In the realm of public health, few concepts are as powerful or as misunderstood as herd immunity. It’s a term that has dominated headlines during pandemics, stirred debates on vaccine policies, and influenced global health decisions. But beyond the buzzwords and controversy, herd immunity is rooted in solid science and centuries of observation.
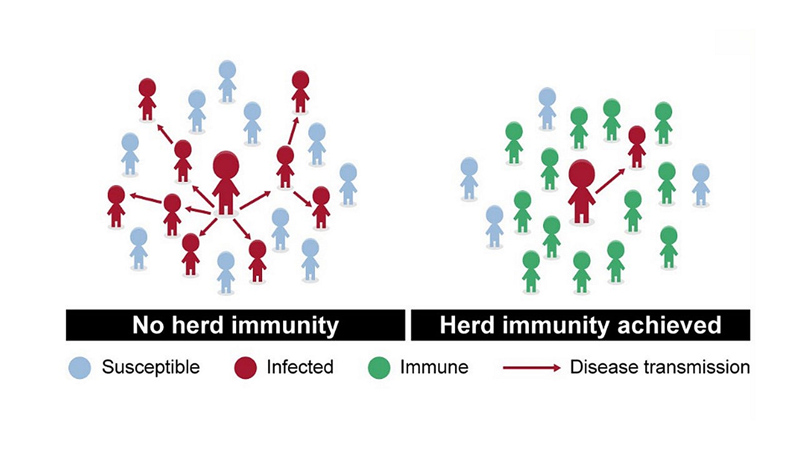
At its core, herd immunity is not just about protecting oneself—it’s about building a collective shield, a form of indirect protection that arises when a large portion of a community becomes immune to a disease, making its spread unlikely. This phenomenon doesn’t just help the immune; it protects the vulnerable—infants, the elderly, and those with compromised immune systems—who may not be able to protect themselves.
This article delves deep into what herd immunity really is, how it works biologically and mathematically, the role vaccines play, the diseases it has helped to control or eliminate, the myths that surround it, and its relevance in our modern, interconnected world.
The Biological Basis: How Disease Spreads
To understand herd immunity, we must first understand how infectious diseases spread. When a pathogen—such as a virus or bacterium—enters a host, it can multiply and be transmitted to other individuals through various means: respiratory droplets, bodily fluids, contaminated surfaces, or vectors like mosquitoes.
The speed and reach of this spread are influenced by a key metric known as the basic reproduction number, or R₀ (R-naught). This number represents the average number of people one infected individual will transmit the disease to in a population with no immunity.
For example:
- Measles has an R₀ of 12–18.
- Influenza typically ranges from 1.3 to 1.8.
- COVID-19 (original strain) had an R₀ of around 2–3, but newer variants have seen higher numbers.
The higher the R₀, the more contagious the disease—and the harder it is to control.
Herd Immunity Threshold: The Mathematical Concept
The idea of herd immunity relies on the principle of transmission interruption. If enough people in a population are immune—either through vaccination or past infection—the pathogen has fewer hosts to infect. This creates a “dead end” for transmission, reducing the chances of outbreaks.
Mathematically, the herd immunity threshold (HIT) can be calculated using the formula:
HIT = 1 – (1 / R₀)
Let’s break that down:
- For measles (R₀ of ~15), the HIT is 1 – (1/15) = 0.933, or 93.3% of the population.
- For a disease with an R₀ of 2, the HIT is 50%.
- For COVID-19 variants with R₀ around 6, HIT approaches 83%.
This formula tells us how much of the population needs immunity to prevent the disease from spreading. Importantly, the threshold is not about stopping every single case, but about preventing sustained transmission.
Natural Infection vs. Vaccination: The Path to Immunity
There are two ways people acquire immunity: through natural infection and through vaccination. While both can produce immunity, the consequences are vastly different.
Natural infection means the person gets sick and recovers, thereby gaining immunity. This might sound straightforward, but it comes with risks:
- Severe illness or complications.
- Death.
- Long-term health problems (e.g., long COVID, post-viral fatigue).
- Burden on healthcare systems.
Vaccination, on the other hand, introduces a safe form of the antigen—either inactivated, attenuated, or a piece of the pathogen—to stimulate the immune system without causing disease. It trains the body to recognize and fight the pathogen in the future.
The ethical and medical consensus is clear: vaccination is the safer and more controlled path to herd immunity.
The Role of Vaccines in Achieving Herd Immunity
Vaccines have been humanity’s most powerful tool for achieving herd immunity. The history of public health is rich with victories made possible by immunization campaigns.
Smallpox: A Case Study in Elimination
Smallpox, caused by the variola virus, was once a feared global killer. It had a high mortality rate and no known cure. But a global vaccination campaign, spearheaded by the World Health Organization (WHO), achieved something unprecedented: the eradication of smallpox in 1980.
The campaign relied not just on vaccinating everyone, but on reaching a high enough level of immunity in each community to halt transmission. This was one of the first successful applications of herd immunity on a global scale.
Polio: The Final Frontier?
Poliovirus, which can cause permanent paralysis, has been nearly eradicated thanks to aggressive immunization efforts. In 1988, there were more than 350,000 cases worldwide. By 2022, that number had dropped to under 100.
Here, herd immunity has helped protect entire populations. But interruptions in vaccination efforts can lead to resurgence—a powerful reminder of how delicate this protection can be.
Measles: A Reemerging Threat
Despite having an effective vaccine, measles has seen a resurgence in various countries due to declining vaccination rates. With an R₀ as high as 18, measles requires about 95% of the population to be immune to maintain herd protection.
In areas where vaccination dropped below that threshold—due to misinformation or logistical challenges—outbreaks flared up, often affecting those who couldn’t be vaccinated.
