When we think about illness, we often imagine fever, fatigue, or perhaps a cough. But beneath these outward signs lies a hidden world—a microscopic battlefield waged by lifeforms so small they are invisible to the naked eye. These organisms—bacteria, viruses, fungi, and parasites—are everywhere. They float in the air we breathe, hide in the food we eat, and cling to the surfaces we touch. Most of them are harmless. Many are even helpful. But some have the power to upend human lives, challenge modern medicine, and remind us how fragile our biology can be.
To truly understand the forces that cause infectious diseases, we must dive into the biological nature of these microscopic entities. Despite their similar association with illness, they differ vastly in structure, behavior, reproduction, and interaction with their hosts. They belong to entirely different branches of life, and their strategies for survival and attack are as diverse as the symptoms they cause.
Bacteria: Ancient Architects of Life and Illness
Long before humans walked the Earth—or even before Earth had animals or plants—bacteria reigned supreme. These single-celled organisms are among the oldest lifeforms on the planet, dating back more than 3.5 billion years. Found in every conceivable environment—from the icy crusts of Antarctica to the boiling vents of the ocean floor—bacteria are masters of survival. Some need oxygen to thrive, while others die in its presence. Some live off sugars and starches; others digest sulfur or methane. They are astonishingly diverse, adaptable, and ubiquitous.
Structurally, bacteria are prokaryotic, meaning they lack a defined nucleus and membrane-bound organelles. Instead, their genetic material floats freely in a circular strand called the nucleoid. Their simplicity is deceptive. Despite having no brains or nervous systems, bacteria coordinate their behavior with surprising sophistication, especially when forming biofilms or launching an attack on a host.
