In a discovery that may change how scientists view the connection between chronic diseases, an international research team led by the Medical University of Vienna has found that a protein long associated with diabetes could also be a powerful player in cancer treatment—specifically, prostate cancer. This protein, known as PPARγ (peroxisome proliferator-activated receptor gamma), is already familiar to endocrinologists for its critical role in regulating glucose metabolism and its use as a drug target in type 2 diabetes. But now, cancer researchers are peering into its hidden dimensions, uncovering a surprising influence on cancer cell growth and metabolism.
This revelation opens a promising new chapter in the search for targeted cancer therapies, suggesting that some drugs used for diabetes might be retooled as weapons against prostate cancer—a disease that remains one of the most formidable malignancies in men worldwide.
What is PPARγ? The Gene Switch at the Center of It All
PPARγ is more than just another protein. It’s a transcription factor—a molecular switch that controls the expression of numerous genes, especially those involved in metabolism, inflammation, and cell proliferation. In the world of diabetes, PPARγ has long been a superstar. For decades, researchers have known that activating this protein improves insulin sensitivity, making it a valuable target for drugs like pioglitazone, a member of the thiazolidinedione class.
By modulating the expression of genes in fat cells and other tissues, pioglitazone helps reduce blood glucose levels and mitigate insulin resistance. Its effects have made it a staple in the pharmacological arsenal against type 2 diabetes. But beneath its metabolic magic lies an underexplored potential: the capacity to influence cellular behaviors in cancer.
From Glucose to Growth: Shifting Focus to Prostate Cancer
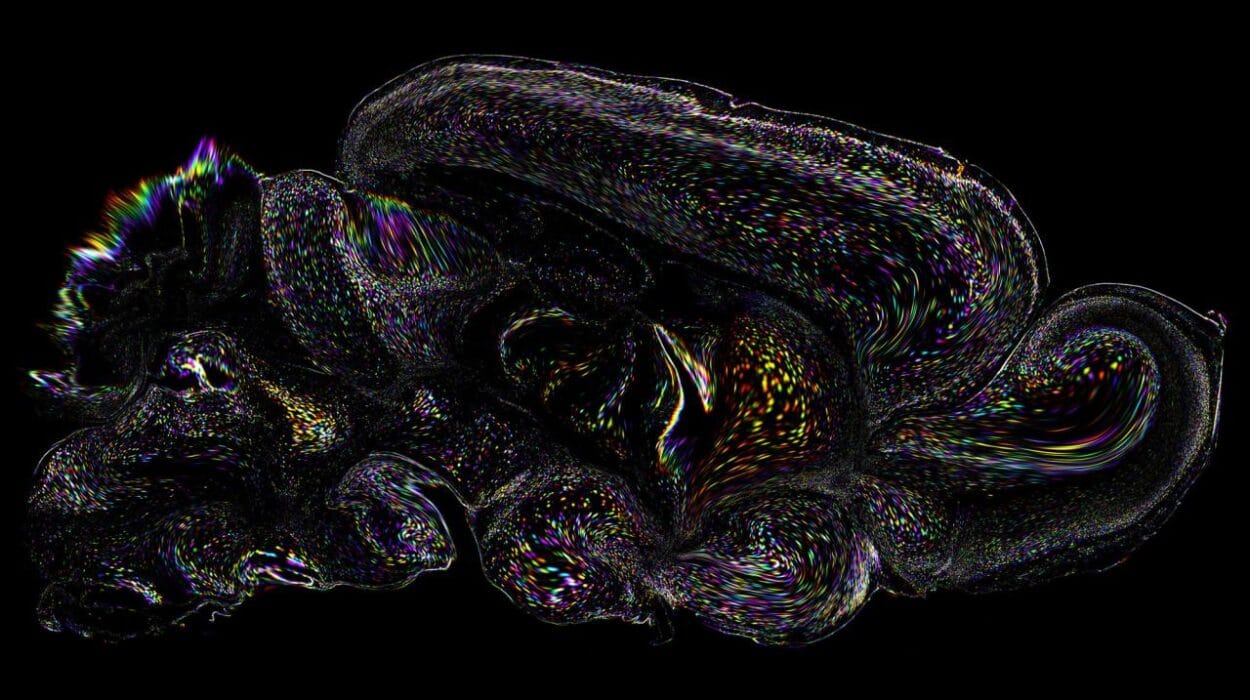
While diabetes and cancer might seem like vastly different diseases, both share a surprising number of molecular pathways, especially those governing metabolism and cell division. The Vienna-led research team, under the guidance of Lukas Kenner of the Clinical Department of Pathology at MedUni Vienna, decided to explore this intersection. Their central question: Could PPARγ, which regulates metabolic activity in diabetes, also regulate the growth of prostate cancer cells?
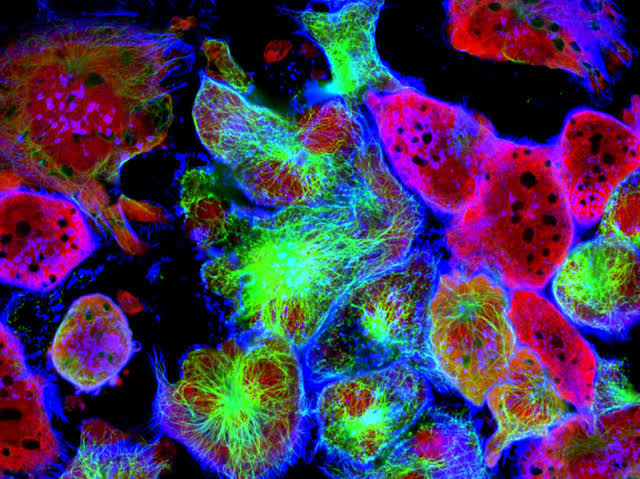
Using a combination of cell culture experiments and human tissue samples, the researchers meticulously analyzed how altering PPARγ’s activity influenced cancerous cells. Their findings were striking. When the diabetes drug pioglitazone was used to activate PPARγ, prostate cancer cells exhibited slower growth and altered metabolic behavior—signs of inhibited tumor progression.
