For decades, cancer has remained one of humanity’s most formidable challenges, claiming millions of lives each year. While science has made tremendous progress in diagnosing and treating many types of cancer, therapies for solid tumors—like breast, prostate, lung, and ovarian cancer—have lagged behind. These cancers account for nearly 90% of all cases worldwide, making the lack of effective targeted treatments one of the greatest obstacles in modern oncology.
Among the most promising innovations in recent years is chimeric antigen receptor (CAR) T cell therapy. This remarkable approach harnesses a patient’s own immune system to fight disease, reprogramming T cells—the body’s frontline fighters—into precision weapons against cancer. For blood cancers such as certain types of leukemia and lymphoma, CAR T cell therapy has delivered stunning results, sometimes achieving remissions when no other treatment could. But against solid tumors, this strategy has stumbled, often falling short because the tumor environment itself is hostile and resistant.
Now, a collaborative research effort between the USC Norris Comprehensive Cancer Center and City of Hope has unveiled a new strategy that could finally tip the balance. By re-engineering CAR T cells to release a powerful fusion protein directly into tumors, the scientists may have found a way to unlock CAR T therapy’s potential for a much broader range of cancers.
Cracking the Solid Tumor Puzzle
The central problem with treating solid tumors lies in their microenvironment. Unlike blood cancers, which circulate in the body and are more accessible to immune cells, solid tumors are surrounded by dense, complex tissue that makes it difficult for T cells to enter. Even when T cells reach the tumor, they often find themselves trapped in an environment designed to suppress them. The tumor essentially creates a fortress, filled with biological signals that tell immune cells to slow down, weaken, or even die off.
Researchers have long sought a way to break through this barrier. One promising candidate has been interleukin 12 (IL-12), a cytokine—or signaling protein—that boosts immune activity and can help T cells regain their strength inside tumors. Yet attempts to use IL-12 have faced a major problem: when released throughout the body, it can trigger dangerous and sometimes fatal levels of inflammation. The challenge, then, has been to find a way to focus IL-12’s power only where it is needed—inside the tumor itself.
A Clever Fusion of Two Weapons
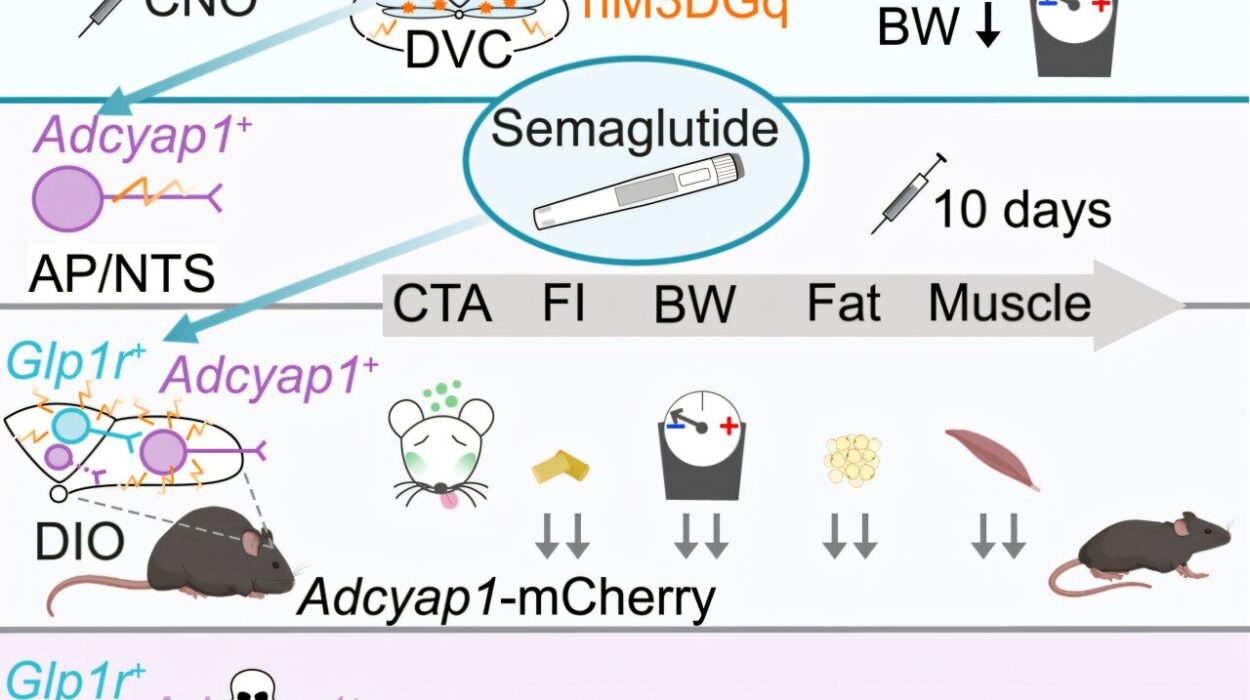
The USC and City of Hope team devised an ingenious solution. They engineered CAR T cells to produce a fusion protein combining IL-12 with a programmed death-ligand 1 (PD-L1) blocker. This is a form of immune checkpoint inhibitor—a therapy already widely used in cancer treatment—which prevents cancer cells from switching off immune attacks.
