Imagine walking through a blooming garden on a warm spring day. The flowers are radiant, the air is filled with fragrance—and suddenly your eyes start watering, your nose begins to itch, and you cannot stop sneezing. For millions of people around the world, this isn’t just a passing annoyance; it’s a sign of an allergic reaction. Allergies are among the most common chronic conditions of modern times, affecting people of all ages and backgrounds. They are, in many ways, silent disruptors of daily life—sneaking into ordinary moments and turning them into struggles.
But allergies are more than just inconvenient. In severe cases, they can be life-threatening. From mild hay fever to dangerous anaphylaxis, allergic reactions are the immune system’s overzealous attempt to protect the body from substances that are, in reality, harmless. To understand allergies, we must dive into the complex workings of the immune system, the triggers that set off its alarms, and the ways modern medicine seeks to soothe its misguided vigilance.
What Are Allergies?
At their core, allergies are the result of an overactive immune system. Normally, the immune system protects us from harmful invaders such as bacteria, viruses, and toxins. It does this by recognizing foreign substances (antigens) and mounting a defense through antibodies, immune cells, and chemical messengers.
In the case of allergies, however, the immune system mistakes harmless substances—like pollen, pet dander, dust mites, peanuts, or shellfish—as dangerous invaders. This misidentification triggers a cascade of immune responses, releasing chemicals such as histamine that cause the characteristic symptoms of allergies: sneezing, itching, swelling, or in severe cases, difficulty breathing.
Allergies can affect nearly any part of the body: the skin, respiratory system, digestive tract, and even the cardiovascular system. They can range from mild discomfort to potentially fatal conditions, making them one of the most unpredictable aspects of human health.
The Causes of Allergies: Why Does the Body Overreact?
The question that has puzzled scientists for centuries is: why does the immune system overreact in this way? The answer is multifaceted, involving genetics, environment, and immune system dynamics.
The Genetic Predisposition
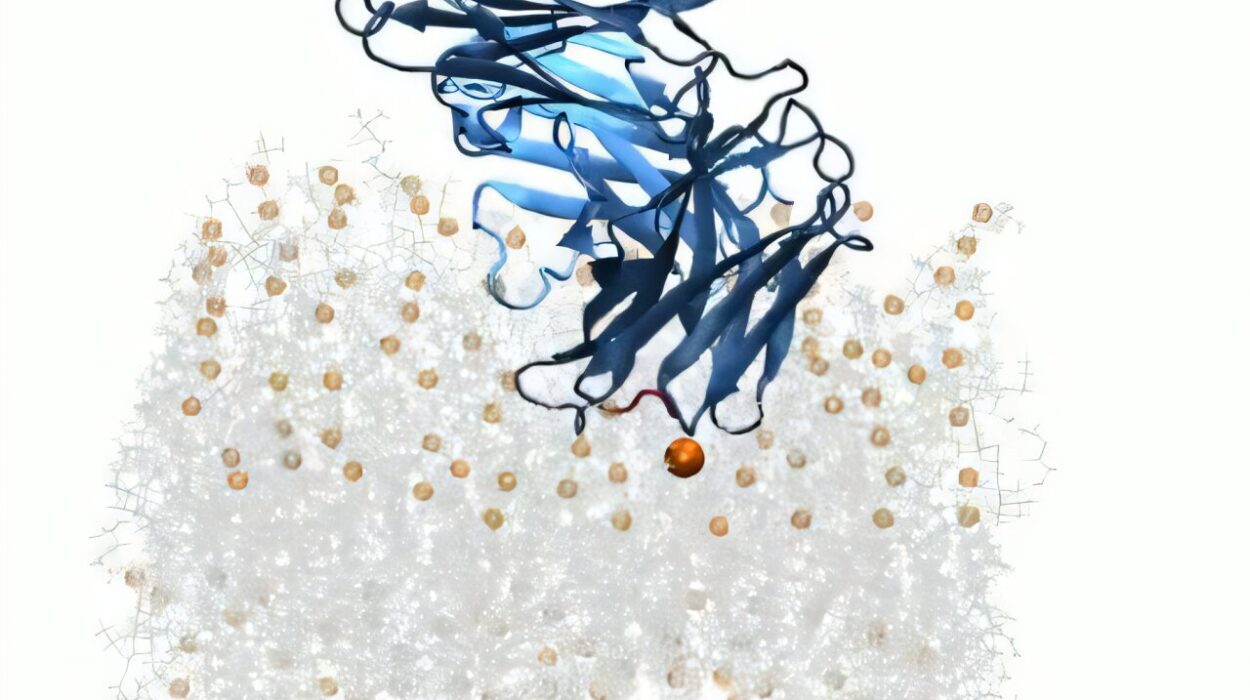
Allergies often run in families. If one parent has allergies, their child has a higher risk of developing them; if both parents are allergic, the risk is even greater. This hereditary tendency is known as atopy, and it reflects the likelihood of producing high levels of immunoglobulin E (IgE)—the antibody most involved in allergic reactions. Genes influence how the immune system responds to allergens and how sensitive it is to particular substances.
