The heart is the engine that drives life. From the moment we are born to the moment we take our last breath, the heart beats in a rhythmic dance, a steady pulse that keeps blood flowing through our veins and oxygen circulating through our bodies. But what happens when this rhythm is disrupted? When the heart’s steady beat turns erratic, it can send shockwaves through the body, affecting not just the heart, but the entire organism. This disruption in the heart’s natural rhythm is known as an arrhythmia.
While arrhythmias may sound like a medical term reserved for the most severe of conditions, the truth is that these irregular heartbeats are more common than most people think. In fact, they affect millions of people worldwide. But just because they are common does not mean they are trivial. Arrhythmias can range from being completely benign to life-threatening, and understanding the delicate balance of the heart’s electrical system is key to comprehending why some irregularities matter more than others.
The Heart’s Electrical System: The Conductor of the Beat
Before we can understand arrhythmias, we need to first understand the rhythm itself. The heart’s beat is not a random event. It’s the result of a carefully orchestrated system of electrical signals that flow through the heart, causing it to contract and pump blood. This system is often compared to a symphony, where different sections of the orchestra must play in perfect harmony to create a cohesive, beautiful piece of music.
At the heart of this system is the sinoatrial (SA) node, a small cluster of cells located in the right atrium of the heart. The SA node acts as the natural pacemaker of the heart, initiating electrical impulses that set the rhythm of the heartbeat. These electrical signals travel through the atria (the upper chambers of the heart), causing them to contract and push blood into the ventricles (the lower chambers). Then, the signals pass through the atrioventricular (AV) node, a specialized region that acts as a gatekeeper, delaying the signal slightly before sending it to the ventricles. This delay ensures that the ventricles fill with blood before they contract and pump it to the lungs and the rest of the body.
In a healthy heart, this process happens seamlessly, with electrical signals traveling at a steady pace, creating a regular rhythm. However, when something goes awry with this electrical system, it can lead to an arrhythmia.
What Are Arrhythmias?
An arrhythmia is simply any abnormality in the heart’s rhythm. The term encompasses a wide range of conditions, from occasional skipped beats to life-threatening irregularities. Some arrhythmias are so mild that they are barely noticeable, while others can cause severe symptoms like dizziness, fainting, or even sudden cardiac arrest.
There are several types of arrhythmias, and they are typically categorized based on their location and the nature of the rhythm disturbance. Broadly speaking, arrhythmias can be classified as either tachycardia (a fast heart rate) or bradycardia (a slow heart rate), and they can originate in the atria (the upper chambers of the heart), the ventricles (the lower chambers), or the conduction system itself.
However, this classification is just the tip of the iceberg. The real complexity of arrhythmias lies in their variety and the factors that cause them. Some arrhythmias are congenital, meaning they are present from birth, while others develop later in life due to a variety of causes, such as heart disease, high blood pressure, electrolyte imbalances, or even stress.
Types of Arrhythmias: A Closer Look
When it comes to arrhythmias, the names themselves can be daunting. But to understand these conditions, we must take a closer look at the different types of arrhythmias, their causes, and their potential consequences.
Atrial Fibrillation: The Most Common Arrhythmia
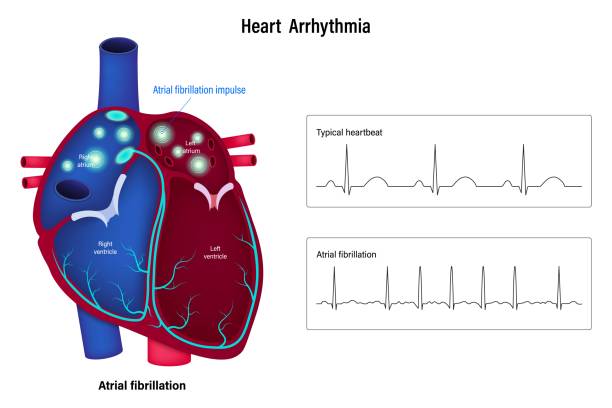
Atrial fibrillation (AFib) is the most common type of arrhythmia, affecting millions of people worldwide. It occurs when the electrical signals in the atria become disorganized, causing the atria to fibrillate or quiver instead of contracting normally. As a result, the blood flow to the ventricles becomes irregular, and the heart rate can become fast and erratic.
AFib can be intermittent or persistent, and while it may not always cause symptoms, it can increase the risk of stroke and other complications. In fact, people with AFib are five times more likely to have a stroke due to the formation of blood clots in the atria. While AFib can be managed with medication, lifestyle changes, and sometimes procedures like catheter ablation, it remains a major concern for those affected.
Ventricular Arrhythmias: The Silent Danger
Ventricular arrhythmias are among the most dangerous types of arrhythmias. They occur when the electrical signals in the ventricles become disordered, leading to irregular or very fast heartbeats. The most well-known form of ventricular arrhythmia is ventricular tachycardia (VT), a condition where the heart beats very quickly and inefficiently, compromising its ability to pump blood effectively.
If left untreated, VT can lead to ventricular fibrillation (VFib), a chaotic, life-threatening rhythm in which the ventricles quiver instead of contracting. VFib is the primary cause of sudden cardiac arrest, and without immediate intervention, it can be fatal. Defibrillation, or the application of an electrical shock to the heart, is often required to restore a normal rhythm in cases of VFib.
