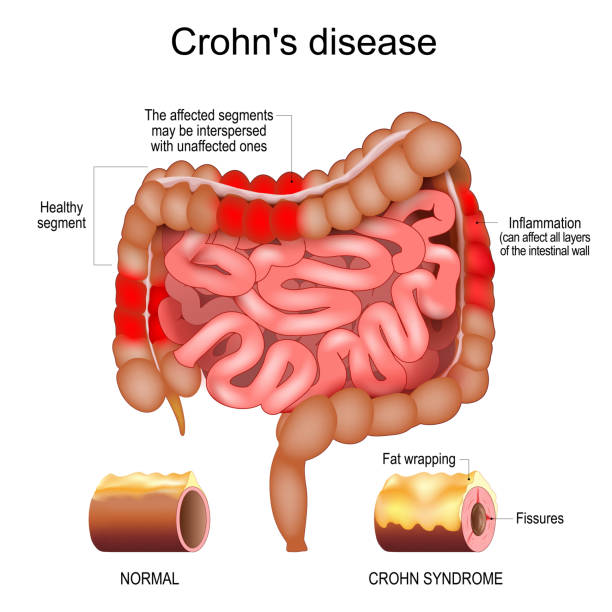
In the intricate landscape of human health, few conditions are as relentless and life-altering as Crohn’s disease. For those who live with it, Crohn’s is not merely a medical diagnosis; it is a companion that reshapes daily routines, influences emotions, and tests resilience. Unlike a fleeting illness that comes and goes, Crohn’s lingers—often unpredictable, sometimes silent, and other times fierce. It belongs to the group of disorders known as inflammatory bowel diseases (IBD), yet it carries its own unique fingerprint.
Crohn’s disease is defined by chronic inflammation that can strike anywhere along the digestive tract, from the mouth to the anus. It does not discriminate by age, gender, or background, though it often begins in adolescence or early adulthood. Its impact reaches far beyond the gut—it can affect nutrition, energy, mental health, and even social relationships. To truly understand Crohn’s is to explore its causes, recognize its symptoms, unravel how it is diagnosed, and learn about the evolving strategies for treatment and care.
The Science Behind Crohn’s: Searching for Causes
One of the most difficult questions in medicine is why Crohn’s disease develops. Despite decades of research, there is no single definitive cause. Instead, Crohn’s arises from a complex interplay of genetics, the immune system, environmental triggers, and gut microbiota.
Genetic Predisposition
Family history is one of the strongest risk factors. Studies show that if a close relative has Crohn’s, an individual’s risk is significantly higher. Scientists have identified over 200 genetic variations associated with inflammatory bowel disease, with some specific mutations linked directly to Crohn’s. For instance, mutations in the NOD2 gene are among the most well-studied, affecting how the immune system responds to bacteria in the intestines.
Immune System Dysregulation
At the heart of Crohn’s lies an immune system gone awry. Instead of protecting the body from harmful invaders, the immune system of someone with Crohn’s reacts excessively to the normal bacteria in the gut. This overreaction triggers chronic inflammation, which damages the lining of the digestive tract. It’s not that these bacteria are harmful, but rather the body mistakenly treats them as threats.
Environmental Triggers
Where someone lives, what they eat, and the conditions of their environment all influence the risk of developing Crohn’s. The disease is more common in industrialized countries, particularly in North America and Europe. This suggests that diet, sanitation, and modern lifestyles may play roles. Factors such as smoking, high-fat diets, stress, and frequent use of antibiotics have been linked to increased risk or worsened disease activity.
The Role of Gut Microbiota
The human gut is home to trillions of bacteria, fungi, and viruses that form a delicate ecosystem essential for digestion and immunity. In Crohn’s disease, this balance—called the microbiome—appears disrupted. Instead of a healthy mix of microbes, patients often show reduced diversity and an overgrowth of inflammatory bacterial species. Whether this imbalance is a cause or consequence of Crohn’s is still under investigation, but it clearly plays a role in the cycle of inflammation.
The Symptoms of Crohn’s Disease
Crohn’s disease does not follow a single script. Its symptoms vary widely from person to person, depending on where in the digestive tract the inflammation occurs and how severe it becomes. For some, symptoms are mild and manageable; for others, they are debilitating.
Digestive Symptoms
The most common and defining symptoms involve the digestive system. These include:
- Persistent diarrhea, often urgent and unpredictable.
- Abdominal pain and cramping, typically in the lower right side but potentially anywhere in the gut.
- Blood in the stool, a sign of intestinal bleeding.
- Reduced appetite and unintended weight loss.
Unlike many digestive illnesses that come and go, Crohn’s often follows a relapsing-remitting pattern—periods of flare-ups followed by times of remission. During remission, symptoms may fade, but the risk of another flare always lingers.
Systemic Symptoms
Crohn’s affects more than the gut. The ongoing inflammation can spread its impact throughout the body. Fatigue is one of the most reported symptoms, leaving patients drained even after rest. Fever may accompany flare-ups, signaling active inflammation. Children and adolescents with Crohn’s may experience delayed growth and puberty due to malnutrition and inflammation.
Extraintestinal Manifestations
One of the more surprising aspects of Crohn’s disease is its ability to cause problems outside the digestive tract. Up to one-third of patients experience extraintestinal symptoms, including:
- Joint pain and arthritis.
- Eye inflammation, such as uveitis.
- Skin conditions like erythema nodosum (red, tender nodules) or pyoderma gangrenosum (ulcerative lesions).
- Liver and bile duct disorders.
These manifestations highlight the systemic nature of Crohn’s—it is not just a gut disease but an immune-mediated disorder affecting the entire body.
