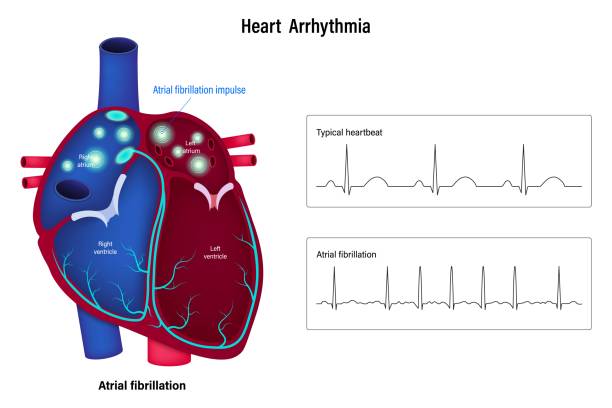
Obesity has become a defining epidemic of the 21st century, with over 650 million adults affected globally, according to the World Health Organization. It’s a condition deeply intertwined with modern lifestyles—overeating, processed food consumption, and sedentary behavior. The consequences are dire: heart disease, type 2 diabetes, fatty liver disease, and certain cancers. But beneath the visible fat and rising statistics lies a subtler story—one written by trillions of invisible microbial partners within us.
In a groundbreaking study published in Cell Metabolism, researchers led by Hiroshi Ohno at the RIKEN Center for Integrative Medical Sciences (IMS) in Japan have discovered a surprisingly elegant solution to the obesity puzzle—one that hinges on a special molecule called acetate, a tailored fiber supplement, and the quiet but powerful action of gut bacteria known as Bacteroides.
This discovery does more than just open the door to potential new obesity treatments—it reshapes how we think about weight, metabolism, and the critical relationship between our bodies and the microbes that live inside us.
Fermentation, Fiber, and Fat: The Hidden Metabolism in Your Gut
To understand this discovery, we need to take a detour through the large intestine, where most dietary fiber ends up after escaping digestion in the stomach and small intestine. Here, trillions of bacteria engage in a metabolic alchemy called fermentation, breaking down indigestible plant matter into short-chain fatty acids (SCFAs), including acetate, butyrate, and propionate. These SCFAs don’t just get absorbed—they act as powerful molecular signals, regulating inflammation, appetite, and even how our bodies store and use energy.
Among SCFAs, acetate is the most abundant, and it’s already known to have several beneficial effects on metabolism, including suppressing appetite and enhancing fat oxidation. But here’s the catch: the amount of acetate produced by fermentation varies wildly between individuals, depending on gut bacteria composition, fiber intake, and even genetics. This makes dietary fiber—a powerful prebiotic—not always reliable as a one-size-fits-all solution to weight management.
Ohno and his team sought to bypass this variability. What if, instead of hoping our gut microbes would produce enough acetate from dietary fiber, we simply delivered acetate directly to where it matters most?