The Vulnerable Among Us: Why Herd Immunity Matters
One of the most compelling arguments for herd immunity is its role in protecting the most vulnerable:
- Newborns and infants, who may be too young to receive certain vaccines.
- Immunocompromised individuals, such as cancer patients, organ transplant recipients, or those with autoimmune disorders.
- Elderly populations, who often have weaker immune responses.
- People with severe allergies to vaccine components.
These individuals rely on the immunity of others to reduce their exposure risk. When herd immunity is achieved, the virus or bacteria is less likely to circulate, reducing the odds of contact. It’s not just a public health strategy—it’s a moral responsibility.
The Pitfalls of Relying Solely on Natural Infection
Some have suggested achieving herd immunity by allowing a virus to spread unchecked through the population—especially during the COVID-19 pandemic. While this idea might sound like a “shortcut,” it’s fraught with danger.
Let’s look at why this approach is flawed:
- High Death Toll: Allowing widespread infection leads to thousands or even millions of deaths.
- Overwhelmed Healthcare: Hospitals become overburdened, reducing care quality not only for infectious disease but also for emergencies like heart attacks and accidents.
- Long-term Health Consequences: Not everyone fully recovers. Chronic symptoms can follow even mild infections.
- Unpredictability: Viruses mutate. A strategy based on natural infection can backfire if new variants evade immunity.
Ethically, allowing disease to run rampant in hopes of natural herd immunity is unacceptable in modern medicine.
Challenges in Achieving Herd Immunity
Despite its theoretical clarity, herd immunity can be difficult to achieve or maintain. Here’s why:
Waning Immunity
Some vaccines or infections do not confer lifelong protection. Boosters may be needed to maintain immunity levels. Without periodic vaccination, the percentage of immune individuals can fall below the herd immunity threshold.
Mutating Pathogens
RNA viruses like influenza and SARS-CoV-2 mutate rapidly. New variants may partially or fully escape previous immunity, requiring updated vaccines or new strategies.
Vaccine Hesitancy
Public trust in vaccines is essential. In some communities, misinformation, historical abuses, or cultural beliefs lead to vaccine refusal. This creates clusters of unvaccinated individuals vulnerable to outbreaks.
Global Disparities
Access to vaccines is not equal. Low-income countries often struggle with supply, distribution, and storage. Until immunity is global, diseases can circulate and re-enter even well-vaccinated populations.
Asymptomatic Transmission
Diseases like COVID-19 can spread even when people show no symptoms, making control more difficult and undermining the effectiveness of herd protection unless a very high percentage is immune.
The Immunological Mechanism: How Vaccines Protect
To understand how herd immunity builds, we must understand how the immune system responds to a vaccine.
When a vaccine is administered, the body is exposed to a harmless version or component of the pathogen—enough to stimulate an immune response. This leads to the production of antibodies and the development of memory cells.
If the real pathogen invades later, these memory cells recognize it and mount a rapid, strong response, often neutralizing it before symptoms occur.
When many people in a community have these memory cells, the pathogen faces a “wall” of resistance. Fewer infections lead to fewer opportunities for mutation and fewer chances for vulnerable people to encounter the disease.
The Ethical Dimension: Individual Freedom vs. Collective Health
One of the most contentious aspects of herd immunity involves the balance between personal choice and societal responsibility. In some countries, vaccine mandates have sparked legal battles and protests.
From a public health perspective, the argument is clear: your immunity protects others. But this must be balanced with transparent communication, education, and respect for individual concerns.
It’s crucial that efforts to promote herd immunity are grounded in:
- Trust between health institutions and the public.
- Access to accurate information.
- Equity in healthcare availability.
COVID-19 and the Evolution of Herd Immunity Thinking
The COVID-19 pandemic offered the world a crash course in herd immunity. Early on, experts estimated a threshold around 60–70%, but as more transmissible variants emerged, those estimates rose to 80% or more.
Complicating factors included:
- Breakthrough infections, where vaccinated individuals still got infected.
- Variant escape, where immunity from earlier strains was less effective.
- Behavioral changes, like mask use and social distancing, which influenced transmission independent of immunity.
It became clear that herd immunity for COVID-19, in the traditional sense, might not be fully achievable—but widespread immunity still drastically reduced hospitalizations, severe disease, and deaths.
The Future of Herd Immunity: What Lies Ahead?
Looking forward, herd immunity remains a cornerstone of infectious disease control. But it’s not a panacea. It works best when paired with:
- Surveillance systems to track outbreaks.
- Global cooperation in vaccine distribution.
- Public education campaigns to counter misinformation.
- Ongoing research into immune response and pathogen evolution.
Diseases that mutate slowly and have effective vaccines (like measles or rubella) are excellent candidates for herd immunity. Rapidly mutating viruses with animal reservoirs (like influenza or coronaviruses) may require more dynamic strategies.
Still, the principle remains vital: when enough people are protected, everyone benefits.
Conclusion: Strength in Numbers
Herd immunity is not just a scientific concept—it is a profound expression of human interdependence. It reminds us that our health is intertwined, that our actions ripple beyond our individual lives, and that the most vulnerable among us depend on the immunity of others for protection.
It also reflects the power of modern medicine to tame the most dangerous diseases through understanding, cooperation, and technology.
Achieving herd immunity is not always easy. It requires public trust, scientific diligence, ethical reflection, and political will. But history has shown us what is possible when we commit to it. Smallpox is gone. Polio is nearly extinct. Measles can be controlled. COVID-19, despite its challenges, has been blunted.
When we immunize, we do more than protect ourselves—we build a collective fortress, a public shield that says: we care for each other. And in a world still threatened by emerging infections, that might be our most powerful medicine of all.