Congestive Heart Failure (CHF), often referred to as simply “heart failure,” is a condition that affects millions of people worldwide. Despite its alarming name, heart failure doesn’t mean the heart has stopped beating. Rather, it signifies that the heart is struggling to pump blood as effectively as it should. This weakening of the heart’s ability to perform its crucial function can have serious consequences for the body’s overall health. CHF is not a singular disease, but a complex syndrome with various underlying causes and many layers of symptoms.
The word “congestive” refers to the buildup of fluid that often accompanies heart failure, leading to swelling, shortness of breath, and fatigue. This fluid buildup occurs because the heart’s diminished pumping power results in poor circulation, which affects multiple organ systems. For those living with CHF, the disease can be both physically taxing and emotionally challenging, affecting everything from daily activities to the most intimate relationships.
In this exploration of congestive heart failure, we will break down the condition’s causes, symptoms, progression, and treatment options, all while understanding the science behind how the heart’s weakening can have a ripple effect throughout the body.
What Is Congestive Heart Failure?
At its core, Congestive Heart Failure refers to a condition in which the heart becomes less efficient at pumping blood to meet the body’s needs. This insufficiency may be due to either the heart’s inability to fill with enough blood or its inability to pump enough blood into circulation. The result is a chronic condition that affects the organs and systems dependent on proper blood flow, such as the lungs, liver, and kidneys.
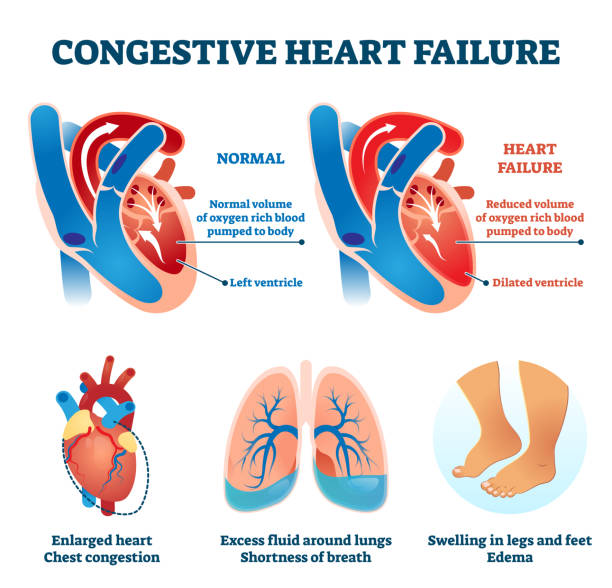
In a healthy heart, the left ventricle pumps oxygen-rich blood to the body, while the right ventricle pumps blood to the lungs for oxygenation. When the heart weakens, this process becomes inefficient, leading to symptoms like fatigue, shortness of breath, and swelling of the extremities. The term “congestive” specifically refers to the buildup of fluids that occurs as a result of this inadequate circulation, which manifests in places like the lungs, abdomen, and legs.
Understanding CHF begins with understanding the heart’s basic function. The heart is essentially a muscular pump. Each time it beats, it sends oxygenated blood to the body’s tissues and organs, and deoxygenated blood to the lungs. However, when the heart can no longer pump effectively, blood begins to pool, leading to congestion. Over time, this congestion can worsen, placing even more strain on the heart.
The Anatomy of Heart Failure
Heart failure can result from a variety of different factors that affect the heart’s structure or function. The heart has four chambers: two atria (upper chambers) and two ventricles (lower chambers). The left ventricle plays a critical role in pumping oxygen-rich blood throughout the body. When this ventricle is impaired, the heart can no longer effectively supply the body with the blood it needs.
There are several conditions that can damage the heart and lead to CHF. These include:
- Coronary Artery Disease (CAD): The most common cause of CHF. CAD occurs when the coronary arteries that supply blood to the heart become narrowed or blocked, reducing blood flow to the heart muscle itself.
- Hypertension (High Blood Pressure): Over time, untreated hypertension can cause the heart to work harder than normal, leading to thickening of the heart muscle and eventually heart failure.
