Imagine a life where the simple act of eating a meal could stir anxiety, where a sudden cramp in the stomach feels like a storm rising, and where the fear of urgently needing a bathroom shadows even joyful moments. This is the reality for millions of people living with ulcerative colitis—a chronic disease that affects the large intestine and profoundly shapes daily life.
Ulcerative colitis is not just a medical condition; it is a companion that intrudes on work, relationships, travel, and even rest. Yet, it is also a condition where science, medicine, and human resilience meet. Understanding ulcerative colitis is about more than memorizing symptoms and treatments—it is about seeing the lives behind the diagnosis, the courage in managing flare-ups, and the ongoing search for lasting relief.
In this article, we will dive deep into ulcerative colitis—its causes, symptoms, diagnosis, and treatment—using both scientific clarity and empathetic language to make sense of a condition that is both biologically complex and emotionally demanding.
What Is Ulcerative Colitis?
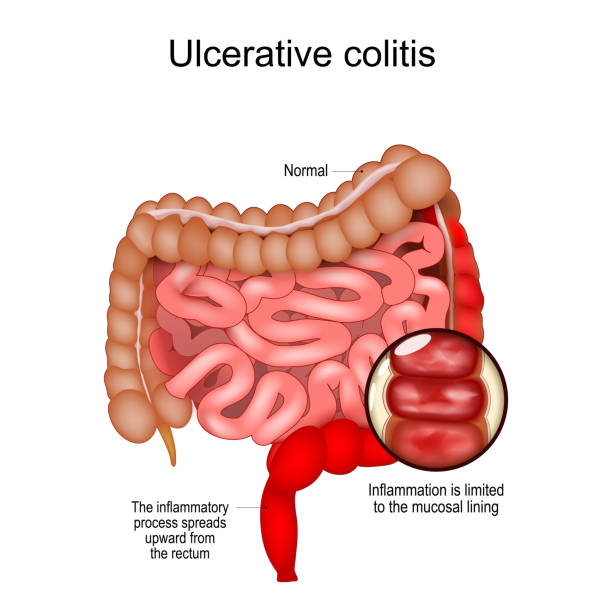
Ulcerative colitis (UC) is a chronic inflammatory disease that affects the large intestine, also known as the colon, as well as the rectum. It belongs to a group of conditions collectively called inflammatory bowel diseases (IBD), which also includes Crohn’s disease. Unlike Crohn’s, which can affect any part of the digestive tract, ulcerative colitis is limited to the colon and rectum.
The disease is characterized by long-lasting inflammation and the formation of ulcers on the inner lining of the colon. This inflammation disrupts the colon’s ability to absorb water and process waste, leading to frequent diarrhea, abdominal pain, and bleeding.
Ulcerative colitis is a lifelong condition. While it does not currently have a cure, modern medicine offers a variety of ways to manage symptoms, reduce inflammation, and allow people to live full, meaningful lives.
The Causes of Ulcerative Colitis
Despite decades of research, the precise cause of ulcerative colitis remains elusive. Scientists believe it results from a complex interaction of genetics, immune system dysfunction, environmental triggers, and lifestyle factors.
Genetic Susceptibility
Genetics plays a significant role. People with a family history of ulcerative colitis or Crohn’s disease are at a higher risk of developing the condition themselves. Studies have identified specific genetic variations—such as those involving immune regulation—that make individuals more susceptible. However, genes alone do not explain everything. Not everyone with a genetic predisposition develops ulcerative colitis, which means other factors must be involved.
Immune System Dysfunction
The immune system is designed to protect us from harmful invaders like bacteria and viruses. In ulcerative colitis, however, the immune system appears to misfire. Instead of targeting external threats, it attacks the cells of the colon’s lining. This misguided immune response leads to chronic inflammation and the painful symptoms of the disease.
Researchers believe this could be due to an abnormal reaction to the natural bacteria in the gut microbiome. Normally, these bacteria coexist peacefully with the body, aiding in digestion and immune function. In UC, the immune system may mistakenly perceive them as dangerous, launching a damaging inflammatory response.
Environmental and Lifestyle Factors
Environmental triggers also influence the onset of ulcerative colitis. Some of these include:
- Diet: While diet alone does not cause ulcerative colitis, certain foods may trigger flare-ups or worsen symptoms. High-fat diets, refined sugars, and low-fiber patterns are associated with inflammation.
- Infections: Previous gastrointestinal infections might alter the gut microbiome and immune response, paving the way for UC.
- Stress: Stress does not directly cause ulcerative colitis, but it can worsen symptoms and trigger flare-ups.
- Geography and lifestyle: Ulcerative colitis is more common in industrialized countries, suggesting that modern lifestyle factors—urban living, pollution, and reduced exposure to natural microbes—may play a role.
A Multifactorial Condition
The truth is, ulcerative colitis does not have a single cause. It is the result of multiple risk factors colliding. A person may carry genetic predispositions, encounter environmental triggers, and experience immune dysfunction, all leading to the chronic inflammation that defines UC.
Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis vary depending on the severity of inflammation and the specific part of the colon affected. The disease often develops gradually and can range from mild to life-threatening.
Common Symptoms
- Diarrhea: Often persistent and sometimes accompanied by blood or pus.
- Abdominal pain and cramping: Typically in the lower left abdomen but can occur anywhere.
- Rectal bleeding: A hallmark symptom caused by ulcers in the colon.
- Urgency to defecate: Sometimes with an inability to control bowel movements.
- Weight loss and fatigue: Due to malabsorption of nutrients, chronic inflammation, and frequent bowel movements.
- Fever: Occurs during more severe flare-ups.
