There are days when tiredness feels ordinary—after a long work shift, an intense workout, or a sleepless night. But imagine waking up every single day with a crushing weight of fatigue that no amount of rest can relieve. Imagine simple tasks, like brushing your teeth or walking to the kitchen, leaving you drained as if you had run a marathon. Imagine your body and mind refusing to cooperate, while the world expects you to function as though nothing is wrong.
This is the reality for people living with Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME). It is an illness that doesn’t always leave visible marks, yet it can dismantle lives from the inside out. The invisibility of the condition often leads to misunderstanding, skepticism, and stigma, making patients feel not only physically exhausted but also emotionally isolated.
CFS/ME is not “just being tired.” It is a complex, multi-system illness that disrupts the nervous system, immune system, and metabolism. Its exact cause remains elusive, but its impact is undeniable. Millions of people worldwide live in the shadow of this condition, often struggling for recognition, validation, and adequate care.
In this article, we will dive into the scientific understanding of CFS/ME, exploring its causes, symptoms, diagnosis, and treatment. Along the way, we will not only examine the medical facts but also acknowledge the human experience of living with a condition that challenges both science and society.
What Is Chronic Fatigue Syndrome?
CFS/ME is a long-term illness characterized by overwhelming fatigue that does not improve with rest and is worsened by physical or mental activity. The defining feature is post-exertional malaise (PEM)—a worsening of symptoms after even minor exertion, often delayed by 24–48 hours. Patients may also experience cognitive difficulties (“brain fog”), pain, sleep disturbances, and other systemic symptoms.
Unlike ordinary fatigue, which resolves after rest or sleep, the exhaustion of CFS/ME lingers, unpredictable and unrelenting. It interferes with daily activities, making work, school, and social life nearly impossible for many.
The illness affects people of all ages, races, and genders, though it is most commonly diagnosed in women between the ages of 40 and 60. Estimates suggest that between 17–24 million people worldwide may have CFS/ME, though many remain undiagnosed.
The Search for Causes
One of the greatest challenges in understanding CFS/ME is its unclear origin. Researchers agree it is a multifactorial condition, likely triggered by a combination of genetic, environmental, and biological factors.
Viral and Infectious Triggers
A significant proportion of patients report the onset of CFS/ME after an infection. Viruses such as Epstein-Barr virus (EBV), which causes mononucleosis, have been closely linked. Other pathogens—including enteroviruses, human herpesvirus 6 (HHV-6), and even bacterial infections like Lyme disease—are also suspected.
These infections may not directly cause CFS/ME but could trigger long-term changes in the immune system, leaving the body stuck in a state of chronic dysfunction.
Immune System Dysregulation
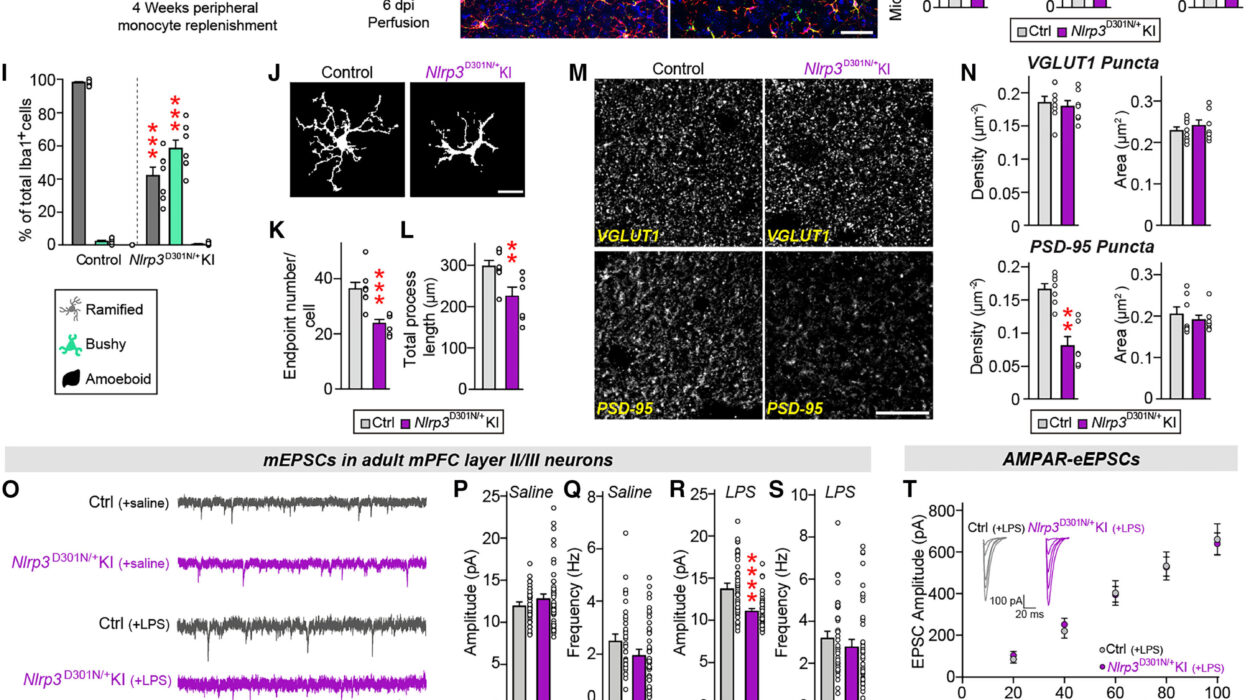
