Panic attacks are one of the most intense, terrifying experiences a person can endure. They come suddenly, often without warning, engulfing the sufferer in overwhelming waves of fear, physical distress, and a suffocating sense of doom. To an outsider, panic attacks may seem like exaggerated anxiety or a momentary lapse of composure. But for those who live through them, they are very real and life-altering episodes. The question that haunts many is: what exactly is happening inside the brain during a panic attack? How does a cascade of neurons and chemicals transform ordinary moments into crises of survival, even when no actual danger exists?
Exploring the science behind panic attacks reveals not only the intricate workings of the brain’s fear circuitry but also the delicate balance of chemistry and cognition that sustains our emotional lives. This article takes you deep inside the brain during a panic attack, illuminating the biological, psychological, and evolutionary forces that underlie this powerful experience.
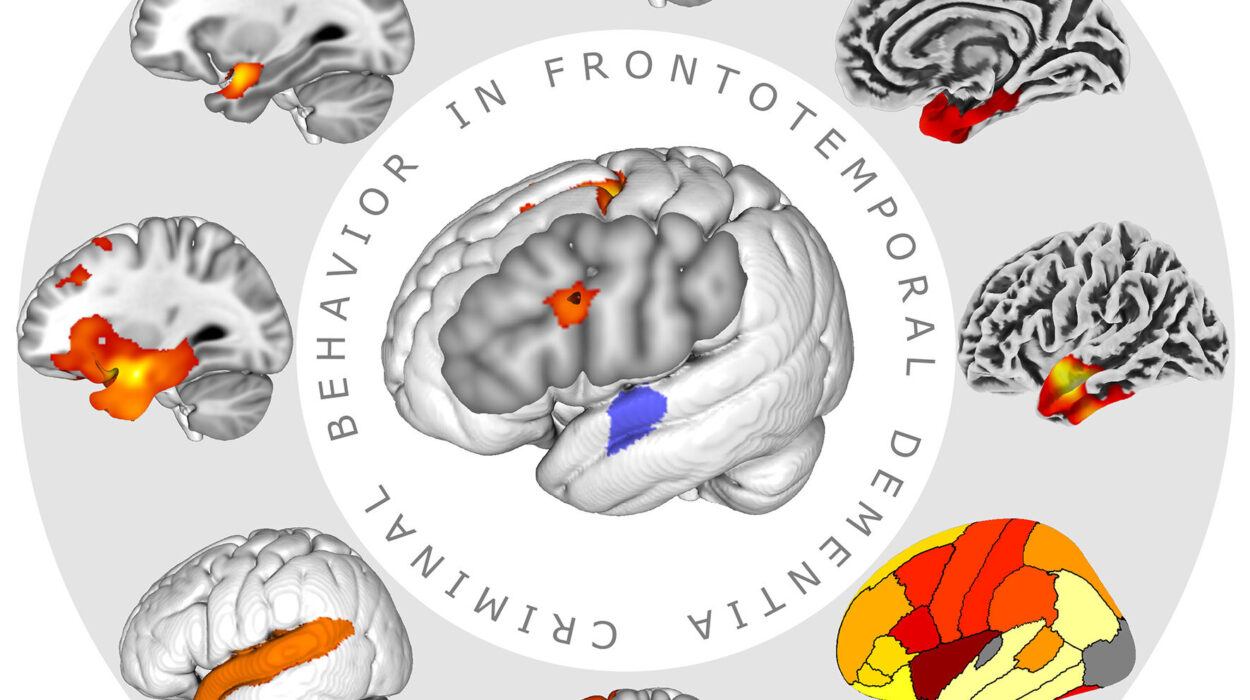
The Anatomy of Fear: The Brain’s Alarm System
To understand panic attacks, one must first appreciate the brain’s fundamental role in detecting and responding to threats. At the heart of this response is the amygdala, a small almond-shaped structure buried deep within the temporal lobes. The amygdala acts like an ancient sentinel, constantly scanning sensory input for signs of danger. When a threat is perceived—whether it’s a real predator or a looming social embarrassment—the amygdala springs into action.
It sends a signal to other parts of the brain, including the hypothalamus, which activates the autonomic nervous system. This system governs the fight-or-flight response, releasing stress hormones like adrenaline and cortisol into the bloodstream. The body reacts with rapid heart rate, increased blood flow to muscles, and a burst of energy, preparing to either confront or flee from danger. This response evolved over millions of years to protect our ancestors from immediate physical threats.
