Prostate cancer is one of the most common cancers affecting men worldwide, and yet it often develops silently, without obvious symptoms in its early stages. For many, the very idea of cancer evokes fear, uncertainty, and a sense of helplessness. But knowledge is power. To understand prostate cancer is to reclaim control—over choices, over health, and over hope.
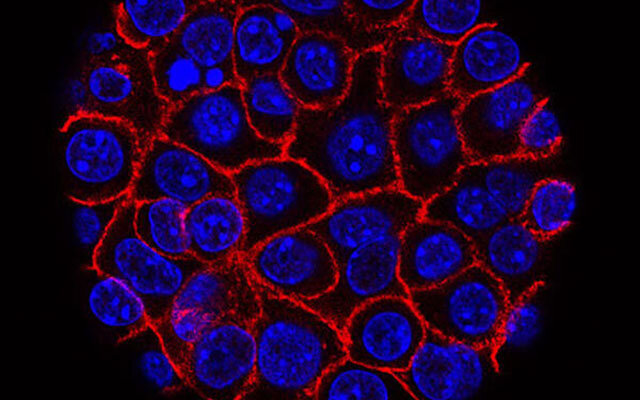
The prostate, a small walnut-shaped gland located just below the bladder, plays an outsized role in men’s health. It produces seminal fluid, which nourishes and transports sperm. Most of the time, the prostate quietly carries out its function, unnoticed. But in some men, cells in the prostate begin to grow uncontrollably. When this happens, prostate cancer is born.
For decades, prostate cancer has challenged scientists and doctors, not only because of its prevalence but also because of its unpredictable nature. Some prostate cancers are aggressive and spread quickly, while others grow so slowly that they may never pose a serious threat. This complexity makes understanding the causes, recognizing the symptoms, diagnosing accurately, and choosing the right treatment both a science and an art.
The Prostate: A Small Gland with a Big Impact
To fully understand prostate cancer, one must first appreciate the prostate itself. This gland, typically about the size of a walnut, sits between the bladder and the penis, encircling the urethra—the tube that carries urine and semen out of the body.
Its main role is to produce seminal fluid, a key component of semen, which supports sperm survival and fertility. Hormones, especially testosterone, regulate the prostate’s growth and function. With age, the prostate naturally enlarges—a condition called benign prostatic hyperplasia (BPH). While BPH is not cancer, its symptoms can sometimes resemble those of prostate cancer, making medical evaluation essential.
The prostate’s location and function explain why cancer in this gland can cause urinary symptoms, sexual difficulties, and, in advanced cases, widespread health problems.
Causes of Prostate Cancer: Why Does It Develop?
The precise causes of prostate cancer remain complex, involving a blend of genetics, environment, lifestyle, and biological aging. Scientists have identified several risk factors that increase a man’s likelihood of developing the disease.
Genetic Factors
Some men inherit a genetic predisposition to prostate cancer. Mutations in genes such as BRCA1, BRCA2, or HOXB13 have been linked to higher risks. Men with a family history of prostate cancer—especially if a father, brother, or multiple relatives were affected—face a significantly elevated likelihood of developing the disease themselves.
Age
Age is one of the strongest risk factors. Prostate cancer is rare in men under 40 but becomes increasingly common after age 50. By the time men reach their seventies, many will have microscopic evidence of prostate cancer, even if it never becomes clinically significant.
Hormonal Influence
Testosterone and its more potent derivative, dihydrotestosterone (DHT), fuel prostate cell growth. Prolonged exposure to high hormone levels can potentially increase the risk of abnormal cell changes leading to cancer.
Lifestyle and Environmental Factors
Diet and lifestyle also play roles. Diets rich in red meat, processed foods, and high-fat dairy products have been associated with increased risks, while diets high in fruits, vegetables, and omega-3 fatty acids may offer protection. Obesity, sedentary behavior, and smoking are additional contributors.
Environmental exposures, such as certain chemicals used in agriculture or industry, may also heighten risk, though research is ongoing.
Race and Ethnicity
African American men are disproportionately affected, both in incidence and mortality rates. They tend to develop prostate cancer at younger ages and with more aggressive forms. The reasons appear to be a combination of genetics, socio-economic factors, and disparities in healthcare access.
Symptoms of Prostate Cancer: Listening to the Body’s Signals
One of the most challenging aspects of prostate cancer is that, in its early stages, it often causes no symptoms. This silent progression is why routine screening can be so important. However, as the disease grows, it may begin to interfere with normal urinary and reproductive functions.