More importantly, they noted that diabetic patients undergoing treatment with PPARγ agonists like pioglitazone showed no relapse of prostate cancer at the time of data collection. While early, these clinical observations point to an intriguing therapeutic opportunity: repurposing diabetes drugs for cancer treatment.
The Rise of Metabolic Oncology
The concept of targeting metabolism to fight cancer isn’t new. Since the early 20th century, scientists have observed that cancer cells behave differently when it comes to energy use—they consume glucose at a far higher rate than normal cells, a phenomenon known as the “Warburg effect.” This metabolic quirk has become a foundational concept in oncology. But what’s been missing is a reliable way to selectively manipulate these pathways without harming healthy cells.
That’s where PPARγ may come in. By selectively activating or inhibiting this protein, scientists might be able to tweak the metabolic programming of cancer cells, slowing or even reversing tumor growth. This research by the MedUni Vienna team is one of the most compelling examples yet of how a molecule from one disease field can serve as a bridge to new treatments in another.
Pioglitazone: A Drug with Dual Potential
Pioglitazone has had a long and sometimes controversial history. While effective at lowering blood sugar, its use has been marred by concerns about side effects, including weight gain, fluid retention, and in some studies, potential links to bladder cancer. But in recent years, a more nuanced view has emerged, and its profile as a metabolic modulator has regained interest—particularly among cancer researchers.
In this new study, pioglitazone’s ability to regulate PPARγ showed profound effects on prostate cancer cells. It didn’t just slow their growth; it altered the very way these cells metabolized energy, hinting at a deeper reprogramming of their internal biology. This dual-action profile—regulating both glucose metabolism and cancer cell behavior—positions pioglitazone as a fascinating candidate for drug repurposing.
A New Frontier for Prostate Cancer Therapy
Prostate cancer remains the second most common cancer in men globally, with hundreds of thousands of new cases diagnosed each year. In Austria alone, the disease claims the lives of roughly one in eight men with cancer, despite significant advances in early detection and treatment. The current treatment landscape ranges from surgery and radiation to hormone therapy and chemotherapy, depending on the stage and aggressiveness of the disease.
But these treatments can come with significant side effects and often lose effectiveness over time. That’s why the discovery of PPARγ’s role in tumor regulation is so compelling—it could offer a new molecular target for a subset of patients, particularly those who may not respond to conventional therapies.
And because drugs like pioglitazone are already approved and widely available, the path from lab bench to clinical trial could be significantly faster than with new, untested compounds.
A Step Toward Personalized Medicine
Another intriguing implication of this study is the potential to use PPARγ activation status as a biomarker. If doctors can identify which patients have tumors sensitive to PPARγ modulation, they could tailor treatments more precisely. This is a core goal of personalized medicine—matching the right treatment to the right patient based on molecular characteristics.
As lead researcher Emine Atas of MedUni Vienna’s Department of Biomedical Imaging explains, “We observed that patients with diabetes treated with PPARγ agonists showed no signs of prostate cancer relapse during our data collection. This not only highlights a potential therapeutic benefit but also suggests a prognostic role for PPARγ activity in clinical practice.”
Challenges and Future Research
While the findings are encouraging, the researchers are quick to point out that more work is needed. The current results are based on laboratory models and retrospective observations. To confirm pioglitazone’s effectiveness in treating prostate cancer, large-scale clinical trials must be conducted, comparing outcomes in patients who receive PPARγ-targeting drugs versus those who don’t.
There are also questions about the exact mechanisms through which PPARγ affects tumor growth. Does it act directly on cancer cell proliferation genes? Does it modulate the tumor microenvironment? Could there be synergistic effects when combined with other cancer treatments?
These are questions that the team plans to pursue in the next phase of their research, which could unlock even more applications for PPARγ modulation across different types of cancer.
The Broader Implications: Convergence of Disease Pathways
One of the most profound aspects of this discovery lies in its broader implication: diseases that we often think of as distinct—like diabetes and cancer—might share common molecular roots. By understanding these shared pathways, researchers can develop cross-cutting therapies that work across diseases, increasing efficiency and opening new doors in treatment.
This convergence also reflects a deeper truth about human biology: everything is connected. The systems that govern metabolism, cell growth, and inflammation do not operate in isolation. They are part of an intricate web, where a shift in one domain can ripple across others.
PPARγ, as it turns out, may be one of the key regulators in this web—a molecular bridge linking two of the most burdensome diseases of our time.
Conclusion: A New Direction for Cancer Therapy
This groundbreaking research is more than just a curiosity—it’s a potential turning point. By revealing that a diabetes drug can influence prostate cancer growth via PPARγ, the Medical University of Vienna and its international collaborators have shown how exploring intersections in biology can lead to unexpected and powerful breakthroughs.
As further studies unfold, the possibility of using metabolic drugs to control cancer could redefine our approach to oncology. What once seemed like separate frontiers—endocrinology and oncology—are now revealing a shared terrain rich with therapeutic potential. In that shared space, a new era of medicine may be taking shape—one where treating cancer could begin with a drug originally designed to manage blood sugar.
This is the power of science at its best: not just solving problems, but revealing new paths forward.
Reference: Emine Atas et al, The anti-diabetic PPARγ agonist Pioglitazone inhibits cell proliferation and induces metabolic reprogramming in prostate cancer, Molecular Cancer (2025). DOI: 10.1186/s12943-025-02320-y