The Hygiene Hypothesis
One widely discussed explanation for the rise in allergies, especially in developed countries, is the hygiene hypothesis. This theory suggests that reduced exposure to microbes in early childhood—due to cleaner environments, antibiotics, and less contact with farm animals or natural soil—may leave the immune system “bored” and more likely to overreact to harmless substances. In other words, without enough real threats to fight, the immune system starts attacking pollen, peanuts, or cat hair.
Environmental Factors
Beyond genetics and hygiene, the environment plays a critical role. Pollution, climate change, and urban living have all been linked to increased allergy prevalence. For instance, warmer temperatures and higher carbon dioxide levels encourage plants to produce more pollen, prolonging allergy seasons. Indoor living, with exposure to dust mites and mold, adds another layer of constant triggers.
Immune System Imbalance
At the cellular level, allergies are often linked to an imbalance between two types of immune responses: Th1 (which fights microbes) and Th2 (which fights parasites). In allergic individuals, the Th2 response tends to dominate, producing excessive IgE antibodies that latch onto allergens and set off inflammatory reactions.
Common Allergens: The Triggers of Chaos
While almost any substance can potentially cause an allergy, some triggers are far more common than others.
- Airborne Allergens: Pollen, dust mites, mold spores, and animal dander are the main culprits behind hay fever (allergic rhinitis) and asthma.
- Food Allergens: Peanuts, tree nuts, shellfish, milk, eggs, soy, and wheat account for the majority of food allergies.
- Insect Allergens: Stings from bees, wasps, hornets, and fire ants can provoke severe reactions.
- Drug Allergens: Antibiotics like penicillin, certain pain relievers, and anesthesia agents are among the most common drug-related allergens.
- Contact Allergens: Substances like latex, nickel, and certain cosmetics can cause skin allergies such as dermatitis.
The severity of reactions to these allergens varies widely—one person might experience mild itchiness, while another could go into life-threatening anaphylactic shock from the same trigger.
Symptoms of Allergies: The Body’s Cry for Help
The symptoms of allergies depend on the type of allergen, the site of exposure, and the sensitivity of the individual. While often mild, they can interfere with daily activities and quality of life. In some cases, they escalate into emergencies.
Respiratory Allergies
When allergens enter the nose or lungs, they provoke symptoms such as sneezing, runny nose, nasal congestion, coughing, wheezing, and shortness of breath. Allergic rhinitis (hay fever) and allergic asthma fall into this category.
Skin Allergies
Direct contact with allergens or systemic reactions can cause itchy rashes, hives (urticaria), eczema flare-ups, and swelling (angioedema). The skin often acts as a mirror of the body’s allergic responses.
Food Allergies
Food allergies can produce symptoms within minutes to hours of ingestion. These range from itching in the mouth, swelling of lips and throat, nausea, and diarrhea to severe reactions like difficulty breathing and anaphylaxis.
Eye Allergies
Known as allergic conjunctivitis, these reactions cause red, itchy, watery, and swollen eyes. They are common in people with seasonal allergies.
Anaphylaxis: The Severe End of the Spectrum
Anaphylaxis is a rapid, systemic allergic reaction that can be fatal without immediate intervention. Symptoms include sudden swelling of the throat, difficulty breathing, a drop in blood pressure, dizziness, and loss of consciousness. It is a medical emergency requiring immediate treatment with epinephrine.
Diagnosis of Allergies: Unmasking the Triggers
Diagnosing allergies involves a combination of medical history, physical examination, and specialized tests. The process requires patience and precision because symptoms often overlap with other conditions like infections or intolerances.
Medical History and Symptom Diary
The first step is a thorough history. Doctors often ask patients to keep a diary of symptoms, noting when they occur, what exposures preceded them, and whether they vary by season, environment, or activity.
Skin Prick Test
This is one of the most common diagnostic tools. Small amounts of suspected allergens are introduced into the skin (usually on the forearm or back), and the site is monitored for swelling or redness. A positive reaction suggests an allergy to that substance.
Blood Tests
Tests such as the specific IgE blood test (RAST or ImmunoCAP) measure the level of IgE antibodies in the blood directed against particular allergens. This is especially useful when skin tests are not possible, such as in patients with skin conditions or those taking certain medications.