Yet in a panic attack, this alarm system is triggered without an obvious external cause. The amygdala misfires, sounding the alarm in a harmless situation. This false alarm feels devastatingly real to the sufferer. The brain’s intricate balance between danger detection and safety assessment breaks down, plunging the person into acute fear.
The Role of the Amygdala: The Epicenter of Panic
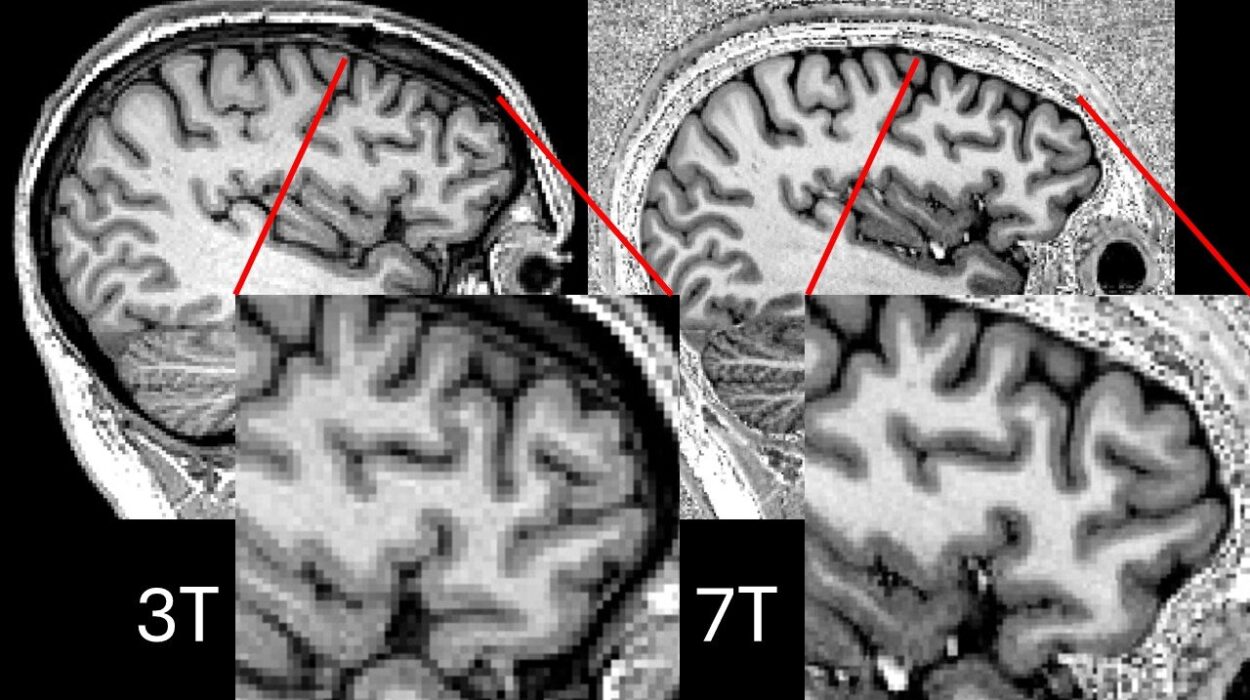
While the amygdala’s role in fear is well-established, its specific involvement in panic attacks has been illuminated by decades of neuroscientific research. Imaging studies using functional MRI have shown hyperactivity in the amygdala during panic attacks. This heightened activity correlates with the intense feelings of terror and physical symptoms experienced.
The amygdala also interacts closely with the hippocampus, a region responsible for memory formation and contextualizing experiences. In a healthy brain, the hippocampus helps regulate fear by distinguishing between real threats and safe environments. During a panic attack, this regulatory function can falter, leaving the amygdala unchecked.
Moreover, the prefrontal cortex—responsible for rational thought and decision-making—normally exerts a calming influence on the amygdala. But in panic attacks, the communication between the prefrontal cortex and the amygdala is impaired, diminishing the brain’s ability to rationalize fear and calm the alarm system.