Early Symptoms
- Difficulty starting or maintaining urination
- Weak urine stream
- Increased frequency of urination, especially at night (nocturia)
- Urgency to urinate
- Feeling that the bladder is not fully emptied
These symptoms are not unique to cancer; they can also result from benign prostatic hyperplasia or urinary tract infections.
Advanced Symptoms
If the cancer grows larger or spreads beyond the prostate, additional symptoms may appear:
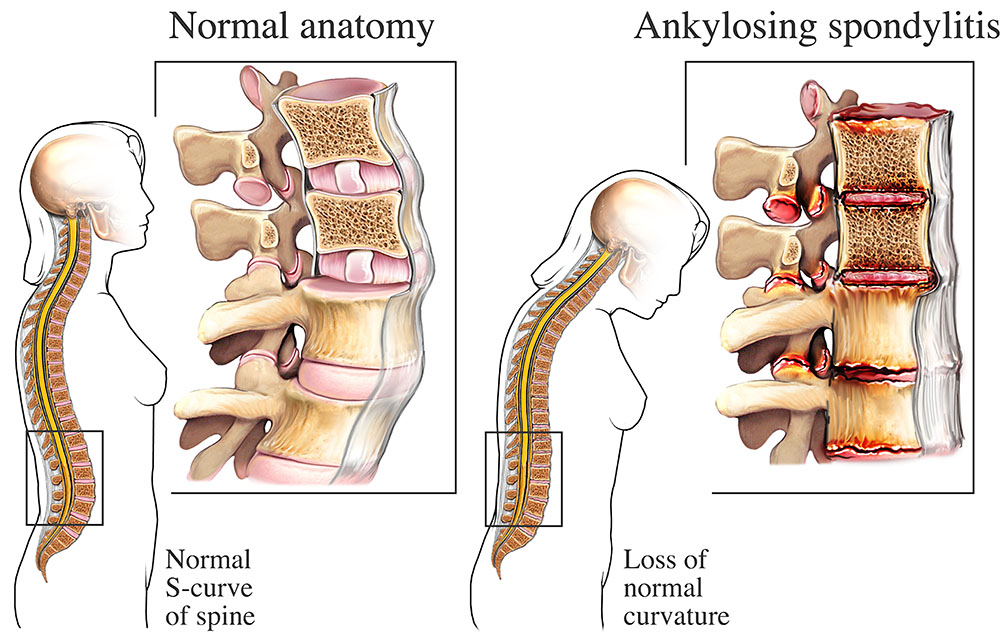
- Blood in urine or semen
- Painful ejaculation
- Erectile dysfunction
- Pain in the hips, spine, or ribs (a sign of bone metastasis)
- Unexplained weight loss and fatigue
Recognizing these symptoms early and seeking medical advice can make the difference between a manageable condition and a life-threatening illness.
Diagnosis: Shedding Light on the Hidden Enemy
Accurate diagnosis is crucial, not only to confirm the presence of prostate cancer but also to determine its aggressiveness and best course of treatment.
Prostate-Specific Antigen (PSA) Test
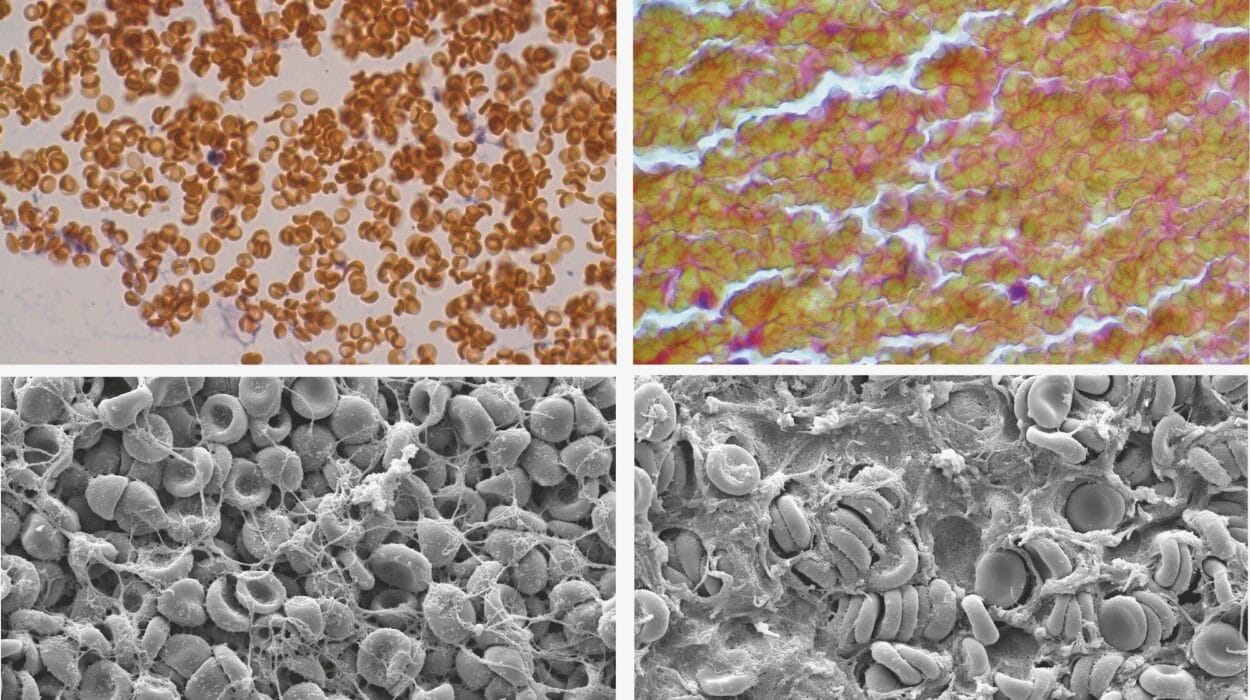
The PSA test measures the level of prostate-specific antigen in the blood. Elevated PSA levels can suggest prostate cancer but may also result from BPH or infection. While controversial due to risks of overdiagnosis, PSA testing remains a valuable screening tool when used judiciously.
Digital Rectal Exam (DRE)
A physician inserts a gloved, lubricated finger into the rectum to feel for irregularities in the prostate. Though uncomfortable, the DRE can detect abnormalities that PSA tests might miss.
Imaging Techniques
MRI and ultrasound provide detailed views of the prostate, helping identify suspicious areas. Advanced imaging can also evaluate whether cancer has spread beyond the gland.
Biopsy
The definitive diagnosis comes from a biopsy—removing small samples of prostate tissue to be examined under a microscope. Pathologists then assign a Gleason score, which grades the aggressiveness of cancer cells.
Staging
Once diagnosed, prostate cancer is staged to determine how far it has progressed:
- Stage I: Small, confined to the prostate, low risk
- Stage II: Still confined but larger or more aggressive
- Stage III: Spread to surrounding tissues