Extraintestinal Symptoms
Ulcerative colitis does not confine itself to the gut. Many patients experience symptoms in other parts of the body, known as extraintestinal manifestations. These include:
- Joint pain or arthritis.
- Skin problems such as rashes, sores, or ulcers.
- Eye inflammation, including uveitis.
- Liver disease, such as primary sclerosing cholangitis.
Patterns of Flare-Ups and Remission
One of the most challenging aspects of ulcerative colitis is its unpredictability. Symptoms often come and go in cycles of flare-ups and remission. During flare-ups, inflammation is active, and symptoms intensify. During remission, symptoms improve or disappear entirely, though the disease remains in the body.
This unpredictable cycle makes ulcerative colitis not only a physical struggle but also an emotional and psychological challenge, as patients often live with the fear of the next flare.
Diagnosis of Ulcerative Colitis
Diagnosing ulcerative colitis can be complex, as its symptoms overlap with other gastrointestinal conditions such as Crohn’s disease, irritable bowel syndrome (IBS), and infections. Accurate diagnosis requires a combination of medical history, physical examination, laboratory tests, imaging, and endoscopic procedures.
Medical History and Physical Examination
The diagnostic journey usually begins with a detailed medical history, including questions about family history, symptom patterns, diet, and lifestyle. A physical exam may reveal tenderness in the abdomen or signs of anemia and weight loss.
Laboratory Tests
- Blood tests: These may detect anemia (low red blood cell count) due to chronic blood loss, or high inflammatory markers such as C-reactive protein (CRP).
- Stool tests: Used to rule out infections and to check for blood, pus, or inflammatory markers like calprotectin.
Endoscopic Evaluation
The most definitive diagnostic tool is colonoscopy. In this procedure, a flexible tube with a camera is inserted into the rectum, allowing doctors to view the inner lining of the colon. Colonoscopy can reveal hallmark signs of ulcerative colitis, such as continuous inflammation, ulcerations, and bleeding. Biopsies (small tissue samples) are often taken for microscopic examination.
Flexible sigmoidoscopy, a similar but less extensive procedure, examines only the lower part of the colon and may be used in milder cases or follow-ups.
Imaging Studies
In some cases, imaging tests such as CT scans or MRI scans may be used to evaluate the extent of inflammation and rule out complications. MRI enterography, in particular, can provide detailed images of the colon without radiation exposure.
Differential Diagnosis
Because ulcerative colitis shares symptoms with other gastrointestinal conditions, doctors must carefully rule out conditions such as Crohn’s disease, celiac disease, or infections like Clostridioides difficile.
Treatment of Ulcerative Colitis
While ulcerative colitis has no known cure, treatments aim to reduce inflammation, control symptoms, and improve quality of life. The best approach varies from patient to patient, depending on disease severity, response to medications, and lifestyle factors.
Medications
- Aminosalicylates (5-ASAs): These anti-inflammatory drugs, such as mesalamine and sulfasalazine, are often the first line of treatment for mild to moderate UC. They work directly on the lining of the colon to reduce inflammation.
- Corticosteroids: Powerful anti-inflammatory drugs like prednisone are used for short-term management of moderate to severe flare-ups. Because of their significant side effects, they are not recommended for long-term use.
- Immunomodulators: Drugs like azathioprine and 6-mercaptopurine suppress the immune system to prevent it from attacking the colon. These are often prescribed when 5-ASAs and corticosteroids are insufficient.
- Biologic therapies: Biologics are advanced treatments that target specific molecules involved in inflammation. Examples include anti-TNF agents (infliximab, adalimumab), anti-integrin drugs (vedolizumab), and anti-interleukin drugs (ustekinumab). These therapies have revolutionized treatment, offering hope to patients with severe or resistant UC.
- Janus kinase (JAK) inhibitors: Oral drugs like tofacitinib target signaling pathways that drive inflammation. They offer an alternative for patients who do not respond to biologics.
Lifestyle and Dietary Management
While diet does not cause ulcerative colitis, managing food intake can reduce symptoms and improve comfort. Patients may work with dietitians to identify trigger foods, maintain adequate nutrition, and avoid deficiencies. Stress management techniques, regular exercise, and sufficient sleep also contribute to overall well-being.
Surgery
For some patients, surgery becomes necessary when medications fail or complications arise. Surgical options include proctocolectomy, the removal of the colon and rectum. Often, this is followed by the creation of an ileal pouch-anal anastomosis (IPAA), which allows waste to pass through the anus without the need for a permanent ostomy bag.
Surgery can be life-changing, effectively eliminating ulcerative colitis, but it comes with its own challenges and adjustments.
Living With Ulcerative Colitis
Life with ulcerative colitis is not defined only by symptoms and medical procedures. It is also about resilience, adaptation, and advocacy. Patients often face stigma or misunderstanding because their condition is invisible to others, yet it deeply affects daily life.
Support groups, counseling, and strong healthcare partnerships empower patients to navigate the ups and downs. Advances in medicine continue to expand treatment options, and research into the gut microbiome and immune system promises new breakthroughs in the years ahead.
Conclusion: Finding Balance in the Midst of Uncertainty
Ulcerative colitis is a condition that intertwines the biological and the emotional, the physical and the social. Its causes are complex, its symptoms unpredictable, and its treatments varied. Yet, through science and human resilience, patients are finding ways to live full lives, even in the face of chronic illness.
Understanding ulcerative colitis means more than memorizing its symptoms or treatments. It means seeing the human story behind the disease—the courage of those living with it, the dedication of researchers seeking answers, and the hope that tomorrow will bring even better ways to heal.
Ulcerative colitis is not the end of the story for those diagnosed. It is a challenge, yes, but also an opportunity to discover strength, adaptability, and the unwavering drive to live fully.