Studies reveal that many patients show abnormalities in immune function, such as elevated inflammatory markers, altered cytokine levels, and impaired natural killer (NK) cell activity. These findings suggest that the immune system may remain overactive or misdirected long after the initial infection has resolved, perpetuating symptoms.
Nervous System Involvement
The autonomic nervous system (ANS)—which regulates involuntary functions like heart rate, blood pressure, and digestion—appears disrupted in CFS/ME. This dysfunction, known as dysautonomia, may explain symptoms such as dizziness, lightheadedness, and rapid heartbeat when standing (a condition called postural orthostatic tachycardia syndrome, or POTS, often overlaps with CFS/ME).
Mitochondrial and Metabolic Abnormalities
The body’s energy factories—the mitochondria—have come under scrutiny in CFS/ME research. Some studies suggest that mitochondrial dysfunction may impair the body’s ability to produce and utilize energy efficiently, leading to the hallmark fatigue and PEM.
Genetic and Epigenetic Factors
Genetic predisposition likely plays a role, as CFS/ME sometimes clusters in families. Epigenetic changes—alterations in gene expression caused by environmental influences—may also contribute, turning certain genes “on” or “off” in ways that sustain illness.
Psychological Stress and Trauma
Though not a direct cause, psychological stress, trauma, or significant life events may act as triggers or exacerbating factors, interacting with biological vulnerabilities to set the illness in motion. Importantly, CFS/ME is not “all in the head,” but the brain-body connection likely plays a role in its complex development.
The Symptoms: More Than Fatigue
The most striking feature of CFS/ME is relentless fatigue, but this alone does not capture the breadth of the illness. Patients often describe their experience as a body-wide collapse affecting every system.
Post-Exertional Malaise (PEM)
This is the hallmark symptom. After even minor exertion—physical, mental, or emotional—patients experience a worsening of symptoms that can last days, weeks, or longer. For some, a short walk or reading a few pages can trigger a crash.
Cognitive Dysfunction (“Brain Fog”)
Many patients struggle with memory, attention, processing speed, and word-finding difficulties. This cognitive cloudiness can make reading, problem-solving, or even following conversations extremely difficult.
Sleep Disturbances
Ironically, patients with CFS/ME often do not feel refreshed even after long hours of sleep. Insomnia, unrefreshing sleep, and disrupted circadian rhythms are common.
Pain
Muscle aches, joint pain, and headaches often accompany the fatigue. Some patients report widespread pain resembling fibromyalgia.
Autonomic Symptoms
Dizziness, palpitations, fainting, and intolerance to standing are frequent, often linked to dysautonomia and overlapping conditions like POTS.
Immune and Flu-Like Symptoms
Sore throats, tender lymph nodes, and heightened sensitivity to infections can occur, making patients feel perpetually as though they are fighting off an illness.
Sensory Sensitivities
Many people with CFS/ME become hypersensitive to light, sound, temperature, or even touch, further complicating daily life.
The severity of symptoms varies widely—from those able to manage part-time work to those bedbound, reliant on caregivers for basic needs.