- Cardiomyopathy: This is a disease of the heart muscle itself, which can result from various causes, including alcohol abuse, viral infections, or genetic factors. It weakens the heart muscle, reducing its ability to pump blood effectively.
- Heart Valve Disease: Dysfunctional heart valves can interfere with the flow of blood in and out of the heart, contributing to heart failure.
- Arrhythmias: Abnormal heart rhythms can result in an inefficient pumping of blood, further exacerbating heart failure.
The heart’s ability to pump blood is measured by its ejection fraction (EF), the percentage of blood pumped out of the left ventricle with each heartbeat. A normal EF is typically between 50-70%. In heart failure, this percentage is reduced, indicating that the heart is pumping less effectively.
The Two Main Types of Congestive Heart Failure
Congestive heart failure can be classified into two primary types, each reflecting a different aspect of heart function:
1. Systolic Heart Failure (Heart Failure with Reduced Ejection Fraction)
In systolic heart failure, the heart’s pumping ability is impaired. The left ventricle becomes weakened and cannot contract with sufficient force to pump an adequate amount of blood out of the heart. This results in a reduced ejection fraction (EF), often below 40%. Without enough blood flowing through the body, the organs and tissues don’t receive the oxygen and nutrients they need.
Systolic heart failure is often associated with conditions such as coronary artery disease and previous heart attacks, which damage the heart muscle and impair its ability to pump effectively.
2. Diastolic Heart Failure (Heart Failure with Preserved Ejection Fraction)
In diastolic heart failure, the heart’s ability to fill with blood is impaired. The left ventricle becomes stiff or thickened, reducing its capacity to expand and accept blood during the resting phase between heartbeats (diastole). Despite a normal ejection fraction, the heart cannot fill properly, leading to a reduced overall blood flow to the body.
This type of heart failure is more common in older adults, especially those with a history of high blood pressure, diabetes, and obesity.
Mixed Heart Failure
In some cases, individuals may experience a combination of both systolic and diastolic dysfunction, known as mixed heart failure. This type of heart failure can complicate diagnosis and treatment, requiring a more tailored approach to care.
The Causes of Congestive Heart Failure
Congestive heart failure is not a single disease but rather a complex syndrome with many potential causes. Understanding these causes is crucial for both prevention and treatment. The heart’s ability to pump blood can be impaired by factors that directly affect the heart muscle or by those that impact the heart’s ability to relax and fill with blood. Here are some of the most common contributors:
Coronary Artery Disease (CAD)
As mentioned earlier, coronary artery disease is the leading cause of heart failure. CAD occurs when the arteries supplying blood to the heart muscle become narrowed or blocked due to the buildup of plaque. This reduces the oxygen and nutrients available to the heart, weakening the muscle over time.
High Blood Pressure (Hypertension)
When blood pressure is high, the heart must work harder to pump blood through the body. Over time, this increased workload causes the heart muscle to thicken and stiffen, leading to both systolic and diastolic heart failure. Hypertension also accelerates the process of atherosclerosis (plaque buildup), further compromising the heart’s ability to pump efficiently.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle that impair its ability to contract or relax. This condition may be caused by genetic factors, alcohol abuse, infections, or other conditions. It can lead to both systolic and diastolic dysfunction, depending on the type of cardiomyopathy.
Heart Valve Problems
Heart valves ensure that blood flows in one direction through the heart. If these valves are damaged or diseased, they can cause blood to leak back into the heart, or they may become narrowed, obstructing the flow of blood. This can lead to heart failure by placing additional stress on the heart.
Arrhythmias
Arrhythmias, or irregular heartbeats, can interfere with the heart’s ability to pump blood efficiently. Conditions like atrial fibrillation, which is common in people with heart failure, can cause the heart to beat too rapidly or irregularly, further weakening the heart’s function.
Congenital Heart Defects
Some people are born with structural heart defects that affect the way blood flows through the heart. Over time, these defects can lead to heart failure, especially if they cause the heart to work harder than normal.