Enter AceCel: The Designer Fiber That Hacks the Gut
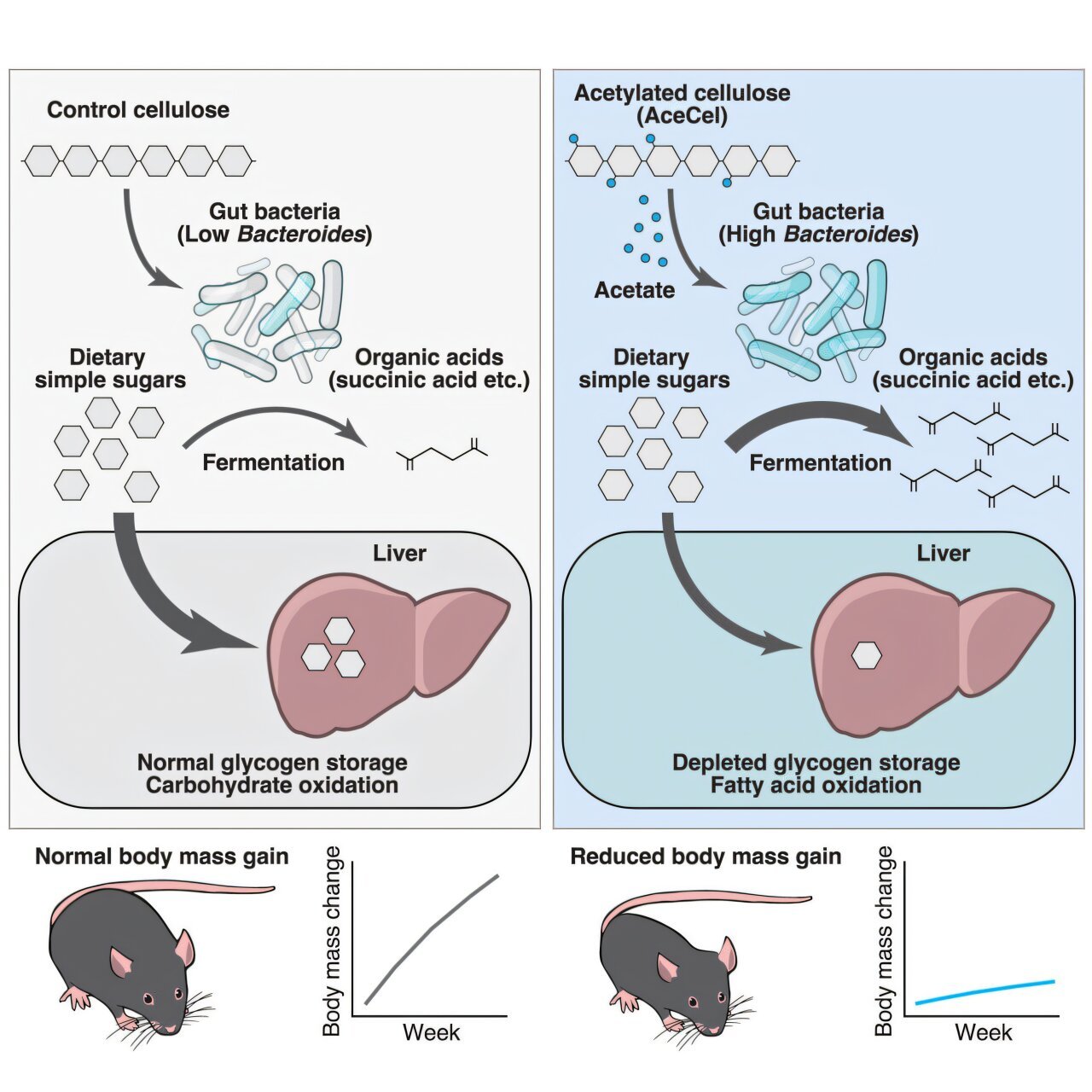
Building on earlier work, the RIKEN team developed AceCel, a novel compound that chemically binds acetate to cellulose, a type of dietary fiber that travels largely undigested to the colon. This design ensures that acetate isn’t digested too early and instead arrives intact in the distal large intestine—the fermentation hub of the gut.
In their new study, researchers administered AceCel to both lean and obese mice. The results were striking. Mice fed AceCel lost weight, reduced their liver fat, and crucially, maintained their muscle mass. This is especially important because many weight-loss interventions also lead to muscle loss, which can weaken metabolism and long-term health.
But what’s truly compelling is what AceCel did not do: similar weight loss effects weren’t observed when other SCFAs, like butyrate or propionate, were tested. This pinpointed acetate as the molecule doing the heavy lifting. The team dug deeper, asking not just what was happening, but how.
Fuel Shift: From Sugar to Fat
When scientists examined how energy was being produced in AceCel-treated mice, they noticed a dramatic shift in metabolic fuel. Instead of drawing energy primarily from carbohydrates, these mice were burning more fat, particularly from their liver—a process similar to what occurs during fasting or low-carbohydrate diets like keto.
