High blood pressure, or hypertension, is often called the “silent killer.” It creeps through the bloodstream with no warnings, no red lights, no obvious alarms. It doesn’t cause pain. You can’t see it or feel it. And yet it damages the body every minute it’s left unchecked. Like a quiet tide slowly eroding the foundation of a cliff, it wears down the arteries, the heart, the brain, the kidneys—until, one day, the damage is no longer invisible.
Worldwide, more than 1.2 billion people are living with high blood pressure. In the United States alone, nearly half of adults have it, often without knowing. But this is not just a statistic—it’s a global health crisis. And it’s deeply personal. Every person with uncontrolled hypertension faces a higher risk of stroke, heart attack, kidney failure, and premature death. Yet despite how common and serious it is, high blood pressure remains misunderstood and often overlooked.
To truly confront this threat, we must understand it from the inside out: how it begins, why it escalates, and what we can do—individually and collectively—to push back.
What Blood Pressure Really Means
Your blood pressure is the force of blood pushing against the walls of your arteries. It rises and falls with each heartbeat. Measured in millimeters of mercury (mmHg), it’s recorded as two numbers: systolic over diastolic. The systolic pressure (the top number) represents the pressure when the heart beats, while the diastolic (the bottom number) reflects the pressure between beats, when the heart is at rest.
A normal reading hovers around 120/80 mmHg. But as that number climbs—whether gradually or suddenly—the risks multiply. At 130/80 mmHg, the American Heart Association considers it Stage 1 hypertension. By 140/90 mmHg, it’s considered more serious. Above that, the danger grows exponentially.
Unlike a fever or a cough, elevated blood pressure doesn’t usually cause discomfort. That’s part of what makes it so dangerous. Most people discover they have it during a routine medical exam—or after a devastating event like a heart attack or stroke.
The Roots Beneath the Surface
What causes blood pressure to rise? There is no single villain. Rather, hypertension arises from a complex interplay of biology, environment, lifestyle, and sometimes simple fate. For some, it’s genetic. A family history of high blood pressure can double the risk. For others, it’s environmental or behavioral—tied to diet, stress, or inactivity.
The arteries play a central role. In a healthy person, these vessels are flexible and elastic, expanding and contracting with each heartbeat. But with age, smoking, poor diet, or chronic stress, they can become narrower and stiffer. This forces the heart to work harder to pump blood through the body. Over time, this strain can lead to a consistent rise in pressure.
Salt is another key factor. Sodium causes the body to retain water, increasing blood volume and pressure. Most people consume far more salt than necessary, often hidden in processed and restaurant foods. When salt intake rises and potassium—found in fruits and vegetables—falls, the balance tips toward hypertension.
Obesity also plays a powerful role. Excess weight forces the heart to supply blood to more tissue. The resulting increase in blood volume raises pressure on artery walls. At the same time, obesity is closely linked to insulin resistance, inflammation, and hormonal imbalances—all of which further increase blood pressure.
But even lean people can develop hypertension. Chronic stress, poor sleep, smoking, alcohol consumption, and certain medications can all interfere with blood pressure regulation. In rare cases, hypertension stems from underlying diseases like kidney disorders or endocrine problems.
When Pressure Turns to Peril
It’s easy to underestimate the power of numbers. A small elevation in blood pressure might not feel like a big deal. But over time, these subtle changes add up to enormous consequences. High blood pressure damages the blood vessels from the inside out. Tiny tears form in the artery walls. The body responds by sending in repair crews of cholesterol and cells—leading to plaque formation. This process, called atherosclerosis, narrows the arteries and stiffens them even more, creating a vicious cycle.
As the arteries narrow, the heart must pump harder. Eventually, the heart muscle thickens and stiffens, a condition known as left ventricular hypertrophy. The heart becomes less efficient and more prone to failure.
High blood pressure is the single most important risk factor for strokes. When pressure gets too high, a vessel in the brain can burst—or a clot can block a narrowed artery—cutting off oxygen and causing part of the brain to die. In some cases, the damage is mild. In others, it’s catastrophic: paralysis, speech loss, cognitive decline, or death.