Other Contributing Factors
Other factors such as obesity, diabetes, excessive alcohol consumption, smoking, and certain medications can also increase the risk of developing heart failure. These conditions can damage the heart in various ways, either by increasing the heart’s workload or by affecting the heart muscle directly.
Symptoms of Congestive Heart Failure
The symptoms of congestive heart failure can vary depending on the severity and stage of the condition. However, some common signs and symptoms include:
- Shortness of Breath: One of the hallmark symptoms of heart failure, shortness of breath occurs because the heart can no longer pump blood effectively, leading to fluid buildup in the lungs (pulmonary congestion).
- Fatigue: When the heart is not pumping blood effectively, less oxygen is delivered to the muscles and tissues, leading to tiredness and weakness.
- Swelling (Edema): Fluid buildup can occur in the legs, ankles, abdomen, and lungs, causing noticeable swelling.
- Rapid or Irregular Heartbeat: The heart may attempt to compensate for its decreased efficiency by beating faster or irregularly.
- Persistent Coughing or Wheezing: This can be a result of fluid buildup in the lungs.
- Decreased Exercise Capacity: Activities that were once easy, such as walking or climbing stairs, may become difficult or impossible due to fatigue and shortness of breath.
Worsening Symptoms
As heart failure progresses, the symptoms can worsen. Shortness of breath may occur even at rest, and swelling can become more pronounced. In severe cases, the heart may struggle to maintain adequate circulation, leading to life-threatening complications like organ failure.
The Diagnosis of Congestive Heart Failure
Diagnosing CHF requires a combination of medical history, physical examination, and diagnostic tests. Healthcare providers will often look for signs of fluid buildup, such as swelling or crackling sounds in the lungs. Common diagnostic tests for heart failure include:
- Electrocardiogram (ECG): To detect arrhythmias or signs of heart damage.
- Echocardiogram: An ultrasound of the heart to assess its structure, function, and ejection fraction.
- Chest X-ray: To look for signs of fluid buildup in the lungs.
- Blood Tests: To check for elevated levels of certain substances, such as brain natriuretic peptide (BNP), which are often elevated in people with heart failure.
Treatment and Management of Congestive Heart Failure
While there is no cure for congestive heart failure, there are many treatments available to manage the condition and improve quality of life. Treatment typically focuses on improving heart function, reducing symptoms, and preventing complications.
Medications
Several classes of medications are used to treat CHF, including:
- ACE Inhibitors and ARBs: These drugs help relax blood vessels, reduce blood pressure, and decrease the heart’s workload.
- Beta-Blockers: These medications slow the heart rate and reduce blood pressure, helping the heart pump more efficiently.
- Diuretics: These are used to reduce fluid buildup in the body by increasing urination.
- Aldosterone Antagonists: These help balance sodium and fluid levels in the body.
Lifestyle Changes
Lifestyle modifications are critical in managing heart failure. A healthy diet, regular physical activity (under a doctor’s supervision), weight management, and avoiding smoking or alcohol can all contribute to better heart health. Managing underlying conditions such as high blood pressure, diabetes, and high cholesterol is also essential.
Surgical Interventions
In some cases, surgical procedures may be necessary, especially if heart failure is caused by structural problems in the heart. These may include:
- Heart Valve Repair or Replacement
- Coronary Artery Bypass Surgery (CABG)
- Implantable Cardioverter-Defibrillators (ICDs) or Cardiac Resynchronization Therapy (CRT) for people with certain types of arrhythmias
Heart Transplantation
In severe cases of heart failure that do not respond to other treatments, a heart transplant may be considered. This is typically a last resort and requires careful evaluation.
Living with Congestive Heart Failure
Although congestive heart failure is a chronic condition, many people live long and fulfilling lives with the right treatment plan. The key to managing CHF is early diagnosis, regular monitoring, and adherence to prescribed treatments. Emotional support, including counseling and support groups, can help individuals cope with the challenges of living with heart failure.