Multiple sclerosis (MS) is a disease that often hides in plain sight, striking in unpredictable ways. It is a chronic condition where the body’s own immune system mistakenly turns against itself, targeting the central nervous system—the brain and spinal cord. For those living with MS, life can become a constant negotiation with fatigue, pain, and neurological changes that can appear suddenly and evolve over time.
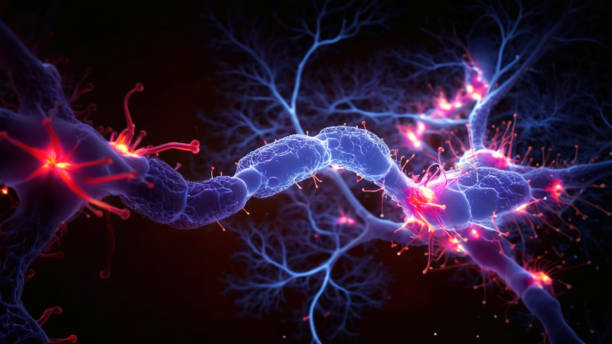
The name multiple sclerosis itself tells a story. Sclerosis refers to the scarring or hardening of tissue, while multiple points to the many places in the nervous system where this damage can occur. When the immune system attacks the protective covering of nerve fibers (myelin), communication between the brain and the body is disrupted, leading to a wide array of symptoms.
Living with MS is not just about managing symptoms but about confronting uncertainty. Will today bring numbness in the legs? Will vision blur? Will fatigue make it impossible to go to work or play with children? These questions illustrate the profound impact MS can have on quality of life. And yet, with advancing research, better treatments, and stronger awareness, many people with MS are living full and meaningful lives despite the challenges.
To truly understand MS, we need to explore its causes, symptoms, diagnostic processes, and treatments, weaving together scientific knowledge with the human experience.
The Causes of Multiple Sclerosis: A Complex Puzzle
The Role of the Immune System
MS is classified as an autoimmune disease. In a healthy immune system, specialized cells defend the body against bacteria, viruses, and other invaders. But in MS, these same defenders become attackers, targeting the myelin sheath that insulates and protects nerve fibers. Without intact myelin, nerve signals slow down or stop altogether.
Why does the immune system make this mistake? Scientists do not yet have a complete answer. Unlike some conditions with a single clear cause, MS seems to arise from a complex interplay of genetic, environmental, and lifestyle factors.
Genetic Susceptibility
Genetics plays a role in predisposing someone to MS, though it is not inherited in a straightforward manner like eye color or blood type. Having a close relative with MS increases risk, but the probability remains relatively low. Researchers have identified variations in certain genes—particularly those related to immune function—that may increase susceptibility. However, genes alone are not enough; many people with these variations never develop MS.
Environmental Influences
Environmental factors are believed to act as triggers in genetically predisposed individuals. Several key influences have been identified:
- Geographic location: MS is more common in regions farther from the equator. Sunlight exposure, and therefore vitamin D levels, may influence risk, as vitamin D is known to play a role in immune regulation.
- Infections: Certain viruses, especially the Epstein-Barr virus (EBV), have been strongly linked to MS. Nearly all adults are exposed to EBV, but in susceptible individuals, the virus may alter the immune system in ways that increase MS risk.
- Smoking: Smoking has been shown to not only increase the risk of developing MS but also accelerate its progression.
- Obesity and diet: Studies suggest that obesity, especially in adolescence, may increase risk, possibly through chronic inflammation and hormonal effects.
A Multifactorial Condition
No single factor explains MS. It is best understood as the result of overlapping influences: genes create a foundation of risk, environmental exposures provide the triggers, and the immune system responds in ways that damage the nervous system. This complexity is one reason why predicting who will develop MS remains so difficult.
Symptoms of Multiple Sclerosis: The Many Faces of the Disease
MS is often called a “snowflake disease” because no two people experience it in exactly the same way. Symptoms vary widely depending on which parts of the central nervous system are affected. They may appear suddenly, improve, then return again, making MS unpredictable and often frustrating.
Early Symptoms
The first signs of MS are often subtle and easy to dismiss, such as numbness in a limb or blurry vision. These symptoms may disappear for months or years before returning, leading some people to delay seeking medical advice.
Common early symptoms include:
- Vision problems such as blurred or double vision, pain with eye movement, or temporary loss of sight.
- Numbness or tingling in the face, arms, or legs.
- Weakness in limbs, often noticeable when walking or climbing stairs.
- Balance issues or dizziness.
Common Ongoing Symptoms
As the disease progresses, symptoms can become more persistent and varied:
- Fatigue: One of the most common and disabling symptoms, MS-related fatigue is not simply feeling tired; it is an overwhelming exhaustion that can strike even after rest.
- Muscle weakness and spasticity: Damage to nerve pathways can cause stiffness, spasms, and difficulty moving.
- Cognitive changes: Problems with memory, attention, or processing information can develop, affecting daily life and work.
- Pain: MS can cause neuropathic pain (from nerve damage) as well as musculoskeletal pain due to mobility challenges.
- Bladder and bowel dysfunction: Nerve damage may disrupt normal control, leading to urgency, frequency, or constipation.
- Mood disorders: Depression and anxiety are common, partly due to the neurological effects of MS and partly from the emotional burden of living with a chronic disease.