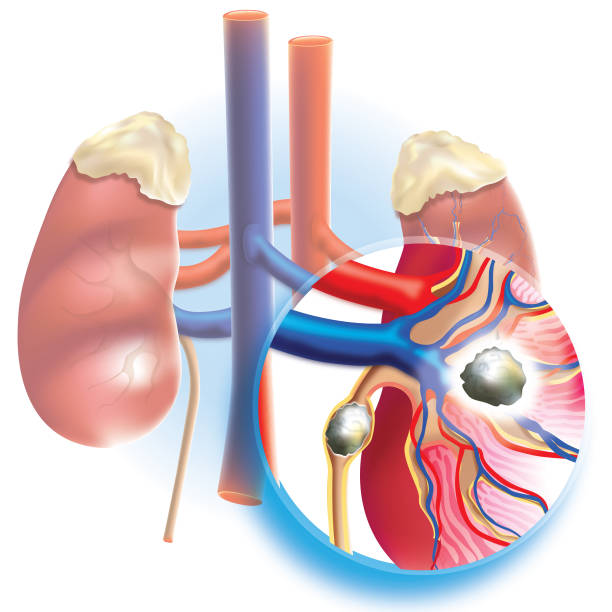
The kidneys are also vulnerable. These vital organs filter waste from the blood, but their delicate vessels can’t withstand prolonged pressure. Over time, kidney function deteriorates, and in many cases, chronic kidney disease leads to dialysis or transplant.
The eyes, too, suffer. Hypertension can cause retinopathy—damage to the blood vessels in the retina—leading to blurred vision or even blindness. And the brain is not immune to the slower effects. Studies increasingly show that uncontrolled hypertension is linked to cognitive decline, memory loss, and dementia.
The bottom line is chilling: high blood pressure is not just about the heart. It’s a full-body, full-life threat.
A Wake-Up Call at Any Age
Once seen as a condition of the old, hypertension is now affecting younger populations at alarming rates. In part, this is due to rising obesity and sedentary lifestyles. But it also reflects growing stress, sleep deprivation, and poor diet. Young adults who assume they’re too young for heart problems may ignore early signs—or never get checked at all.
Pregnancy can also be a time of increased risk. Hypertensive disorders of pregnancy—including gestational hypertension and preeclampsia—can be dangerous for both mother and child. These conditions not only raise short-term risks during childbirth but also increase the woman’s long-term risk of cardiovascular disease.
Even children are now being diagnosed with high blood pressure. Pediatric hypertension is often tied to obesity but can also result from kidney or hormonal disorders. Early detection is crucial, yet many schools and pediatric offices still don’t screen regularly.
The reality is simple: hypertension can strike anyone. But awareness remains dangerously low.
A Life of Awareness, Not Fear
The good news is this: hypertension is preventable, treatable, and manageable. The body, when supported, is astonishingly resilient. Even small changes in lifestyle can lead to measurable improvements in blood pressure—and long-term health.
The first step is awareness. Regular monitoring, whether at a doctor’s office or through a home blood pressure cuff, is essential. For people with risk factors—family history, obesity, diabetes, or smoking—this monitoring should begin early. Knowledge is power, and in this case, it can save lives.
Once diagnosed, treatment typically involves a combination of lifestyle changes and medications. Some people resist taking pills, fearing side effects or dependency. But modern blood pressure medications are safer and more effective than ever before, and for many, they’re life-extending tools.
However, lifestyle is the cornerstone. No drug can replace the benefits of a healthy diet, regular exercise, stress reduction, and quality sleep. These changes not only lower blood pressure but also reduce the need for medication over time.
Food as Medicine
What you eat profoundly affects your blood pressure. Diets rich in fruits, vegetables, whole grains, lean protein, and healthy fats can dramatically reduce hypertension risk. The DASH diet—short for Dietary Approaches to Stop Hypertension—is a research-backed eating plan specifically designed for this purpose.
Reducing sodium is critical. The average person consumes more than 3,400 mg of sodium per day—far above the recommended 1,500–2,300 mg. Cutting back means reading labels, avoiding processed foods, and choosing fresh ingredients.