Elimination Diets and Food Challenges
For food allergies, elimination diets—removing suspected foods from the diet and gradually reintroducing them—can help identify triggers. The gold standard for diagnosis, however, is a medically supervised oral food challenge, in which the patient consumes small amounts of the suspected food under careful observation.
Pulmonary Function Tests
For suspected allergic asthma, lung function tests such as spirometry may be conducted to assess breathing capacity and airway responsiveness.
Treatment of Allergies: Restoring Balance
While there is currently no cure for allergies, treatments aim to reduce symptoms, prevent reactions, and improve quality of life. The approach often combines avoidance strategies, medications, and sometimes long-term therapies.
Allergen Avoidance
The most straightforward treatment is to minimize or avoid exposure to allergens. This can mean using air purifiers, encasing mattresses to reduce dust mites, avoiding outdoor activities during high pollen seasons, or strictly eliminating allergenic foods. For some people, avoidance alone can significantly reduce symptoms.
Medications
Medications play a central role in allergy management.
- Antihistamines: These block the effects of histamine, reducing symptoms like itching, sneezing, and runny nose. They are widely available both over-the-counter and by prescription.
- Decongestants: These relieve nasal congestion by shrinking swollen blood vessels in the nasal passages. They are effective for short-term use but not recommended for long-term relief due to potential side effects.
- Corticosteroids: Available as nasal sprays, inhalers, creams, or oral medications, corticosteroids reduce inflammation and are highly effective for chronic symptoms.
- Leukotriene Modifiers: These medications block the action of leukotrienes, chemicals involved in allergic inflammation, and are often used in asthma treatment.
- Epinephrine (Adrenaline): The lifesaving drug for anaphylaxis. People with severe allergies are often prescribed an epinephrine auto-injector (such as an EpiPen) to carry with them at all times.
Immunotherapy
For long-term relief, allergen immunotherapy is a groundbreaking treatment. It involves exposing the immune system to gradually increasing amounts of the allergen, either through injections (allergy shots) or sublingual tablets/drops. Over time, this retrains the immune system to tolerate the allergen, reducing symptoms and the need for medications.
Immunotherapy is particularly effective for environmental allergies like pollen and dust mites and has been shown to reduce the risk of developing asthma in children.
Lifestyle and Supportive Therapies
Managing allergies often requires a holistic approach. Saline nasal rinses can help clear allergens from nasal passages, moisturizers can soothe eczema-prone skin, and mindfulness practices can reduce stress that exacerbates symptoms. Support groups and counseling may also help individuals cope with the emotional and social burdens of living with chronic allergies.
Living With Allergies: Beyond Medicine
Allergies are not just a medical condition; they are a way of life. People living with allergies often adapt their daily routines, diets, and environments to protect themselves. This can be isolating, especially for children who feel different from their peers or adults who must constantly remain vigilant.
Education and awareness are powerful tools in easing this burden. Schools that train staff to recognize and respond to anaphylaxis, restaurants that clearly label allergens, and workplaces that accommodate allergy needs can all make life safer and less stressful.
Equally important is empathy. For someone with a peanut allergy, a casual snack left on a desk can pose a real danger. For someone with severe hay fever, springtime is not a season of joy but of misery. Recognizing the seriousness of allergies—even when they appear invisible—fosters understanding and inclusion.
The Future of Allergy Research: Hope on the Horizon
Science is moving rapidly toward better solutions for allergies. Researchers are exploring therapies that target the immune system at its roots, aiming not just to relieve symptoms but to cure allergies entirely.
New approaches include biologic drugs that block specific immune pathways, vaccines that desensitize the body to allergens, and even gene-editing technologies that may one day correct the underlying predisposition. The gut microbiome—our internal ecosystem of bacteria—is also under investigation, as it appears to play a role in regulating immune responses and allergy risk.
These breakthroughs hold the promise of transforming allergies from lifelong burdens into manageable or even preventable conditions.
Allergies as a Reflection of Humanity
In a way, allergies remind us of the fragility and complexity of the human body. They show us how a system designed to protect can sometimes harm, how the immune system’s vigilance can become its own worst enemy. Yet they also remind us of resilience: the millions of people who adapt, persevere, and thrive despite these challenges.
To understand allergies is to understand the dance between body and environment, between defense and overreaction. It is to recognize that health is not always about perfection but about finding balance in a world full of both threats and harmless beauty.
Allergies may be disruptive, but they do not define a person’s life. With science, compassion, and awareness, we can create a world where those living with allergies feel not only safe but also empowered to embrace life fully—flowers, foods, and all.