Types of MS and Symptom Patterns
The course of MS varies, and researchers classify it into several types:
- Relapsing-remitting MS (RRMS): The most common form, characterized by periods of new or worsening symptoms (relapses) followed by recovery (remissions).
- Secondary progressive MS (SPMS): Some people with RRMS eventually transition to SPMS, where symptoms steadily worsen with fewer remissions.
- Primary progressive MS (PPMS): About 10–15% of patients experience a gradual worsening of symptoms from the beginning, without distinct relapses.
- Progressive-relapsing MS (PRMS): A rare form marked by steady progression with superimposed relapses.
The unpredictability of these patterns makes living with MS particularly challenging.
Diagnosis: Unraveling the Mystery
Diagnosing MS can be a lengthy and complex process. There is no single test that confirms it; instead, doctors rely on a combination of medical history, neurological examinations, imaging, and laboratory tests.
Neurological Examination
The diagnostic journey usually begins with a detailed clinical history and neurological exam. A neurologist will ask about symptoms, their duration, and any patterns of progression. They will also test reflexes, muscle strength, coordination, balance, and vision to look for evidence of nervous system involvement.
Magnetic Resonance Imaging (MRI)
MRI is the most powerful tool for diagnosing MS. It can reveal lesions or plaques—areas of damaged myelin—in the brain and spinal cord. The presence of multiple lesions in different areas and at different times strongly supports an MS diagnosis.
Lumbar Puncture (Spinal Tap)
A lumbar puncture may be performed to analyze cerebrospinal fluid for signs of immune system activity, such as oligoclonal bands, which are often present in people with MS.
Evoked Potentials
These tests measure the brain’s electrical responses to sensory stimuli, such as visual patterns or sound. Delayed responses can indicate slowed nerve conduction due to myelin damage.
Ruling Out Other Conditions
Because many other diseases can mimic MS symptoms—such as Lyme disease, lupus, or vitamin B12 deficiency—doctors must carefully rule out alternative explanations before confirming the diagnosis.
Treatment: Managing MS in a Modern World
There is currently no cure for MS, but treatments can significantly alter its course, reduce relapses, manage symptoms, and improve quality of life. The treatment approach is multifaceted, involving disease-modifying therapies, symptom management, lifestyle adjustments, and emotional support.
Disease-Modifying Therapies (DMTs)
DMTs are the cornerstone of MS treatment. These medications target the immune system to reduce the frequency and severity of relapses, slow progression, and limit new lesion formation.
Examples include:
- Injectable therapies: Interferon beta and glatiramer acetate.
- Oral medications: Fingolimod, dimethyl fumarate, teriflunomide.
- Infused therapies: Natalizumab, ocrelizumab, alemtuzumab.
Each has its own risks and benefits, and treatment choice depends on disease type, severity, and individual patient factors.
Managing Relapses
When relapses occur, high-dose corticosteroids are often used to reduce inflammation and speed recovery. Plasma exchange may be considered for severe relapses unresponsive to steroids.
Symptom Management
Because MS symptoms vary so widely, treatment must be personalized. Approaches may include:
- Medications for spasticity, pain, bladder issues, or depression.
- Physical therapy to maintain mobility and strength.
- Occupational therapy to support daily activities.
- Cognitive therapy for memory and attention difficulties.
Lifestyle and Holistic Approaches
Lifestyle factors play a vital role in supporting overall health and potentially influencing disease progression. Regular exercise, a balanced diet, stress management, and adequate sleep can all improve resilience. Vitamin D supplementation is often recommended, given its potential role in immune regulation.
Mind-body practices such as yoga, mindfulness, and meditation may also help manage fatigue, mood changes, and pain.
Emotional and Social Support
Living with MS can be emotionally taxing, both for individuals and their families. Counseling, support groups, and open communication are essential for maintaining mental health. The sense of belonging to a community of others facing similar challenges can bring hope and strength.
The Human Experience of MS
Beyond medical definitions and treatment plans, MS is deeply personal. Each individual’s story reflects resilience, adaptation, and courage. Some continue to work, travel, and pursue passions, while others face greater physical limitations. For many, MS reshapes not just health but also identity, relationships, and future plans.
The unpredictability of the disease—its “invisible symptoms” like fatigue or cognitive changes—can make it harder for others to understand. Yet, the rise of advocacy groups, research organizations, and patient voices is helping to bring greater awareness and empathy.
Hope on the Horizon: Advances in Research
Research into MS is advancing rapidly. Scientists are exploring new therapies that go beyond modifying the immune system to actually repair or regenerate damaged myelin. Stem cell therapies, remyelination strategies, and genetic approaches hold promise for the future.
Biomarkers that predict disease course are also under investigation, which could enable more personalized treatments. Advances in imaging are helping researchers visualize disease progression more clearly.
Perhaps most importantly, the community of patients, caregivers, and researchers is stronger and more connected than ever. This shared determination is fueling hope that one day, MS will be not just treatable but curable.
Living with MS: Redefining Strength
Multiple sclerosis is not an easy journey, but it is not a hopeless one. It challenges the body, the mind, and the spirit, but it also reveals the extraordinary strength of those who live with it. Science continues to move forward, offering better tools for treatment and management. And alongside science, compassion, support, and resilience make it possible for people with MS to live meaningful, fulfilling lives.
Health is never just about the absence of disease—it is about the presence of vitality, purpose, and connection. For those with MS, this truth is lived every day.