) evolved from ancient bacteria, they share some ribosomal features. This explains why high doses or long-term use of these drugs can sometimes harm human cells.
Starving the Invader: Disrupting Metabolism
Every living cell needs to make essential components to survive—nucleotides for DNA, amino acids for proteins, and folic acid for metabolic reactions. Some antibiotics work by cutting off these supplies.
Sulfonamides, for example, mimic a compound that bacteria need to synthesize folic acid. Because humans get folic acid from their diet and don’t make it themselves, sulfonamides selectively cripple bacteria without affecting us.
This strategy turns the bacteria’s own pathways against them. By inserting molecular look-alikes into critical biosynthetic processes, these drugs act as Trojan horses. The bacteria unknowingly absorb the impostors, and their internal machinery grinds to a halt.
This kind of metabolic sabotage may not kill bacteria immediately, but it prevents them from replicating or mounting an effective response. Over time, the infection weakens, and the immune system finishes the job.
Scrambling the Blueprint: Interfering with DNA and RNA
Some antibiotics go straight to the source: the bacterial genetic code. By interfering with DNA replication or RNA transcription, they effectively scramble the instructions needed for life.
Fluoroquinolones (like ciprofloxacin) inhibit enzymes called DNA gyrase and topoisomerase IV, which are crucial for unwinding DNA during replication. When these enzymes are blocked, the DNA becomes tangled, and the cell can’t divide or repair itself.
Rifampin, another powerful antibiotic, binds to bacterial RNA polymerase—the enzyme responsible for making messenger RNA from DNA. Without mRNA, no proteins can be built. This is particularly effective against Mycobacterium tuberculosis, which causes tuberculosis and has a notoriously tough cell wall.
These DNA- and RNA-targeting antibiotics are potent and fast-acting but come with a higher risk of side effects because they touch the heart of cellular function. They must be used carefully and often in combination with other drugs to prevent resistance.
The Bacterium Fights Back: Resistance Rises
If the story of antibiotics is a tale of triumph, then the rise of antibiotic resistance is its tragic sequel. Bacteria are not passive victims. They evolve quickly—through mutations, gene transfers, and selective pressures—to develop defenses against our attacks.
Some produce enzymes like beta-lactamases, which break down penicillin and its relatives. Others change their PBPs so the drugs can no longer bind. Efflux pumps eject antibiotics before they can act. Biofilms—slimy communities of bacteria—shield themselves with protective barriers.
Horizontal gene transfer allows resistance genes to leap from one bacterium to another, even across species. A single resistant microbe can seed a population of untreatable pathogens in a matter of hours.
The result? Infections that once melted away with a simple pill now linger, worsen, or kill. Methicillin-resistant Staphylococcus aureus (MRSA), multidrug-resistant tuberculosis (MDR-TB), and carbapenem-resistant Enterobacteriaceae (CRE) are just a few examples of this growing threat.
Human Errors and the Collapse of Efficacy
Resistance doesn’t arise in a vacuum. It is fueled by human behavior—overprescribing, incomplete courses, agricultural misuse, and global misuse of antibiotics. Each unnecessary dose is an evolutionary training session for bacteria. Each incomplete regimen gives survivors a second chance.
In some countries, antibiotics are available without prescription. In others, they’re used prophylactically in livestock, seeping into the environment and selecting for resistant strains. Hospitals, once bastions of healing, have become breeding grounds for superbugs.
And new antibiotics? They’re scarce. Pharmaceutical companies often avoid antibiotic development—it’s costly, time-consuming, and offers poor returns compared to chronic disease drugs. So while resistance spreads like wildfire, the pipeline of new treatments runs dry.
When Antibiotics Don’t Work: The Human Cost
Imagine a world where minor cuts can lead to deadly infections, where routine surgeries become life-threatening, and where childbirth carries a high risk of sepsis. That world existed before antibiotics—and it threatens to return.
Already, drug-resistant infections kill over a million people worldwide each year. Without action, that number could rise to 10 million by 2050. The costs are not just measured in lives, but in economic strain, healthcare burdens, and social disruption.
For patients, the consequences are devastating. Longer hospital stays. Toxic alternative treatments. Fear and uncertainty. For doctors, the challenge is daunting: fighting a shape-shifting enemy with an aging arsenal.
And yet, all is not lost.
The Future of Antibiotics: Innovation and Hope
Scientists around the world are racing to find new antibiotics and novel ways to use them. Some are mining the genomes of soil bacteria and marine organisms. Others are using AI to discover new molecules or repurpose old ones. Phage therapy—using viruses that infect bacteria—is being revisited with modern tools. CRISPR technology may allow us to precisely target and disable resistant bacteria without harming the rest of the microbiome.
Smart drug delivery systems could increase efficacy while reducing side effects. Combination therapies may prevent resistance by hitting bacteria from multiple angles. And rapid diagnostics could help doctors choose the right antibiotic, at the right dose, for the right duration.
But technology alone isn’t enough. Public health initiatives must promote responsible antibiotic use. Education, stewardship programs, and global cooperation are essential. The battle against resistance is not one we can fight in isolation.
Antibiotics and the Microbiome: A Delicate Balance
In our urgency to kill harmful bacteria, we sometimes forget the beneficial ones. The human body contains trillions of microbes that aid digestion, regulate immunity, and even influence mood. Antibiotics often kill indiscriminately, disrupting this delicate ecosystem.
Broad-spectrum antibiotics can decimate gut flora, leading to issues like diarrhea, yeast infections, and even long-term metabolic or autoimmune consequences. Clostridioides difficile, a bacteria that causes life-threatening colitis, often emerges after antibiotic treatment wipes out its competitors.
This has sparked interest in “narrow-spectrum” antibiotics—drugs that target specific pathogens while sparing the microbiome. Probiotics, fecal transplants, and microbiome-friendly therapies are gaining attention as ways to restore microbial balance after treatment.
Understanding how antibiotics affect the whole system—not just the invader—is part of the new frontier in precision medicine.
A Moral and Scientific Responsibility
Antibiotics are not just medications. They are trust—placed in scientists, doctors, and systems to use wisely. The miracle they offer comes with a mandate: to protect what we have, to use only what we need, and to invest in the future.
Each time we use antibiotics recklessly, we weaken their power. Each time we educate, regulate, and innovate, we extend their lifespan. The microbes will never stop evolving. But neither will we.
Conclusion: Guardians of a Microscopic Frontier
From a moldy petri dish to the most advanced synthetic molecules, the journey of antibiotics is one of science at its most human: driven by curiosity, sharpened by necessity, and guided by hope. They have turned the tide of countless infections, bought time for our immune systems, and allowed modern medicine to flourish.
But they are not invincible. Bacteria are relentless, creative survivors. We must be equally relentless in preserving our edge—not through fear, but through responsibility and imagination.
The war inside us continues, unseen but unyielding. How it ends—or whether it ever does—depends on what we do next.