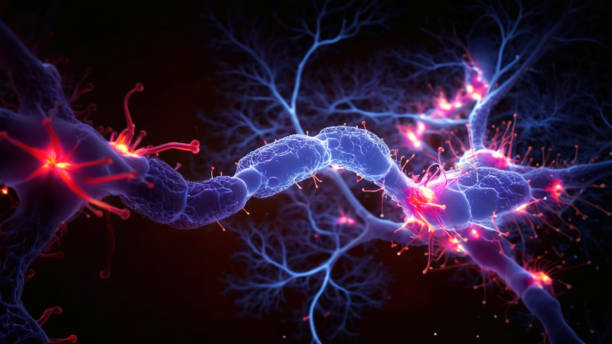
Neurochemistry of Panic: The Brain’s Chemical Symphony Disrupted
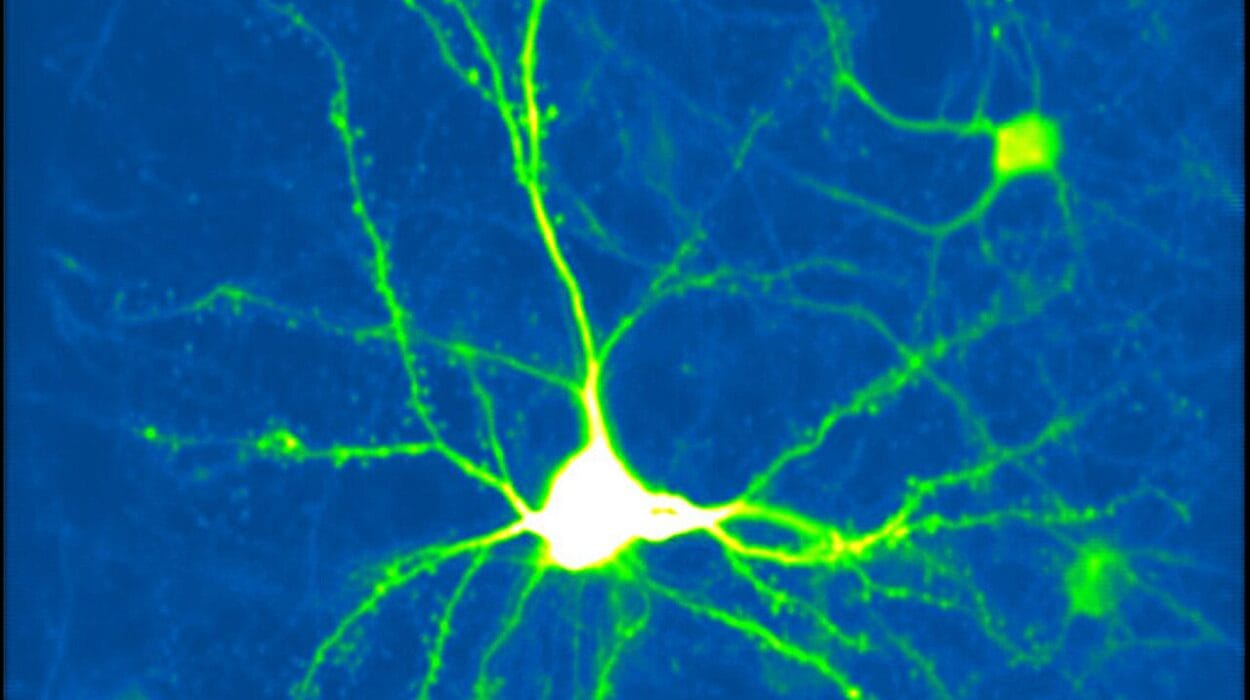
Beneath the electrical activity of neurons lies a complex web of chemicals that modulate brain function. Neurotransmitters are the brain’s messengers, transmitting signals from one neuron to another. Several key neurotransmitters play vital roles in panic attacks.
Gamma-aminobutyric acid (GABA) is the brain’s primary inhibitory neurotransmitter. It functions like a brake pedal, slowing down neural activity and promoting calm. Research shows that reduced GABA activity is linked to anxiety disorders and panic attacks. When GABA’s calming influence weakens, the brain becomes more prone to overreacting to perceived threats.
Conversely, neurotransmitters like norepinephrine and serotonin are deeply involved in mood regulation and the stress response. During a panic attack, norepinephrine surges, contributing to heightened arousal and vigilance. Serotonin’s role is more complex; imbalances in serotonin pathways are associated with anxiety and panic, which is why many effective medications target serotonin receptors.
The balance of these chemicals is delicate. Disruptions caused by genetics, stress, trauma, or even diet can tilt the scales toward a brain state primed for panic.
The Autonomic Nervous System: Body and Brain in Panic
Panic attacks don’t just affect the mind—they flood the body with sensations so intense they often mimic life-threatening emergencies like heart attacks. This is because the autonomic nervous system (ANS) is deeply intertwined with the brain’s panic circuitry.
The ANS has two branches: the sympathetic nervous system, which activates fight-or-flight, and the parasympathetic nervous system, which promotes rest and recovery. In a panic attack, the sympathetic nervous system hijacks control, causing the heart to race, breathing to quicken, muscles to tense, and sweat glands to activate.
