Sepsis is one of the most feared words in modern medicine. It strikes quickly, spreads silently, and often overwhelms even the strongest bodies. Every year, up to 50 million people worldwide develop sepsis, and around 11 million die. It is the leading cause of death in hospitals, claiming more lives than breast cancer, HIV, and malaria combined. Once it sets in, every hour without effective treatment drastically increases the risk of death.
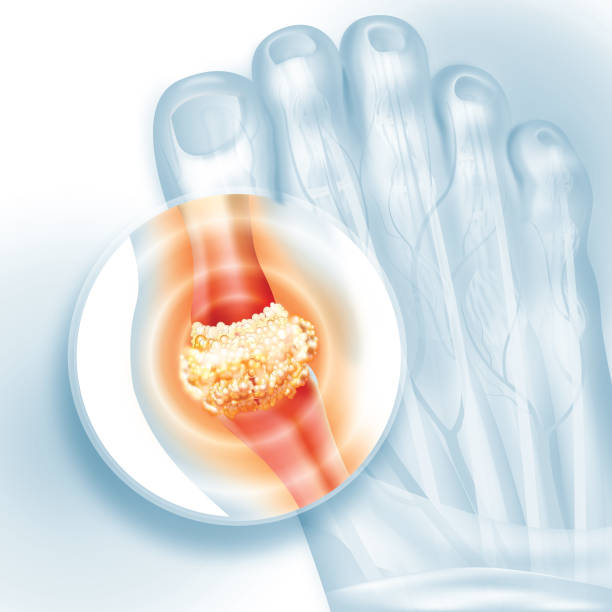
At its core, sepsis is the body’s immune system turning against itself. In trying to fight an infection, the immune response spirals out of control, creating a “cytokine storm” that can cause organ failure, shock, and death. Despite decades of research, doctors have few tools to fight it directly. Current treatments focus on antibiotics and supportive care, but even with the best efforts, mortality rates for severe sepsis can reach 40%.
Now, scientists at the University of Virginia School of Medicine and the University of Michigan believe they may have found a way to stop this deadly runaway process.
A First-of-Its-Kind Antibody
The research team has developed a monoclonal antibody designed specifically to prevent the immune system from going into overdrive. Early studies in mice have already shown extraordinary promise: the antibody not only blocked the dangerous cytokine storm but also restored the function of immune cells while protecting against lung damage.
“This is the kind of breakthrough that can change the standard of care,” said Jianjie Ma, Ph.D., of UVA’s Department of Surgery and UVA Cancer Center. “We’ve developed a first-in-class antibody with the potential to save countless lives from sepsis and other severe inflammatory diseases.”
Unlike older treatments, which often risk suppressing the immune system too much, this antibody seems to strike a careful balance—calming harmful inflammation without leaving the body defenseless. The researchers hope it will become the first therapy to directly address the root cause of sepsis rather than simply treating its symptoms.
Beyond Sepsis: A Wider Potential
While the initial focus is on saving lives from sepsis, the team’s findings could extend far beyond one disease. The antibody may prove useful in conditions where inflammation plays a destructive role, including autoimmune disorders, diabetes, cancer, and even complications seen during organ transplantation.
One of the most intriguing possibilities is treating acute respiratory distress syndrome (ARDS), a severe lung condition that gained international attention during the COVID-19 pandemic. If successful, the therapy could give doctors a powerful new tool against a wide range of life-threatening conditions where inflammation wreaks havoc.
“Our humanized antibody has shown both safety and effectiveness in blocking the cytokine storm and restoring healthy immune function,” said Yongqing Li, MD, Ph.D., of the University of Michigan. “Beyond acute infections, it has the potential to address a spectrum of diseases caused by faulty immune regulation.”
Diagnosing and Treating Together
The research does not stop with the antibody itself. The team has also developed an innovative diagnostic platform called PEdELISA, which can measure six key cytokines from just a drop of blood within two hours. This means doctors could not only treat sepsis but also monitor it in real time, adjusting therapies as needed.
By pairing the antibody with this diagnostic tool, physicians could finally take a personalized approach to sepsis care—detecting it earlier, tracking its progression, and responding quickly before organ damage becomes irreversible.
“Integrating PEdELISA with this first-in-class antibody therapy enables a comprehensive approach to sepsis management,” said industry collaborator Guidong Zhu. “It allows not only earlier and more accurate diagnosis but also continuous, near-real-time monitoring of the patient’s immune status throughout treatment.”
A Step Toward Clinical Trials
The researchers are preparing to test the antibody in human clinical trials at UVA Health and Virginia Commonwealth University. The antibody has already been engineered extensively for clinical use, and the team believes it is well-positioned to move from the lab into patient care.
For patients and families affected by sepsis, this progress represents more than just science—it represents hope. Hope that the terrifying unpredictability of sepsis could one day be replaced with an effective, reliable treatment.
Unlocking the Mysteries of Sepsis
In developing this antibody, the scientists have also uncovered new insights into how sepsis unfolds at the molecular level. They discovered harmful “feedback loops” in macrophages—immune cells that normally help protect the body—that instead drive the uncontrolled inflammatory cascade. By interrupting these loops, the antibody breaks the cycle before it becomes fatal.
This deeper understanding not only advances treatment but may also change the way doctors diagnose and predict the course of sepsis. Such knowledge could ultimately transform a once-mysterious killer into a condition that medicine can anticipate and defeat.
Toward a New Era of Care
For centuries, sepsis has been one of medicine’s most frustrating puzzles. Doctors could fight infections, but when the immune system itself became the enemy, their options were limited. The work from UVA and Michigan may finally change that narrative.
“UVA is proud to be part of this groundbreaking discovery,” said Melina R. Kibbe, MD, dean of UVA’s School of Medicine. “Our leadership is eager to move this bench discovery into the clinic, where it could make the difference between life and death.”
If clinical trials confirm the promise seen in early studies, this antibody could become a cornerstone of modern medicine, reshaping how doctors approach not just sepsis but a wide array of inflammatory diseases. For millions of patients worldwide, it could mean the difference between survival and tragedy.
More information: Wenlu Ouyang et al, A citrullinated histone H3 monoclonal antibody for immune modulation in sepsis, Nature Communications (2025). DOI: 10.1038/s41467-025-62788-6