Many bacteria are beneficial. Our own bodies contain trillions of them, especially in the gut, where they help digest food, synthesize vitamins, and keep harmful microbes in check. Without these symbiotic relationships, our immune systems and metabolisms would collapse.
But other bacteria can be deadly. Pathogenic bacteria—those that cause disease—have evolved mechanisms to evade the immune system, cling to tissues, and release toxins. Tuberculosis, caused by Mycobacterium tuberculosis, hides inside immune cells and can persist for years. Streptococcus pneumoniae can lead to pneumonia and meningitis. Food poisoning from Salmonella or Escherichia coli can strike quickly and violently. Yet, despite their power, bacteria can usually be defeated with antibiotics—a class of drugs that either kill bacteria outright or stop them from reproducing.
Still, this war is evolving. As antibiotics have become widespread, many bacteria have developed resistance. The rise of “superbugs”—strains resistant to multiple drugs—is a global health threat, underscoring the urgent need to understand bacteria not just as enemies, but as part of a dynamic and ancient ecosystem.
Viruses: Genetic Ghosts That Hijack Life
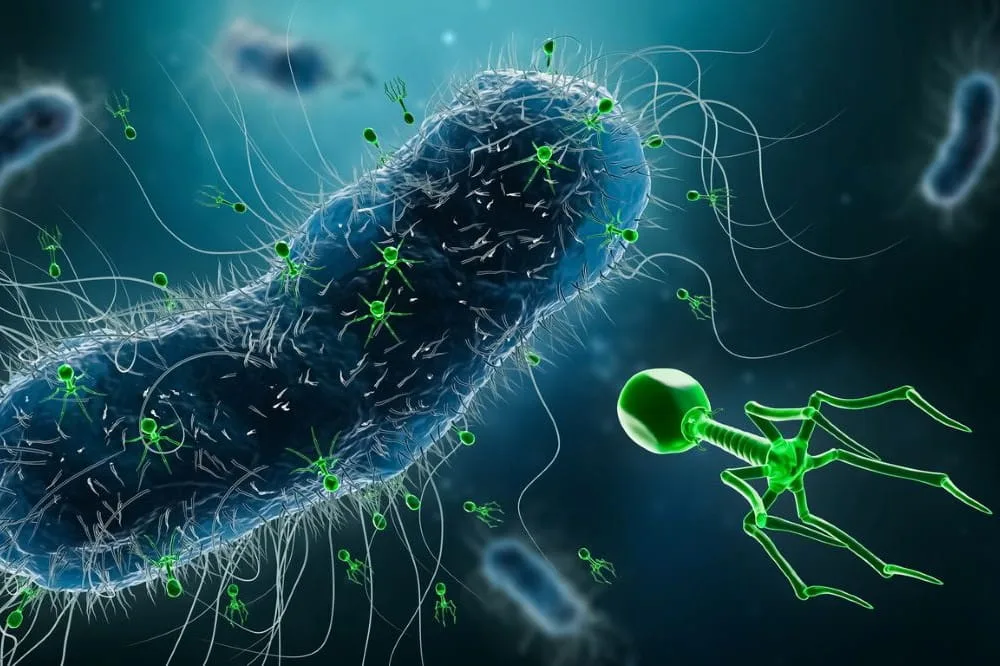
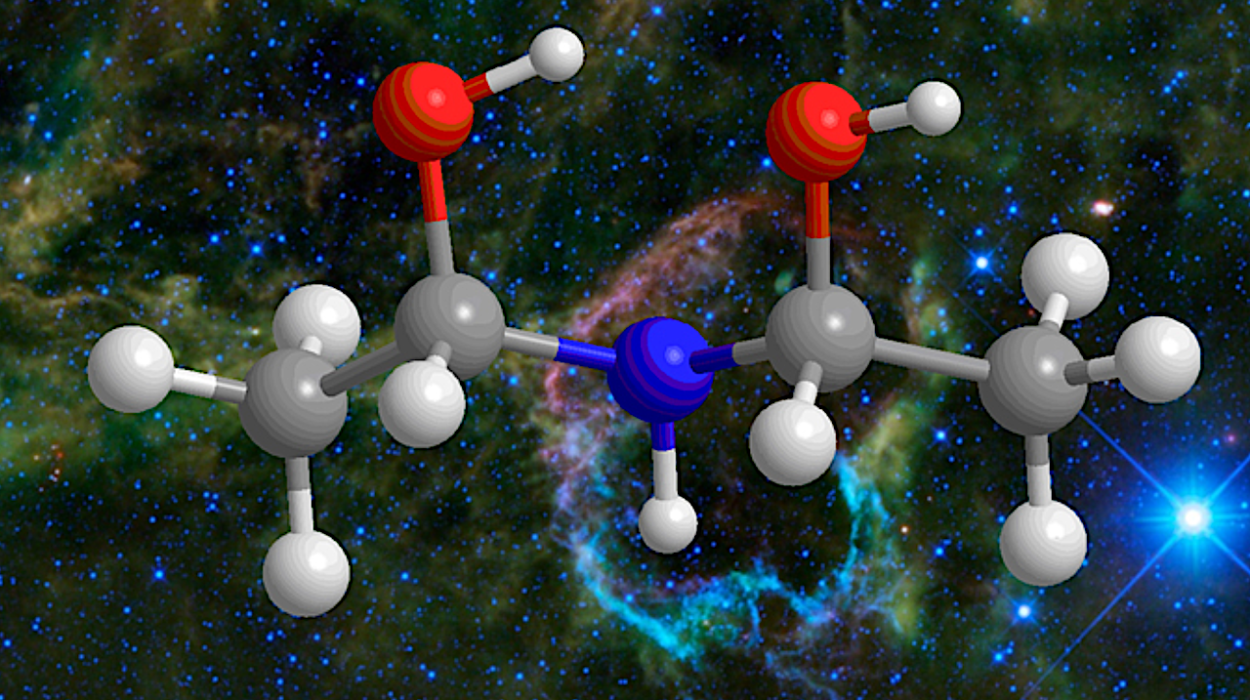
If bacteria are the ancient engineers of the microbial world, viruses are its cunning outlaws. Viruses are not alive in the traditional sense. They do not eat, grow, or carry out metabolic processes. Outside a host cell, a virus is inert—a molecular package of genetic material wrapped in a protein coat. Some also wear an outer lipid envelope, stolen from the cells they invade. But make no mistake: when a virus finds a host, it becomes one of the most efficient invaders in nature.