Potassium, on the other hand, helps balance sodium’s effects. Bananas, spinach, beans, avocados, and sweet potatoes are all excellent sources. Magnesium and calcium also play a role in blood pressure regulation, highlighting the importance of a varied, nutrient-dense diet.
And while moderation is key, some foods have been shown to have direct blood pressure-lowering effects. Beetroot juice, garlic, dark chocolate, and hibiscus tea are all supported by science for their vascular benefits.
Movement and the Circulatory Symphony
The human body was made to move. Exercise strengthens the heart, improves vessel elasticity, reduces stress hormones, and helps manage weight. Aerobic activities like walking, swimming, cycling, or dancing can lower systolic blood pressure by up to 10 points—a change as effective as many medications.
Strength training adds additional benefits by improving muscle mass and metabolic health. Even short bursts of movement throughout the day can help. What matters is consistency. For those with busy lives or physical limitations, even ten-minute walks after meals can make a meaningful difference.
Exercise is not just a chore—it’s a conversation with the body. Each heartbeat during activity sends a signal of vitality and resilience. Over time, these signals translate into stronger circulation and lower pressure.
The Role of the Mind in the Heart’s Burden
Stress doesn’t cause high blood pressure directly—but it does fuel the behaviors that do. Chronic tension can lead to overeating, poor sleep, alcohol use, and emotional exhaustion. It can also activate the body’s fight-or-flight system, raising heart rate and constricting blood vessels.
Learning to manage stress is not just about feeling better. It’s about survival. Techniques like mindfulness meditation, yoga, deep breathing, journaling, and cognitive-behavioral therapy have all been shown to reduce blood pressure. Even something as simple as laughter or time in nature can reset the nervous system.
Sleep is equally vital. Poor sleep—whether due to insomnia, sleep apnea, or an irregular schedule—raises cortisol levels and impairs blood pressure regulation. Aim for 7–9 hours of quality sleep, and treat sleep disorders seriously.
The mind-body connection is real, and when we care for the mind, the body follows.
Medication as an Ally, Not an Enemy
For many people, lifestyle changes alone aren’t enough. That’s where medication comes in—not as a failure, but as an ally. Today, there are several classes of drugs used to manage hypertension, each targeting different mechanisms. These include diuretics (which reduce fluid volume), ACE inhibitors (which relax blood vessels), beta-blockers (which slow the heart), and calcium channel blockers (which reduce arterial tension), among others.
Finding the right medication—and the right dose—can take time. Side effects may occur, but with proper monitoring, most people find a regimen that works. The goal isn’t to medicate forever if it’s avoidable, but to use medicine as a bridge toward better long-term health.
What matters most is adherence. High blood pressure doesn’t go away on its own. Skipping medications because “I feel fine” can be fatal. Partnering with a healthcare provider, checking blood pressure regularly, and sticking with the plan are key to success.
A Future Worth Fighting For
Hypertension is not just a personal problem—it’s a public health challenge. Addressing it requires more than individual effort. It requires policy changes, education, food reform, and healthcare access. Schools need to teach nutrition and movement. Cities must be designed for walking, not just driving. Food companies should be held accountable for sodium levels. Health screenings should be free and accessible.
The burden of high blood pressure falls heaviest on marginalized communities—those facing poverty, discrimination, and limited healthcare. Health equity must be at the center of any solution. No one should suffer or die simply because they were born in the wrong ZIP code.
Globally, governments and organizations are waking up to this reality. The World Health Organization has made hypertension control a priority, recognizing that even small reductions in population blood pressure could save millions of lives. But much work remains.
The future depends on awareness, action, and compassion—starting with how we treat our own hearts.
Conclusion: A Pulse Toward Hope
High blood pressure is not destiny. It is not a life sentence. It is a warning—and an invitation. An invitation to slow down, to listen to the rhythm of your own body, to reconnect with health not as a burden, but as a gift.
Each beat of the heart is a reminder: you are alive. And you have the power to protect that life—not just through pills or diets, but through intention. Through movement, joy, rest, connection. Through the everyday choices that seem small but echo loudly inside your arteries.
Let blood pressure not be a number we fear, but a story we understand. A story we write, day by day, with every step, every meal, every breath.
This story is not yet finished. And with knowledge, courage, and love—it ends in strength.