The Diagnostic Challenge
Diagnosing CFS/ME is notoriously difficult. There is no single test or biomarker; instead, it is a diagnosis of exclusion, made by carefully ruling out other conditions with similar symptoms.
Diagnostic Criteria
Several criteria sets exist, including the Fukuda criteria (1994), the Canadian Consensus Criteria (2003), and the Institute of Medicine (IOM) criteria (2015). The IOM criteria emphasize three core features:
- Substantial reduction in activities due to fatigue lasting at least six months.
- Post-exertional malaise.
- Unrefreshing sleep.
Additionally, patients must experience either cognitive impairment or orthostatic intolerance.
Excluding Other Conditions
Doctors must rule out illnesses such as thyroid disorders, anemia, autoimmune diseases, sleep apnea, depression, and certain cancers. Because of this process, diagnosis often takes years, prolonging patient suffering and uncertainty.
The Problem of Medical Skepticism
One of the greatest burdens patients face is not only their illness but also disbelief. For decades, CFS/ME was dismissed as psychosomatic or “all in the mind.” Though scientific understanding has advanced, stigma and misunderstanding remain, leading to delayed or inadequate care.
Treatment and Management
There is currently no cure for CFS/ME, but treatments aim to reduce symptoms, improve quality of life, and help patients manage their energy.
Pacing and Energy Management
Perhaps the most important strategy is pacing—a method of balancing activity and rest to avoid triggering PEM. Patients learn to recognize their limits, using techniques such as the “energy envelope” model to conserve energy.
Sleep Support
Improving sleep quality is a common goal. Doctors may recommend sleep hygiene practices, cognitive behavioral therapy for insomnia (CBT-I), or in some cases, medications to regulate sleep patterns.
Pain and Symptom Relief
Over-the-counter or prescription medications may help manage pain, headaches, and muscle aches. Some patients benefit from low-dose antidepressants or anticonvulsants for neuropathic pain.
Autonomic Dysfunction Treatments
For those with POTS or orthostatic intolerance, strategies include increased fluid and salt intake, compression garments, and medications to stabilize heart rate and blood pressure.
Experimental and Emerging Therapies
Research into antiviral drugs, immune-modulating therapies, and mitochondrial support continues. Some patients report improvement with supplements such as coenzyme Q10 or L-carnitine, though evidence is mixed.
Psychological and Social Support
Living with CFS/ME is emotionally taxing. Therapy, support groups, and counseling can help patients and families cope, though these should never be framed as “cures.” Validation and understanding are powerful medicines in themselves.
The Human Impact
Beyond biology and medicine, CFS/ME profoundly affects identity, relationships, and hope. Careers end abruptly. Education is interrupted. Friendships fade under the strain of canceled plans and invisible symptoms. Families become caregivers, navigating uncertainty and grief.
Patients often describe a “before and after” life—the person they once were and the shadow they live as now. And yet, resilience shines through. Many become advocates, writers, and voices for change, transforming their suffering into a call for recognition and research.
The Future of CFS/ME Research
Scientific interest in CFS/ME has grown in recent years, particularly after the COVID-19 pandemic. Many patients with long COVID experience symptoms strikingly similar to CFS/ME, reigniting attention and funding for research.
Future directions include:
- Biomarker discovery: Identifying blood-based or imaging markers to improve diagnosis.
- Immune modulation therapies: Targeting inflammation and immune dysfunction.
- Metabolic interventions: Supporting mitochondrial health and cellular energy.
- Neuroimaging studies: Understanding brain inflammation and connectivity.
The hope is that unraveling CFS/ME will not only help millions of patients but also deepen our understanding of chronic illness and the mind-body connection.
A Journey Toward Recognition
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis is more than a medical condition; it is a human struggle at the crossroads of science, society, and compassion. For decades, patients have lived in the shadows, battling both their bodies and disbelief. But the tides are shifting. As research expands and awareness grows, the story of CFS/ME is becoming one not only of suffering but of resilience and progress.
Health is not simply the absence of disease—it is the ability to live fully, to participate in the world, to feel connected and whole. For those with CFS/ME, this remains a distant dream. Yet with science, empathy, and advocacy, we can move closer to a future where the weight of exhaustion no longer defines their lives.