- Stage IV: Spread to lymph nodes, bones, or distant organs
Staging guides treatment choices and prognosis.
Treatment Options: From Watchful Waiting to Advanced Therapies
Treatment for prostate cancer depends on the stage, aggressiveness, age, overall health, and personal preferences of the patient. Unlike many cancers, not all prostate cancers require immediate aggressive treatment. Some grow so slowly that careful monitoring is sufficient.
Active Surveillance and Watchful Waiting
For men with low-risk, slow-growing prostate cancers, doctors may recommend active surveillance—regular PSA tests, biopsies, and imaging to monitor cancer progression. If signs of growth appear, treatment can begin.
Watchful waiting, on the other hand, involves less intensive monitoring, focusing on symptom management rather than cure—often chosen by older men or those with other serious health issues.
Surgery: Radical Prostatectomy
Surgical removal of the prostate, known as radical prostatectomy, is a common treatment for localized prostate cancer. It can be performed through open surgery, laparoscopic techniques, or robotic-assisted methods.
While often effective, surgery carries risks: urinary incontinence, erectile dysfunction, and other complications. Advances in surgical precision have reduced these side effects, but they remain significant considerations.
Radiation Therapy
Radiation therapy uses high-energy beams to destroy cancer cells. It can be delivered externally (external beam radiation therapy) or internally through implanted radioactive seeds (brachytherapy).
Radiation is often as effective as surgery for localized cancers but can also cause urinary, bowel, and sexual side effects.
Hormone Therapy
Because prostate cancer depends on male hormones, hormone therapy—or androgen deprivation therapy (ADT)—aims to lower testosterone levels or block its effects. This can shrink or slow cancer but does not cure it. It is often used for advanced or recurrent cancers.
Chemotherapy
Chemotherapy, which uses drugs to kill rapidly dividing cells, is typically reserved for advanced prostate cancers that no longer respond to hormone therapy. While effective, it can cause fatigue, nausea, hair loss, and other side effects.