Viruses infect by inserting their genetic code—either DNA or RNA—into a living cell. Once inside, they hijack the host’s cellular machinery to replicate themselves. Some viruses burst the cell open to escape; others bud off slowly, cloaking themselves in the cell’s membrane. In both cases, the original cell is usually destroyed, and the virus spreads, often faster than the body can respond.
The diversity of viruses is staggering. Influenza, HIV, herpes, measles, hepatitis, and COVID-19 are all caused by different viruses, each with unique transmission methods, symptoms, and cellular targets. The smallest of them, like the poliovirus, can fit into a single bacterial cell thousands of times over. Others, such as the complex poxviruses, rival bacteria in size.
Because viruses don’t perform metabolic functions, antibiotics don’t work on them. Treating viral infections requires a different strategy—antiviral drugs that block specific stages of viral replication, or vaccines that prepare the immune system in advance. But developing these defenses is a constant arms race. Viruses mutate rapidly, especially RNA viruses, which lack error-correction mechanisms. This is why new strains of influenza emerge each year and why controlling emerging viruses like Ebola or SARS-CoV-2 requires a global, coordinated effort.
What makes viruses both terrifying and fascinating is their liminal existence between life and non-life. They blur the boundary between biology and chemistry, challenging our definitions and forcing us to rethink what it means to be alive.
Fungi: The Opportunists of the Microscopic World
Compared to bacteria and viruses, fungi are far more complex. They are eukaryotic organisms, meaning their cells contain a nucleus and organelles. In many ways, they are more closely related to animals than to plants. Most people know fungi as mushrooms, molds, or yeasts—but in the microbial world, fungi can be silent, deadly invaders.
Fungi can be single-celled, like Candida yeast, or multicellular, forming sprawling networks of filaments called hyphae. These filaments intertwine to form a structure known as mycelium, which can penetrate tissues and absorb nutrients. Unlike bacteria, fungi reproduce both sexually and asexually, often by releasing spores into the environment—spores that are resilient, easily airborne, and capable of surviving extreme conditions.
In healthy individuals, fungi usually pose no threat. Our immune systems are well-equipped to deal with them, and our skin and mucous membranes serve as effective barriers. But in those with weakened immunity—such as people undergoing chemotherapy, organ transplant recipients, or those with HIV/AIDS—fungal infections can become life-threatening.
Fungal pathogens like Aspergillus, Cryptococcus, and Histoplasma can infect the lungs, brain, and bloodstream. Candida albicans, normally a harmless resident of the mouth and gut, can become invasive in hospitals, especially via catheters or surgical wounds. Some fungal infections, like athlete’s foot or ringworm, are superficial and easily treated. Others, like mucormycosis (often called “black fungus”), can devour tissues with horrifying speed if not caught early.
One of the challenges of treating fungal infections is that fungi, being eukaryotes, share many cellular structures with humans. This makes it harder to design antifungal drugs that target fungi without harming human cells. As a result, antifungal medications tend to have more side effects and limited effectiveness compared to antibiotics.
Moreover, environmental changes and overuse of antifungals in agriculture have led to the emergence of drug-resistant strains, such as Candida auris, a hospital-acquired fungus that can be deadly and is difficult to eradicate.
Parasites: Masters of Manipulation and Survival
If bacteria are survivors and viruses are hijackers, parasites are masters of manipulation. Parasites are a diverse group of organisms that live in or on a host and benefit at the host’s expense. Unlike viruses and bacteria, many parasites are visible to the naked eye at some stage of their life cycle. They include protozoa (single-celled eukaryotes), helminths (worms), and ectoparasites like lice or ticks.
Parasites are found in nearly every ecosystem on Earth. They often have complex life cycles involving multiple hosts. Some reproduce sexually in one host and asexually in another. Others undergo metamorphosis or encysting stages to survive hostile environments. Their diversity and adaptability are nothing short of astonishing.
