Imagine a man in his thirties or forties, once full of energy and vitality, suddenly finding himself constantly fatigued, struggling to focus, feeling less motivated, and noticing changes in his body that he can’t quite explain. His muscles seem harder to maintain, his moods swing unpredictably, and his desire for intimacy has faded. He dismisses it as “just getting older,” but beneath the surface, a silent battle may be unfolding—a battle between chronic stress and testosterone, one of the most important hormones for male health and well-being.
Testosterone has long been associated with masculinity, but its role extends far beyond building muscle or fueling sex drive. It affects energy levels, mood, bone density, and even how the body stores fat. At the same time, stress is an unavoidable part of life, designed to protect us in short bursts but deeply destructive when it becomes chronic. Modern science now reveals a powerful and often underestimated connection between stress and low testosterone—a connection that affects not only men’s physical health but also their emotional lives, relationships, and overall sense of purpose.
To understand this connection, we must dive into the intricate world of hormones, explore how stress rewires the body, and examine how the balance between stress and testosterone can shape the course of a man’s life.
The Vital Role of Testosterone
Testosterone is the primary male sex hormone, produced mainly in the testes, with small amounts also coming from the adrenal glands. While both men and women have testosterone, men produce it at much higher levels, making it central to male physiology.
During puberty, testosterone triggers the development of male characteristics—deepening of the voice, growth of facial and body hair, increased muscle mass, and the maturation of reproductive organs. In adulthood, it continues to influence:
- Physical strength and muscle mass
- Bone density and skeletal health
- Red blood cell production
- Sexual desire and performance
- Energy levels and motivation
- Mood regulation and cognitive sharpness
In essence, testosterone is not merely a “sex hormone.” It is a vital regulator of overall vitality, resilience, and quality of life. When testosterone levels drop below normal, a condition known as hypogonadism or “Low T,” men can experience fatigue, depression, loss of muscle, increased fat accumulation, and reduced libido.
But what many people don’t realize is that chronic stress is one of the most significant contributors to lowering testosterone levels.
Stress: The Body’s Double-Edged Sword
Stress is not inherently bad. In fact, short-term stress—known as acute stress—can save lives. It activates the “fight or flight” response, releasing hormones like cortisol and adrenaline that prepare the body to respond to immediate danger. Heart rate increases, blood pressure rises, and energy floods the muscles.
The problem arises when stress is no longer temporary. In modern society, people often face chronic stress from financial struggles, work pressure, lack of sleep, relationship challenges, or constant exposure to digital overstimulation. Unlike acute stress, which ends once the threat is gone, chronic stress lingers like a shadow, keeping the body in a constant state of alert.
This prolonged stress response disrupts many systems in the body, including the reproductive and endocrine systems. And it is here that cortisol—the primary stress hormone—comes into direct conflict with testosterone.
Cortisol vs. Testosterone: A Hormonal Tug-of-War
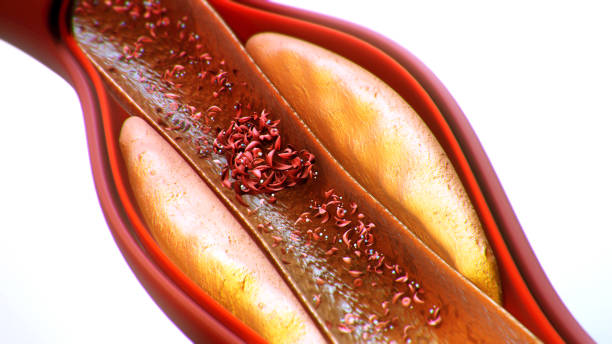
Cortisol and testosterone are both produced from cholesterol, the raw material for many hormones. Under normal conditions, the body maintains a healthy balance between them. But when stress persists, cortisol levels remain elevated, and testosterone production begins to suffer.
This happens through several mechanisms:
- Hormonal Competition
Since cortisol and testosterone share a precursor (cholesterol), chronic stress shifts resources toward cortisol production at the expense of testosterone. - Suppression of the Hypothalamic-Pituitary-Gonadal (HPG) Axis
Stress interferes with the brain’s signaling system that regulates testosterone production. The hypothalamus and pituitary gland, which normally stimulate the testes to produce testosterone, reduce their activity when stress hormones are elevated. - Testicular Effects
Prolonged cortisol exposure directly impairs the Leydig cells in the testes, which are responsible for making testosterone. - Disrupted Sleep Cycles
Stress often leads to poor sleep, and since testosterone production peaks during deep sleep, this further reduces levels. - Increased Inflammation
Chronic stress fuels inflammation, which damages tissues and interferes with hormone regulation, compounding testosterone decline.
In short, the body prioritizes survival over reproduction when it perceives constant stress. From an evolutionary standpoint, this makes sense—facing danger, the body invests energy into immediate survival rather than fertility or long-term vitality. But in today’s world, where stress is chronic and often psychological rather than life-threatening, this survival mechanism becomes a health liability.
The Symptoms of Stress-Induced Low Testosterone
When stress lowers testosterone, men may begin to notice changes that touch nearly every part of life. The symptoms are often subtle at first, but over time they can become debilitating.
- Physical Symptoms: Fatigue, loss of muscle mass, increased body fat (especially around the abdomen), reduced strength, weaker bones, and slower recovery after exercise.
- Sexual Symptoms: Decreased libido, erectile difficulties, reduced semen volume, and infertility.
