It often begins with a whisper—tightness behind the breastbone, a little fatigue, perhaps a skipped beat. Nothing alarming, you think. You’ve been busy. Stressed. Maybe it’s indigestion. But then one day, it isn’t. The pain sharpens. Breathing shortens. And your life—everything you’ve built, loved, and dreamed—suddenly hangs in the balance. This is the terrifying moment heart disease introduces itself not as a vague future risk, but as a present, visceral reality.
For millions of people around the world, this moment arrives uninvited, often without warning. Heart disease remains the leading cause of death globally, taking more lives than any other condition. Yet it doesn’t need to be. Prevention is not only possible, it is powerful. And even after diagnosis, recovery is not only within reach—it can be a transformation, a rebirth of body, mind, and purpose.
This guide is not a dry instruction manual. It is a map drawn with both science and compassion, illuminating how to protect your heart, restore your health, and live not just longer—but better.
Understanding the Beating Engine of Life
Your heart is a muscular marvel. About the size of your fist, it beats around 100,000 times a day, pumping oxygen-rich blood through nearly 60,000 miles of blood vessels. Every cell in your body depends on this flow to survive. But like any engine, the heart is vulnerable to wear, blockage, and breakdown.
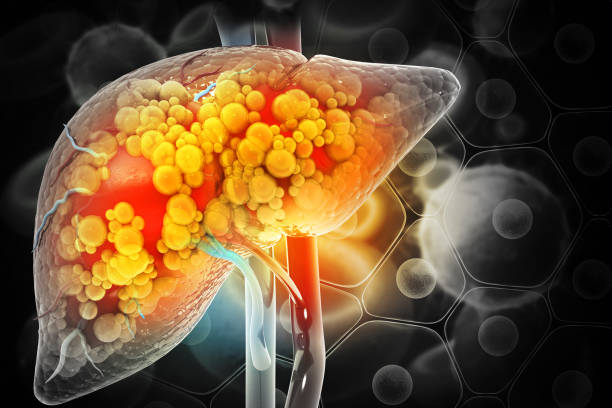
Coronary artery disease (CAD) is the most common form of heart disease. It occurs when plaque—a sticky mix of fat, cholesterol, and other substances—builds up inside the arteries, narrowing the passageways that feed the heart muscle. This process, known as atherosclerosis, can develop silently over years until one day a clot forms, blocking blood flow completely and causing a heart attack.
But heart disease is not just physical. It is emotional, behavioral, environmental, and often, generational. It is shaped by how we eat, how we move, how we manage stress, and even how we connect with others. To prevent and recover from heart disease is to address not just arteries—but an entire way of life.
The Roots of Risk: How Heart Disease Takes Hold
Before we talk about prevention, we must understand how the storm gathers. The risk factors for heart disease are both visible and hidden, some within our control and others inherited.
High blood pressure, or hypertension, silently strains the heart by forcing it to work harder to pump blood. Over time, this pressure damages artery walls, making them more prone to plaque buildup.
High cholesterol—especially elevated levels of low-density lipoprotein (LDL)—adds fuel to this process. LDL particles embed in arterial walls, triggering inflammation and attracting white blood cells that contribute to plaque formation.
Diabetes, particularly type 2, further complicates the picture. High blood sugar damages blood vessels and increases the likelihood of atherosclerosis. Smokers are at even higher risk, as nicotine narrows blood vessels and carbon monoxide reduces oxygen in the blood, forcing the heart into overdrive.
But risk isn’t just physical. Chronic stress floods the body with adrenaline and cortisol, increasing blood pressure and triggering inflammatory pathways. Poor sleep, social isolation, and even depression can all strain the cardiovascular system. The heart, it turns out, is exquisitely sensitive not just to diet and exercise—but to emotion and connection.
The Power of Prevention: A New Life Before It Begins
Prevention begins with knowledge, but it blossoms with intention. The steps we take before disease sets in can be more powerful than any pill. Preventing heart disease doesn’t mean a life of bland food and rigid routines—it means living more fully, more energetically, more aligned with the biology of well-being.
The foundation of prevention lies in lifestyle: eating a heart-healthy diet, staying physically active, managing stress, and avoiding harmful habits like smoking or excessive alcohol consumption. But this is not about restriction. It’s about nourishment.
The Mediterranean diet—rich in vegetables, fruits, whole grains, legumes, nuts, olive oil, and lean proteins like fish—has been shown to reduce the risk of heart disease significantly. This way of eating doesn’t just lower LDL cholesterol; it boosts HDL (“good”) cholesterol, reduces inflammation, and stabilizes blood sugar.
Exercise, too, is a cornerstone. The heart is a muscle, and like any muscle, it thrives on activity. Even 30 minutes of brisk walking five times a week can cut heart disease risk in half. But more than that, movement reconnects us with our bodies, clears our minds, and releases endorphins that counteract stress.
Managing stress is perhaps the most underappreciated form of prevention. Meditation, yoga, deep breathing, even simply spending time in nature can reduce blood pressure and lower cortisol. These practices are not indulgences; they are medicine.
When the Storm Breaks: Facing a Diagnosis
For many, heart disease becomes real only after a diagnosis—a heart attack, a coronary stent, a blocked artery revealed on a scan. These moments are terrifying, and understandably so. But they can also be clarifying. They strip life down to its essentials, reminding us what truly matters.