Protozoan parasites such as Plasmodium (which causes malaria), Giardia, and Entamoeba histolytica infect millions of people globally, often through contaminated water or insect vectors. Helminths—like tapeworms, roundworms, and flukes—can grow meters long and live for years inside the intestines, liver, or blood vessels of their hosts. Ectoparasites like mites and fleas can cause skin irritation and transmit other infections.
Parasites often manipulate host biology in ways that are eerily sophisticated. Toxoplasma gondii, a protozoan parasite, alters the behavior of infected rodents to make them less afraid of cats—its final host. Loa loa, the African eye worm, can migrate across a person’s eye, causing visible and painful distress. Some parasitic worms secrete proteins that suppress the host’s immune system, allowing them to persist undetected for years.
Treating parasitic infections depends heavily on identifying the organism involved. Antiparasitic drugs are diverse but often target metabolic pathways unique to the parasite. In many cases, eradication requires addressing environmental and social factors such as clean water, sanitation, and vector control.
Parasites also pose a growing challenge due to increasing global travel and climate change, which expand the range of vectors like mosquitoes and flies. Diseases once confined to tropical regions are now appearing in temperate areas, making parasite control a global health priority.
The Battle Within: The Immune System’s Response
Despite their differences, bacteria, viruses, fungi, and parasites share one thing in common: they all trigger the immune system. This complex network of cells, tissues, and signaling molecules works tirelessly to recognize and destroy invaders while preserving the body’s own cells.
When the immune system encounters a bacterial infection, it often responds with inflammation, fever, and white blood cells designed to engulf and destroy the bacteria. With viruses, the response is more nuanced. Infected cells send out distress signals called interferons, and special T cells hunt and destroy the compromised cells before the virus can replicate further.
Fungal infections often trigger a dual response—both innate (immediate and nonspecific) and adaptive (targeted and learned)—while parasitic infections can manipulate or dampen the immune response entirely. The immune system’s adaptability is both its strength and weakness; in its zeal to protect the body, it sometimes causes collateral damage, leading to autoimmune conditions or severe inflammation.
Vaccines, immune boosters, and modern diagnostic tools all leverage this natural defense system. Still, pathogens continue to evolve new ways to evade detection, making the immune system’s job a never-ending challenge.
Modern Medicine vs. Microbial Evolution
Our arsenal against infectious diseases has grown exponentially over the past century. Antibiotics, antivirals, antifungals, and antiparasitic drugs have saved millions of lives. Vaccines have eradicated smallpox and nearly eliminated polio. But nature is always adapting. The overuse and misuse of antimicrobial drugs, global travel, deforestation, and climate change have all contributed to the emergence of new pathogens and drug-resistant strains.
Multidrug-resistant tuberculosis, MRSA (methicillin-resistant Staphylococcus aureus), HIV mutations, fungal superbugs, and artemisinin-resistant malaria are just a few examples of this global crisis. These aren’t just scientific problems—they’re societal challenges requiring coordinated responses from healthcare systems, governments, and individuals.
Understanding the differences between pathogens is not an academic exercise—it’s a matter of survival. Each type of organism requires specific diagnostic tools, prevention strategies, and treatment plans. A misdiagnosed fungal infection treated with antibiotics won’t improve. A viral illness treated with unnecessary antibiotics may foster resistance. Precision, education, and innovation are our best defenses.
A Fragile Balance Between Life and Disease
For all their destructive potential, bacteria, viruses, fungi, and parasites are also part of life’s grand tapestry. Bacteria help digest our food and shape our immune systems. Harmless viruses called bacteriophages regulate microbial ecosystems. Fungi decompose organic material, recycling nutrients into soil. Even parasites play a role in shaping evolution and maintaining ecological balance.
The challenge is not to eradicate microbes, but to understand them—to distinguish friends from foes, to harness their power for good, and to defend ourselves when they turn against us. We live in a microbial world, shaped by invisible forces both ancient and ever-changing. The war between pathogens and people is not just a story of conflict, but of coexistence, resilience, and discovery.