- Cognitive Symptoms: Brain fog, difficulty concentrating, and reduced memory retention.
- Emotional Symptoms: Irritability, low mood, anxiety, depression, and loss of motivation.
Many men ignore these symptoms, attributing them to aging or stress alone, without realizing that stress and low testosterone are often two sides of the same coin, each amplifying the other.
The Vicious Cycle: Stress Feeds Low Testosterone, and Low Testosterone Feeds Stress
The relationship between stress and testosterone is not one-directional—it is a vicious cycle.
Chronic stress lowers testosterone, which then reduces resilience to stress. Low testosterone increases fatigue, depression, and irritability, making everyday stressors feel heavier and harder to handle. This creates a downward spiral: more stress leads to lower testosterone, which leads to greater stress sensitivity.
This cycle explains why some men find themselves trapped in a state of burnout, unable to regain energy or motivation despite rest. It also highlights the importance of breaking the cycle—not only by reducing stress but also by restoring hormonal balance.
The Role of Lifestyle in Breaking the Cycle
Fortunately, lifestyle choices have a powerful impact on both stress management and testosterone levels. Science shows that certain habits can reverse the damage caused by chronic stress and support healthy testosterone production.
Nutrition
A nutrient-rich diet provides the building blocks for hormones and reduces inflammation. Diets high in processed foods, sugar, and unhealthy fats promote stress and hormonal imbalance, while diets rich in whole foods, lean proteins, healthy fats, fruits, and vegetables support balance. Zinc, vitamin D, magnesium, and omega-3 fatty acids are especially important for testosterone production.
Physical Activity
Exercise reduces stress, lowers cortisol, and stimulates testosterone production—especially resistance training and high-intensity interval training (HIIT). However, excessive exercise without proper recovery can have the opposite effect, raising cortisol and lowering testosterone. Balance is key.
Sleep
Deep, restorative sleep is essential for testosterone production. Poor sleep increases cortisol, lowers testosterone, and amplifies stress. Prioritizing sleep hygiene—consistent schedules, dark rooms, and limited screen exposure before bed—can make a profound difference.
Stress Management Techniques
Practices like meditation, mindfulness, deep breathing, and yoga lower cortisol and promote hormonal balance. Even small, daily rituals of relaxation can reset the stress response and support testosterone production.
Healthy Relationships and Social Support
Positive social connections buffer stress and raise well-being, while loneliness and conflict worsen stress and hormonal imbalance. Maintaining strong relationships and seeking emotional support is as important for testosterone as diet or exercise.
Medical Interventions: When Lifestyle Isn’t Enough
For some men, lifestyle changes may not fully restore testosterone levels, especially if chronic stress has been ongoing for years or if age-related decline is significant. In such cases, medical evaluation is essential.
Doctors may measure testosterone levels through blood tests and, if appropriate, recommend treatments such as testosterone replacement therapy (TRT). However, TRT is not a simple solution—it must be carefully monitored to avoid side effects and should ideally be combined with lifestyle strategies that address the root causes of stress and imbalance.
Other medical approaches may involve treating underlying conditions (such as sleep apnea, obesity, or depression) that contribute to both stress and low testosterone.
The Broader Impact: Stress, Testosterone, and Society
The connection between stress and low testosterone is not just a personal health issue—it is a societal one. Modern lifestyles, filled with constant pressure, overwork, and poor sleep, create environments where men are more vulnerable to hormonal decline than ever before.
Low testosterone not only affects individuals but also relationships, families, and workplaces. Men struggling with fatigue, low mood, and reduced motivation may find it harder to perform at work, maintain intimacy at home, or engage fully with life.
By understanding the stress-testosterone connection, society can begin to address these challenges—not by blaming men for weakness, but by recognizing the biological toll of chronic stress and creating environments that support resilience, balance, and health.
Hope and Renewal: Restoring Balance
The connection between stress and low testosterone may seem discouraging, but it also carries a message of hope. Because just as stress can suppress testosterone, reducing stress and supporting the body can restore it.
Men who reclaim balance in their lives—through better sleep, nourishing food, exercise, stress management, and meaningful relationships—often see profound changes in their energy, vitality, and sense of purpose. Their testosterone levels rise, their moods stabilize, and the downward spiral transforms into an upward cycle of health.
Science confirms that the human body is remarkably adaptable. Even after years of stress, the endocrine system can recover, and testosterone production can improve. Health is not about perfection but about resilience—the ability to heal, rebuild, and thrive.
Conclusion: The Hidden Dialogue Between Hormones and Life
At its heart, the connection between stress and low testosterone is a story about balance. It is a dialogue between the body’s survival mechanisms and its drive for vitality, between the pressures of modern life and the timeless rhythms of biology.
Testosterone is not merely a hormone of masculinity—it is a hormone of energy, motivation, and life itself. Stress, while useful in moments of danger, becomes destructive when it lingers. Together, they shape the trajectory of men’s health, influencing how they feel, think, and live.
To care for testosterone is to care for life. It means acknowledging the weight of stress, respecting the body’s needs, and cultivating habits that restore balance. It means recognizing that health is not just about surviving but about thriving, not just about fighting disease but about living fully.
The battle between stress and testosterone may be hidden, but it is not unwinnable. With awareness, science, and conscious choices, men can break the cycle, reclaim their vitality, and rediscover what it means to live with strength, clarity, and resilience.