The surge of adrenaline triggers these physical symptoms as the body prepares to flee or fight. But since there is no real external threat, these physical responses amplify feelings of fear, creating a vicious cycle. The brain interprets the bodily sensations—like chest tightness or dizziness—as confirmation of impending doom, intensifying the panic.
The Psychological Dimension: How Thoughts and Perceptions Fuel Panic
Though the brain’s biology underpins panic attacks, the psychological experience is equally critical. Cognitive models of panic emphasize how catastrophic misinterpretations of bodily sensations trigger and maintain attacks.
Imagine feeling your heart race. To someone without panic disorder, this might be attributed to exercise or excitement. But for someone prone to panic, it may be interpreted as a sign of a heart attack or loss of control. This “fear of fear” magnifies anxiety and primes the brain to enter a full-blown panic state.
This feedback loop involves the interplay between the brain’s sensory input, emotional processing centers, and higher cognitive areas responsible for interpretation. When the brain perceives a mismatch between expected safety and internal sensations, it can spiral into panic.
Genetic and Environmental Factors: The Roots of Panic Vulnerability
Panic attacks don’t arise in a vacuum. Both genetic predisposition and environmental stressors shape the brain’s vulnerability to panic. Twin studies show that genetics account for a significant portion of the risk for panic disorder, though no single gene dictates the outcome. Instead, multiple genes interact to influence neurotransmitter systems and brain circuitry.
Early life experiences also leave deep marks. Childhood trauma, chronic stress, or experiences of loss and instability can sensitize the brain’s fear system. This heightened sensitivity makes the amygdala more reactive and the prefrontal cortex less effective at controlling fear responses.
Moreover, stressful life events in adulthood—like job loss, illness, or relationship breakdown—can precipitate panic attacks in susceptible individuals. This complex interplay of nature and nurture shapes the landscape in which panic attacks occur.
The Brain’s Plasticity: Hope for Recovery and Resilience
Though panic attacks are terrifying, the brain is remarkably adaptable. Neuroplasticity—the ability of the brain to reorganize itself—offers hope for those struggling with panic.
Therapies such as cognitive-behavioral therapy (CBT) work by retraining the brain’s response to fear. CBT helps patients recognize and challenge catastrophic thoughts, reducing the amygdala’s hyperactivity and strengthening the prefrontal cortex’s regulatory control. Through repeated exposure and cognitive restructuring, the brain learns to distinguish harmless bodily sensations from true threats.
Medications like selective serotonin reuptake inhibitors (SSRIs) restore chemical balance and calm overactive neural circuits. Together, therapy and medication can reshape the brain’s panic pathways, breaking the cycle of fear.
The Evolutionary Paradox: Why Does the Brain Misfire?
From an evolutionary perspective, the brain’s tendency to panic in the absence of real threats might seem like a flaw. Yet this misfiring reflects the brain’s “better safe than sorry” approach.
In ancient environments, failing to respond quickly to a real threat was far more dangerous than overreacting to a false alarm. This bias towards hypersensitivity ensured survival. However, in the modern world—where dangers are often psychological rather than physical—this once-useful mechanism can backfire, trapping individuals in relentless cycles of panic.
Understanding this paradox can help sufferers cultivate compassion for their own brains, recognizing panic as a misdirected survival tool rather than a personal failing.
Living with Panic: The Human Experience Behind the Neuroscience
Beyond the neurons and chemicals lies the lived reality of those who endure panic attacks. The experience is deeply isolating, as panic often strikes unpredictably and without clear cause. Many suffer in silence, afraid of stigma or misunderstanding.
The sheer terror can disrupt daily life, making ordinary activities like driving, shopping, or socializing daunting. The brain’s malfunction creates a prison of fear where freedom feels elusive.
Yet, with knowledge, support, and treatment, many reclaim their lives. They learn that panic is not permanent and that their brains can be rewired towards calm and safety. This journey is both scientific and profoundly human—a testament to resilience in the face of the brain’s own betrayals.
Conclusion: The Brain’s Enigma of Panic
What happens in the brain during a panic attack is a complex symphony of biology, chemistry, cognition, and emotion. It reveals how finely tuned yet fragile our internal alarm systems are. The amygdala’s alarm, the chemical imbalances, the racing heart, and the spiraling thoughts together create an experience that feels like a brush with death, even when death is nowhere near.
Yet understanding these processes offers not just explanation, but empowerment. It transforms panic from a mysterious terror into a biological phenomenon that can be treated, managed, and overcome. At its core, the story of panic attacks is a story about the brain’s remarkable power and vulnerability—its ceaseless effort to keep us safe, even when that effort sometimes goes awry.