In practical terms, this means that AceCel doesn’t just make you eat less—it reprograms your metabolism, encouraging your body to burn stored fat rather than quickly available sugars. The mice, notably, remained more metabolically flexible—a hallmark of good metabolic health.
Even more intriguingly, this metabolic shift didn’t appear to be a simple side-effect of calorie reduction or appetite suppression. There was something deeper at play—something microbial.
The Microbial Middleman: Why Bacteroides Matter
To decode the connection between acetate and metabolism, Ohno’s team performed a series of tests on mice with altered gut microbiomes. Some mice had no gut bacteria at all, while others were selectively colonized with specific species of Bacteroides, a genus of bacteria common in healthy human intestines.
What they found was nothing short of revelatory: AceCel had no beneficial effects in mice without gut bacteria. But when any of three Bacteroides species were present, weight loss and fat reduction returned, confirming that acetate alone isn’t enough—it requires the right microbial partner.
This Bacteroides-acetate partnership appears to remodel the gut ecosystem in ways that enhance carbohydrate fermentation. As more sugars get consumed by bacteria in the gut, less sugar remains for the host body to absorb, reducing the tendency to store that sugar as fat or liver glycogen. In essence, gut bacteria are hijacking and consuming the sugars before your body can.
This microbial sugar theft doesn’t starve the host—it redirects energy toward fat metabolism, giving the body no choice but to start burning its own fat reserves. It’s a profound example of how microbial ecology directly shapes host metabolism.
Implications for Human Health: A New Front in the War on Obesity
The potential of this research is enormous. Unlike pharmaceuticals that alter brain chemistry to suppress appetite or surgeries that restrict stomach size, AceCel represents a microbiome-targeted therapy that works with the gut, rather than against it.
“Developing a treatment or prevention strategy for obesity is an urgent issue that must be solved quickly,” said Ohno in a press release. “We found that acetylated cellulose can prevent obesity by modulating the function of the gut microbiome.”
Of course, this is still early-stage research. The current findings are based on mouse models, and while the gut physiology of mice shares many similarities with humans, there are important differences. The team’s next step is to confirm the safety and efficacy of AceCel in humans. If successful, it could be formulated into functional foods—perhaps a supplement, a powder, or even an ingredient in bread or cereal.
The Broader Picture: Personalizing the Gut-Body Connection
One of the study’s most fascinating takeaways is the demonstration of how dependent human metabolism is on the microbiome. Your ability to lose weight or process sugar may hinge not just on what you eat—but on who’s living in your gut when you eat it.
This aligns with a growing movement in medicine and nutrition to personalize treatments based on microbiome profiling. Imagine a future where a stool sample helps doctors tailor weight-loss strategies based on your microbial fingerprints. If Bacteroides levels are low, you might need a probiotic boost to unlock the full potential of something like AceCel.
It also forces us to reevaluate conventional advice around dietary fiber. It’s not just about how much you consume—but how your body and microbes work together to use it. This insight may finally explain why some people respond better to high-fiber diets than others.
Final Thoughts: Rethinking What It Means to Eat
The study from Hiroshi Ohno’s team is more than a breakthrough in obesity research—it’s a testament to the intricate, invisible ecosystems inside us and how they influence every facet of our physiology.
It suggests that combating obesity might not require starvation, intense workouts, or draconian diets, but smarter interventions that harness the synergy between food and our microbial allies. As science continues to unravel the mysteries of the microbiome, we are beginning to understand that the path to better health may run not just through the mouth, but through the microbiota-filled corridors of the colon.
In the future, “you are what you eat” may need an update: You are what your microbes do with what you eat.
Reference: Tadashi Takeuchi et al, Acetylated cellulose suppresses body mass gain through gut commensals consuming host-accessible carbohydrates, Cell Metabolism (2025). DOI: 10.1016/j.cmet.2025.04.013