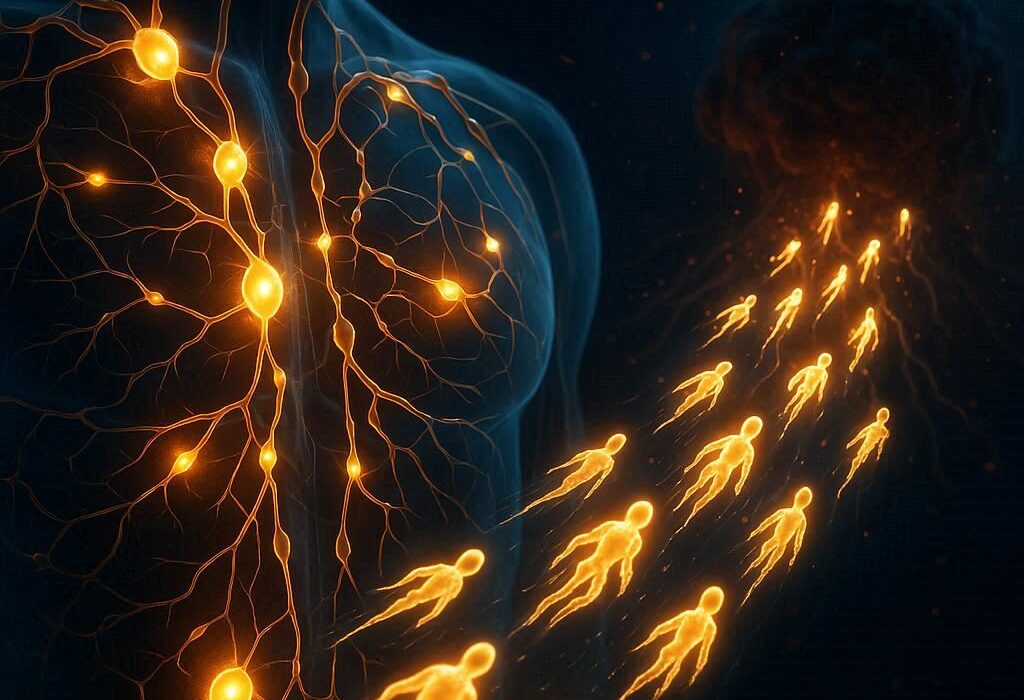
Immunotherapy and Targeted Therapy
Newer treatments harness the immune system or target specific genetic mutations in cancer cells. Immunotherapies, such as checkpoint inhibitors, and drugs that exploit DNA repair defects (like PARP inhibitors), are expanding options for advanced cases.
Bone-Targeted Treatments
Since prostate cancer often spreads to the bones, medications like bisphosphonates or radiopharmaceuticals help reduce bone pain and fractures.
Living with Prostate Cancer: Beyond the Diagnosis
A prostate cancer diagnosis reshapes a man’s life. It brings not only medical challenges but also emotional, psychological, and social ones. Many men struggle with anxiety, fear, and questions about identity, sexuality, and future.
Support from family, friends, and healthcare providers is essential. Counseling, support groups, and open conversations about concerns can reduce the sense of isolation.
Lifestyle changes—such as adopting a healthy diet, exercising regularly, managing stress, and quitting smoking—can improve both quality of life and treatment outcomes. Many men also find strength in mindfulness, spirituality, or advocacy, turning their journey into a source of purpose and resilience.
Prevention: Can Prostate Cancer Be Avoided?
While not all prostate cancers can be prevented, certain strategies may reduce risk:
- Eating a balanced diet rich in vegetables, fruits, and whole grains
- Maintaining a healthy weight
- Exercising regularly
- Avoiding smoking and limiting alcohol
- Having regular check-ups, especially for those with a family history or higher risk
Prevention is not about eliminating all risks but about stacking the odds in one’s favor.
The Future of Prostate Cancer Care
Research is moving rapidly. Precision medicine—tailoring treatment to individual genetics—is already transforming prostate cancer care. Liquid biopsies, which detect cancer DNA in the blood, may soon allow earlier and less invasive diagnosis. Artificial intelligence is helping doctors interpret scans and predict outcomes with greater accuracy.
Scientists are also exploring vaccines that could train the immune system to prevent prostate cancer entirely, a groundbreaking possibility for the future.
Hope and Humanity in the Face of Cancer
Prostate cancer is more than a disease; it is a journey that tests resilience, redefines priorities, and deepens appreciation for life. While statistics highlight its prevalence, they cannot capture the countless stories of men who faced the diagnosis, made difficult choices, endured treatments, and emerged with renewed strength.
To speak of prostate cancer is to speak not only of cells and science but also of courage, family, and the will to live fully. Advances in research continue to bring hope, but perhaps the greatest source of strength lies in the human capacity to face illness with dignity, determination, and love.