Complications of Crohn’s Disease
If left uncontrolled, Crohn’s can lead to serious complications. The inflammation may penetrate deep into the intestinal wall, causing abscesses, fistulas (abnormal connections between different parts of the intestine or other organs), and strictures (narrowing of the intestine that can block food passage). These complications often require surgical intervention.
Long-term inflammation also increases the risk of colon cancer, particularly when Crohn’s affects the colon for many years. Malnutrition is another concern, as damaged intestines struggle to absorb nutrients effectively.
Diagnosing Crohn’s: Piecing Together the Puzzle
There is no single test that definitively diagnoses Crohn’s disease. Instead, doctors rely on a combination of medical history, physical examination, laboratory studies, imaging, and endoscopy to piece together the diagnosis.
Medical History and Physical Examination
The diagnostic journey begins with a thorough discussion of symptoms, family history, and lifestyle. Physicians also perform a physical exam to check for tenderness, abdominal masses, or signs of malnutrition.
Laboratory Tests
Blood tests may reveal anemia (low red blood cell count) or elevated markers of inflammation such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Stool tests are also important, as they help rule out infections and detect inflammation markers like calprotectin.
Imaging Studies
Techniques such as CT scans, MRI, and ultrasound allow doctors to see inside the abdomen, identify inflammation, strictures, or abscesses, and determine the extent of disease. MRI enterography, in particular, has become a valuable tool for visualizing the small intestine without exposing patients to radiation.
Endoscopy and Biopsy
Endoscopy remains the gold standard for diagnosing Crohn’s. Colonoscopy enables direct visualization of the colon and terminal ileum, where Crohn’s frequently occurs. During the procedure, doctors take biopsies—small samples of tissue—to examine under a microscope. The presence of granulomas, a type of immune cell cluster, strongly supports the diagnosis. Capsule endoscopy, where patients swallow a tiny camera, may be used to examine areas of the small intestine that are otherwise hard to reach.
Treatment of Crohn’s Disease
While there is no cure for Crohn’s disease, treatment aims to reduce inflammation, relieve symptoms, and maintain remission. Advances in medicine have greatly expanded the arsenal of therapies, giving patients more options and hope than ever before.
Medications
Anti-inflammatory drugs
Corticosteroids such as prednisone can quickly suppress inflammation and bring flare-ups under control. However, they are not suitable for long-term use due to side effects like weight gain, bone loss, and increased infection risk.
Immunosuppressants
Drugs like azathioprine, 6-mercaptopurine, and methotrexate weaken the overactive immune response, reducing inflammation over time. They require careful monitoring but can maintain long-term remission.
Biologic therapies
One of the greatest advances in Crohn’s treatment has been the development of biologics—engineered antibodies that target specific molecules in the immune system. Anti-TNF agents (such as infliximab and adalimumab) block tumor necrosis factor, a key driver of inflammation. Newer biologics target integrins (vedolizumab) or interleukins (ustekinumab), offering additional options when anti-TNFs fail.
Antibiotics and supportive drugs
In cases involving fistulas or abscesses, antibiotics may help. Pain relievers, antidiarrheal medications, and nutritional supplements also play supportive roles.
Nutrition and Lifestyle
Diet does not cause Crohn’s, but it significantly influences symptoms. During flare-ups, low-residue or liquid diets may ease discomfort by reducing strain on the intestines. Long-term, patients are encouraged to eat balanced diets rich in nutrients, avoid trigger foods, and consider supplements for vitamins and minerals commonly deficient in Crohn’s (such as vitamin D, B12, and iron).
Lifestyle adjustments, including quitting smoking, managing stress, and maintaining regular exercise, have been shown to improve outcomes and reduce flare-ups.
Surgery
For some patients, surgery becomes unavoidable. Up to 70% of those with Crohn’s will require surgery at some point in their lives, often to treat strictures, fistulas, or areas of severe damage. Surgery may involve removing diseased portions of the intestine, but it is not a cure—Crohn’s often returns near the surgical site. Still, surgery can provide years of relief and significantly improve quality of life.
Living with Crohn’s: The Human Experience
Beyond medical treatment, Crohn’s disease challenges the human spirit. It affects careers, relationships, and mental health. The unpredictability of flare-ups can cause anxiety, and the chronic nature of the disease can lead to depression. Yet, countless patients demonstrate extraordinary resilience, building supportive networks, advocating for awareness, and finding ways to live fully despite the disease.
Patient support groups and counseling services play crucial roles in addressing the emotional impact. Education about the disease empowers patients to make informed decisions and advocate for their own care. Advances in telemedicine and online communities also make it easier to connect with others who share the journey.
The Future of Crohn’s Disease Management
The horizon of Crohn’s treatment is filled with promise. Researchers are exploring personalized medicine approaches, tailoring therapy based on genetic and microbial profiles. Stem cell therapies, microbiome transplants, and novel biologics are being tested, offering hope for more effective and lasting solutions.
At the same time, increasing attention is being paid to the holistic management of Crohn’s—integrating mental health care, nutrition, lifestyle modification, and patient-centered approaches into standard treatment. This reflects a shift in medicine from simply treating disease to nurturing overall well-being.
Conclusion: Living Beyond Crohn’s
Crohn’s disease is a lifelong condition, but it is not the end of life’s possibilities. With scientific advances, compassionate care, and personal resilience, many people with Crohn’s live vibrant, fulfilling lives. The journey may involve detours, challenges, and battles, but it also inspires strength, adaptability, and courage.
Understanding Crohn’s—from its causes to its treatments—reminds us that health is not merely the absence of illness, but the presence of resilience, hope, and the will to keep moving forward. For those touched by Crohn’s, life is not defined by the disease but by the determination to thrive in spite of it.