Here’s why this fusion matters. Many tumors, when confronted by immune cells, release PD-L1 to deactivate them. But by linking IL-12 directly to a PD-L1 blocker, the scientists ensured that IL-12 would be delivered precisely where PD-L1 levels are high—that is, right at the tumor site. In effect, the tumor’s own defense mechanism becomes its weakness: the very act of raising PD-L1 invites the fused IL-12 to accumulate and strengthen the immune attack.
This design not only amplifies the power of CAR T cells but also minimizes the risk of IL-12 causing harm elsewhere in the body. It’s a localized strike, focused on the battlefield where the fight is most urgent.
Remarkable Results in Early Testing
When the researchers tested these engineered CAR T cells in mouse models of prostate and ovarian cancer, the results were striking. The modified cells successfully infiltrated the tumors, reshaped the hostile environment, and triggered dramatic shrinkage of the cancer. Even more encouraging, they did so without unleashing widespread toxicity.
This is significant because safety has always been one of the biggest hurdles for IL-12–based therapies. By keeping its activity localized, the fusion protein allowed researchers to harness IL-12’s benefits while avoiding its dangers. In these early studies, the treatment not only worked—it worked safely.
The findings, published in Nature Biomedical Engineering, suggest a potential path forward for treating cancers that have so far resisted CAR T therapy.
Beyond Prostate and Ovarian Cancer
Although the study focused on prostate and ovarian tumors, the implications extend much further. Solid tumors across the body—whether in the brain, the pancreas, or the gastrointestinal tract—share common features, including their ability to suppress immune activity through checkpoints like PD-L1. That means this approach could be adapted for many different cancer types.
The researchers are already expanding their work, testing the strategy in pancreatic and colorectal cancers, with plans to move into brain tumors as well. Each cancer will need to be studied carefully, since no two are exactly alike, but the principle of harnessing PD-L1 to deliver IL-12 locally may have wide-ranging applications.
If successful, this could represent a new era for CAR T therapy, bringing its transformative power to the majority of cancers, not just a subset.
A Broader Vision for Immune Engineering
Another exciting aspect of this discovery is its potential beyond CAR T cells. The fusion strategy might also be applied to other forms of immune-based therapies, such as tumor-infiltrating lymphocytes or T-cell receptor therapies, which also rely on reactivating immune responses inside tumors. In this sense, the innovation is less about one specific therapy and more about opening a door to a new way of thinking: using tumors’ own defense mechanisms to deliver potent counterattacks.
For patients, this could mean not only more effective treatments but also therapies that are safer and more precisely targeted. For oncologists, it adds a powerful new tool to an expanding arsenal of immunotherapies, which have already revolutionized cancer treatment in the past decade.
Toward the Clinic
As with all scientific breakthroughs, moving from mouse models to human patients will require careful testing. The researchers estimate that clinical trials could begin within the next one to two years, provided safety and efficacy continue to hold up in preclinical studies.
If those trials succeed, the therapy could transform how doctors treat cancers once considered nearly untouchable. Patients facing diseases like pancreatic or brain cancer, which often come with grim prognoses, could someday benefit from therapies that not only attack tumors but do so with precision and minimal collateral damage.
The Human Story Behind the Science
Behind every advance in cancer research is a story of determination, creativity, and hope. The scientists who developed this new CAR T strategy are part of a broader movement—one driven by the belief that cancer’s defenses, no matter how formidable, can be overcome.
For patients and families, the hope is even more personal. Each breakthrough is a reminder that cancer is not invincible, that tomorrow’s treatments can be better, safer, and more effective than today’s. The fight against cancer is not only a scientific challenge but also an emotional journey, filled with setbacks and triumphs, despair and renewal.
This new work reflects the essence of modern oncology: harnessing the body’s own defenses, engineering them to be stronger, smarter, and more precise, and directing them where they are needed most. It’s a vision of medicine not as blunt force, but as a finely tuned collaboration with nature.
A Future Within Reach
The battle against cancer is far from over, but each breakthrough brings us closer to tipping the scales. The fusion of IL-12 and PD-L1 blocking within CAR T cells is not just a clever piece of bioengineering—it is a symbol of progress, creativity, and perseverance in the face of one of humanity’s greatest challenges.
If this strategy fulfills its promise, it could redefine how we approach solid tumors, opening possibilities for treatment across a wide spectrum of cancers. For patients, it offers renewed hope. For researchers, it affirms the power of imagination in science. And for the rest of us, it is a reminder that the fight against cancer is not only about defeating disease, but also about affirming life itself.
More information: Solid tumour CAR-T cells engineered with fusion proteins targeting PD-L1 for localized IL-12 delivery, Nature Biomedical Engineering (2025). DOI: 10.1038/s41551-025-01509-2