The first hours after a heart event are about survival. Clot-busting drugs, catheterization, bypass surgery—these tools of modern cardiology are nothing short of miraculous. They save lives every day. But the days and weeks that follow are about something deeper: how to rebuild a life on new terms.
Cardiac rehabilitation is an essential part of recovery. This medically supervised program combines exercise training, education, and counseling to help people regain strength, confidence, and control. Studies show that patients who complete cardiac rehab have significantly lower mortality rates, fewer hospitalizations, and better quality of life.
But recovery also happens in quieter moments—choosing a salad instead of a burger, walking to the store instead of driving, turning off the phone to sleep. Each decision becomes a vote for life. And gradually, the fear that once dominated gives way to empowerment.
The Emotional Landscape of Heart Recovery
Heart disease doesn’t just wound the body—it shakes the soul. After a heart attack or surgery, many people feel vulnerable, anxious, even depressed. The illusion of invincibility is gone. The heart becomes something to watch, worry about, sometimes even fear.
It’s common to ask: Why me? What now? Will it happen again?
These are not just medical questions. They are existential ones. And they require more than medication. They require healing.
Talking to others—whether in support groups, therapy, or simply with loved ones—can lift the burden. So can rediscovering purpose. Volunteering, creating, mentoring, learning—these acts remind us that life is not over. In fact, for many survivors, life after heart disease is more vivid than ever.
The Japanese have a word: “ikigai,” meaning reason for being. Recovery is not just about preventing the next event. It’s about finding your ikigai—what makes your heart beat not just literally, but passionately.
The Role of Medication: Allies, Not Enemies
While lifestyle change is foundational, medication often plays a vital role—especially after a diagnosis. Statins, blood pressure medications, antiplatelet drugs like aspirin—they’re not just chemical interventions. They are tools, allies, sometimes life-saving ones.
Statins lower cholesterol and reduce inflammation in artery walls. ACE inhibitors and beta blockers ease the heart’s workload. Aspirin helps prevent clots from forming. These medications are evidence-based and time-tested. But they work best when combined with lifestyle changes, not in place of them.
It’s important to take medications consistently and communicate openly with your healthcare provider. Side effects can usually be managed, and the benefits—lower risk of stroke, heart attack, or sudden death—are often profound.
What matters most is not medication alone, but the mindset of healing: knowing that each pill, each step, each salad, each breath is part of your recovery journey.
Women and Heart Disease: The Misunderstood Risk
Heart disease is often thought of as a “man’s problem,” but this misconception has proven deadly. Heart disease is the leading cause of death for women globally, and yet many women—and even healthcare providers—fail to recognize the signs.
Women are more likely to experience subtle symptoms: fatigue, shortness of breath, nausea, back or jaw pain. These can be mistaken for anxiety, indigestion, or flu. As a result, women often delay seeking care, and when they do, their symptoms may be dismissed.
This delay can cost lives.
Awareness is power. Women need to know their numbers—blood pressure, cholesterol, blood sugar—and advocate for their health. Hormonal shifts during menopause increase risk, making midlife a critical window for prevention.
But women also tend to be more socially connected and emotionally expressive—both protective factors. Harnessing these strengths can be part of a powerful recovery path.
Reversing the Damage: Is It Possible?
One of the most hopeful findings in cardiovascular medicine is that, in many cases, heart disease is not only preventable—it’s reversible.
Studies by Dr. Dean Ornish and others have shown that intensive lifestyle changes—including a plant-based diet, regular exercise, stress management, and social support—can not only halt but reverse atherosclerosis. Arteries can actually begin to open, plaque can regress, and symptoms can disappear.
This is not magic. It’s biology responding to nourishment.
But reversal requires commitment. It’s not a quick fix. It’s a lifestyle transformation. For those who choose it, the rewards are often astonishing—not just longer life, but better life, with less pain, more energy, and a renewed sense of purpose.
The Future of Heart Health: From Genes to AI
Medicine is entering a new era, where prevention and treatment will be increasingly personalized. Genetic testing can identify inherited risks. Wearable devices can monitor heart rhythms, activity, and even blood pressure in real-time. Artificial intelligence is beginning to analyze patterns and predict events before they happen.
But technology will never replace the basics: eat real food, move your body, manage stress, connect with others, sleep deeply, and stay curious.
The future of heart health lies in integrating science with humanity—in treating not just the disease, but the person.
Love, Connection, and the Healing Heart
In the end, the heart is not just a pump. It is a symbol. It is where we place our hand when we pledge, where we feel both grief and joy, where we fall in love and mourn.
Science has shown that love—real, human connection—actually protects the heart. People in healthy relationships live longer, recover faster, and have lower rates of heart disease. Isolation, by contrast, is as dangerous as smoking or obesity.
So don’t underestimate the power of presence. Hug your children. Call your parents. Forgive your enemies. Laugh with friends. Cry when you need to. All of it matters. All of it heals.
A Final Beat: Your Life, Your Heart
Heart disease is not a death sentence. It is a wake-up call. A chance to change course. To slow down. To listen. To remember what makes life worth living.
Prevention is not about fear—it’s about freedom. Recovery is not about limitation—it’s about liberation.
So start today. Not with guilt or perfectionism, but with compassion. Choose water over soda. Take a walk at sunset. Learn a new recipe. Sit in silence. Tell someone you love them. Every beat matters. Every choice counts.
Your heart is not just in your chest. It’s in your hands.