Bradycardia: When the Heart Slows Down
While most arrhythmias are associated with an abnormally fast heart rate, some involve a slow heart rate. Bradycardia occurs when the heart beats too slowly—typically fewer than 60 beats per minute. While a slow heart rate is not always problematic (some athletes naturally have slow heart rates due to their fitness level), in others, it can cause symptoms like dizziness, fatigue, and fainting.
In severe cases, bradycardia can lead to a lack of oxygen reaching the brain and other vital organs, potentially resulting in life-threatening complications. A common cause of bradycardia is a malfunction in the SA node, the heart’s natural pacemaker, which can cause the heart to beat too slowly. Treatment for bradycardia may include a pacemaker, a small device implanted under the skin that helps regulate the heart’s rhythm.
The Causes of Arrhythmias
Arrhythmias are not random occurrences; they are often the result of underlying conditions or disruptions to the heart’s electrical system. Understanding the causes of arrhythmias is crucial for both prevention and treatment.
Heart Disease: The Primary Culprit
One of the most common causes of arrhythmias is underlying heart disease. Conditions like coronary artery disease, heart attacks, heart failure, and valve disorders can all contribute to the development of arrhythmias. Damage to the heart muscle or the electrical pathways within the heart can lead to irregular heartbeats.
For instance, after a heart attack, scar tissue can form in the heart muscle, disrupting the normal flow of electrical signals. This can lead to arrhythmias, including life-threatening ones like ventricular tachycardia or ventricular fibrillation. Similarly, heart failure, in which the heart is unable to pump blood efficiently, can increase the risk of arrhythmias due to changes in the heart’s structure and function.
Electrolyte Imbalances: The Heart’s Conductors
The heart’s electrical system depends on a delicate balance of electrolytes, such as potassium, sodium, calcium, and magnesium. These charged particles help transmit electrical signals across the heart muscle. When electrolyte levels become imbalanced—due to dehydration, kidney disease, or certain medications—the heart’s rhythm can become disturbed.
For example, low potassium levels (hypokalemia) can lead to irregular heartbeats, including conditions like atrial fibrillation or premature ventricular contractions. Conversely, high potassium levels (hyperkalemia) can be even more dangerous, leading to potentially fatal arrhythmias like ventricular fibrillation.
Stress and Lifestyle Factors: The Modern Contributors
In today’s fast-paced world, stress has become a significant contributor to heart problems, including arrhythmias. Chronic stress can lead to the release of hormones like adrenaline, which can stimulate the heart and cause irregular rhythms. Similarly, excessive caffeine, alcohol, or drug use can trigger arrhythmias in some individuals. Lifestyle factors such as poor diet, lack of exercise, and smoking also increase the risk of arrhythmias, particularly when they lead to conditions like high blood pressure or obesity.
Diagnosing Arrhythmias: Finding the Beat
Diagnosing an arrhythmia typically begins with a physical exam and a discussion of symptoms. A doctor may listen to the heart with a stethoscope to detect irregularities in the rhythm. However, to pinpoint the exact nature of the arrhythmia, more advanced diagnostic tools are often required.
Electrocardiogram (ECG or EKG)
The electrocardiogram (ECG or EKG) is the most common test used to diagnose arrhythmias. It measures the electrical activity of the heart by placing electrodes on the skin. The resulting graph shows the pattern of electrical signals in the heart, which can reveal abnormalities in rhythm, heart rate, and electrical conduction.
Holter Monitor and Event Monitor
For arrhythmias that are intermittent, a doctor may recommend wearing a Holter monitor or an event monitor. These portable devices continuously record the heart’s electrical activity for an extended period, allowing doctors to capture irregularities that might not appear during a brief ECG.
Treatment Options: Restoring the Rhythm
The treatment of arrhythmias depends on the type of arrhythmia, its severity, and the underlying causes. In some cases, treatment may not be necessary, especially for benign arrhythmias that do not cause symptoms or harm. However, for more serious arrhythmias, several treatment options are available.
Medications
Antiarrhythmic drugs are often prescribed to help control heart rhythms. These medications work by altering the electrical signals in the heart, either slowing down or speeding up the heart rate, or preventing abnormal signals from spreading.
Electrical Cardioversion
For certain types of arrhythmias, electrical cardioversion may be recommended. This procedure involves delivering a brief electrical shock to the heart to reset its rhythm. It is often used to treat atrial fibrillation or atrial flutter.
Pacemakers and Defibrillators
In cases of bradycardia or life-threatening arrhythmias, devices like pacemakers or implantable cardioverter-defibrillators (ICDs) may be used. A pacemaker is a small device implanted under the skin that helps regulate the heart’s rhythm, while an ICD can deliver shocks to the heart if it detects a dangerous arrhythmia, such as ventricular fibrillation.
Catheter Ablation
In some cases, a procedure called catheter ablation may be used to treat arrhythmias. During this procedure, a catheter is inserted into the heart through a blood vessel, and targeted areas of abnormal tissue are destroyed with radiofrequency energy. This can help correct arrhythmias like atrial fibrillation or ventricular tachycardia.
Living with Arrhythmias: A New Rhythm
While arrhythmias can be alarming, many people with these conditions lead full, active lives with proper treatment and management. Lifestyle changes, such as regular exercise, a heart-healthy diet, stress management, and avoiding triggers like excessive caffeine or alcohol, can help reduce the risk of arrhythmias and improve heart health.
In many ways, living with an arrhythmia is about learning to understand the heart’s rhythm and working with it, not against it. With the right treatment and lifestyle adjustments, most people with arrhythmias can continue to live fulfilling lives, keeping their hearts in tune with the rhythms of the world.