Fasting has become one of the most talked-about health trends of the last decade. From intermittent fasting schedules to ketogenic diets, millions of people are experimenting with food restriction as a way to lose weight, improve energy, or even enhance longevity. But new research from the University of British Columbia Okanagan (UBCO) suggests that fasting may not affect everyone equally—particularly when it comes to people living with obesity.
“Fasting and low-carbohydrate meals can benefit many people,” explains Dr. Hashim Islam, Assistant Professor in UBCO’s School of Health and Exercise Sciences. “But our study found that people with obesity may respond to fasting differently than leaner individuals, especially in how their immune systems react.”
The findings highlight that nutrition science is not one-size-fits-all, and that the biological effects of fasting may depend heavily on body type.
What Happens When We Fast?
When the body runs low on carbohydrates, it turns to stored fat as fuel. This metabolic shift produces molecules called ketones, which many scientists believe help reduce inflammation and improve immune function. Past studies have suggested fasting might strengthen the body’s defenses and even lower the risk of chronic diseases.
Lead author Dr. Helena Neudorf explains: “Fasting switches the body’s energy source from sugar to fat. This process not only burns stored fat but can also change how the immune system behaves.”
That switch, however, may not occur in the same way for people of different body compositions.
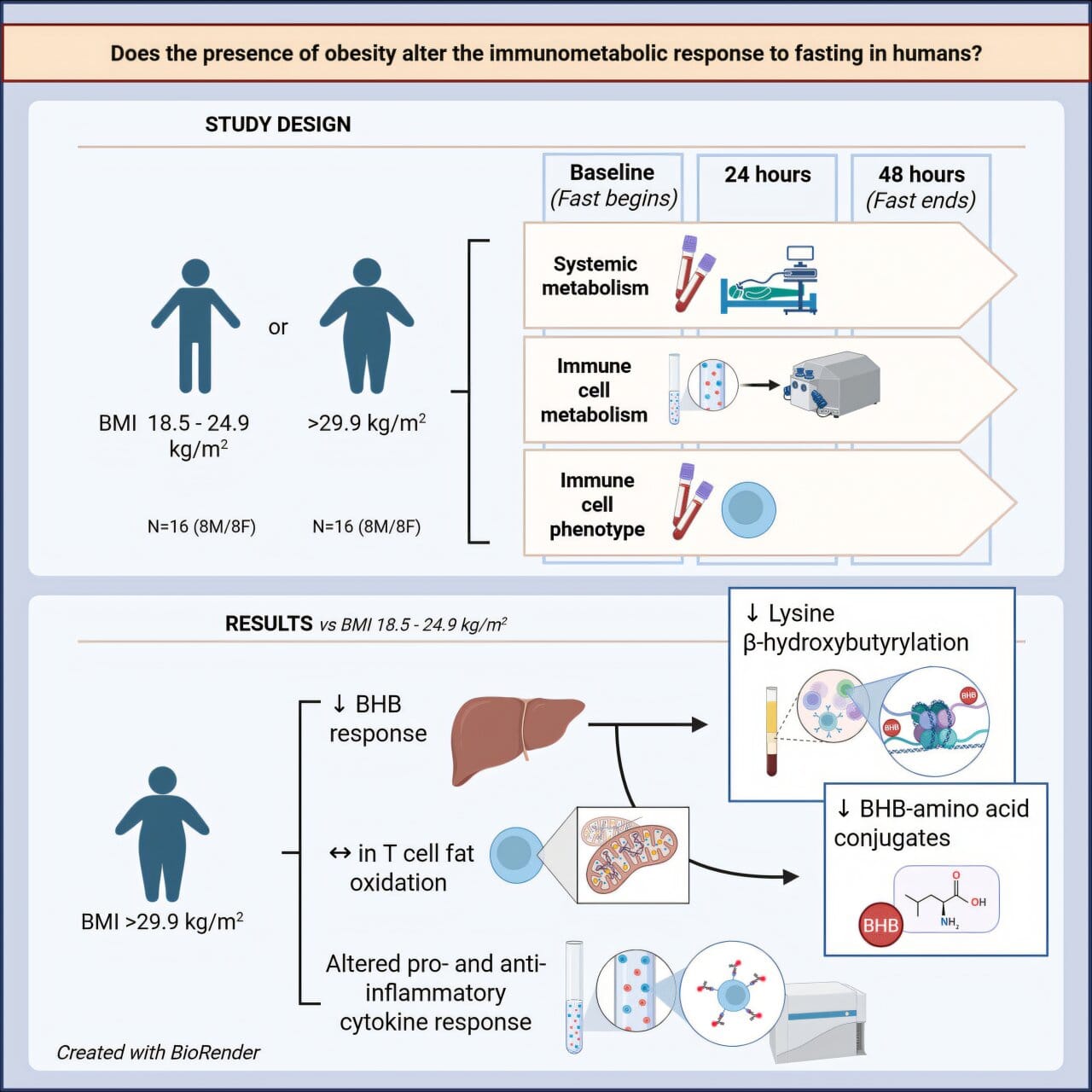
The Study: Lean vs. Obesity
To better understand these differences, researchers recruited two groups of participants—one lean and one living with obesity—and asked them to complete a 48-hour fast. Blood samples were collected before, during, and after fasting. The scientists examined metabolic rate, inflammation markers, hormone levels, and the behavior of T cells, a type of white blood cell that plays a key role in fighting infections and regulating inflammation.
The results, published in iScience, revealed striking contrasts. People with obesity showed higher levels of pro-inflammatory T cells and continued producing inflammatory signals even after fasting. They also had smaller increases in ketone levels and fewer chemical changes linked to immune regulation.
By contrast, lean participants adapted more efficiently. Their immune cells switched to burning fat, and their overall immune state shifted toward balance and lower inflammation.
“Overall, the anti-inflammatory benefits of fasting were weaker in people living with obesity,” says Dr. Neudorf.
Why This Matters
Obesity is already linked to chronic low-grade inflammation, a condition that raises the risk of heart disease, diabetes, and other serious illnesses. The new study suggests that fasting may not counteract this inflammation in the same way it does for lean individuals.
That doesn’t mean fasting is useless for people with obesity. Instead, it underscores the complexity of nutrition science. “People living with obesity may respond differently to an isolated two-day fast compared to those who are leaner,” notes Dr. Islam. “But we don’t yet know if these differences are ultimately beneficial or harmful.”
A Call for Personalized Nutrition
The research team emphasizes that more work is needed before drawing firm conclusions. The study involved only a short fast, and longer-term studies could reveal different effects. Still, the findings are a reminder that dietary advice cannot always be universal.
“Nutrition, metabolism, and immune function are deeply interconnected,” says Dr. Islam. “Our work shows we need to consider individual differences when recommending dietary strategies. What works for one body may not work for another.”
As fasting and ketogenic diets continue to gain global popularity, these insights could shape more personalized approaches to health—ensuring that people choose strategies that fit their unique biology, rather than following trends alone.
More information: Helena Neudorf et al, Altered immunometabolic response to fasting in humans living with obesity, iScience (2025). DOI: 10.1016/j.isci.2025.112872