The human skin, our body’s largest organ, is much more than a protective covering. It is a living, breathing barrier that regulates temperature, shields internal organs, synthesizes vitamin D, and communicates our health to the outside world through its tone, texture, and resilience. But in the case of psoriasis, this remarkable organ becomes the battleground for a perplexing and persistent disorder. Skin cells begin to behave erratically, proliferating far faster than they should, piling up on the surface in thick, scaly plaques that crack, itch, and bleed. These visual signs are just the tip of a much deeper and more complex iceberg—one that connects the skin to the intricate workings of the immune system.
Psoriasis is not just a skin condition. For decades, it was misunderstood as nothing more than a cosmetic nuisance or a stubborn rash. But as research has advanced, the veil has been lifted on its true nature. Psoriasis is now recognized as a chronic, immune-mediated disorder—a condition in which the body’s immune system misfires and turns its sophisticated weapons against its own tissues. In psoriasis, that target happens to be the skin, but the mechanisms driving this attack originate deep within the immune system. This autoimmune connection is at the heart of the disease, and understanding it is essential to unraveling the mystery of what truly causes psoriasis.
Skin in Overdrive: The Cellular Chaos
To understand what goes wrong in psoriasis, one must first grasp how skin normally functions. Skin cells are created in the basal layer, deep within the epidermis, and then rise to the surface in a tightly regulated cycle that takes about four weeks. Once at the surface, these cells slough off, making way for newer ones from beneath. This process is orderly, unnoticeable, and beautifully efficient.
In psoriasis, however, the tempo of this process accelerates dramatically. Instead of taking weeks, skin cells race to the surface in mere days. But the exit ramp is blocked—the skin can’t shed these excess cells fast enough. The result is a buildup of thickened, inflamed patches known as plaques. These are often covered in silvery-white scales and can appear anywhere, though they favor the elbows, knees, scalp, and lower back.
This overproduction of skin cells is not a standalone phenomenon. It is the visible consequence of an immune system in overdrive. What sparks this internal alarm? That question leads us into the labyrinth of immune function, genetic predisposition, environmental influence, and molecular confusion that defines psoriasis.
The Immune System’s Role: Friend Turned Foe
The immune system’s primary job is to protect the body from foreign invaders—viruses, bacteria, and harmful organisms that could cause illness. In autoimmune diseases like psoriasis, the immune system mistakes parts of the body itself as dangerous and launches an attack. In psoriasis, it appears that the immune system erroneously identifies normal skin cells as threats and begins to mount a response.
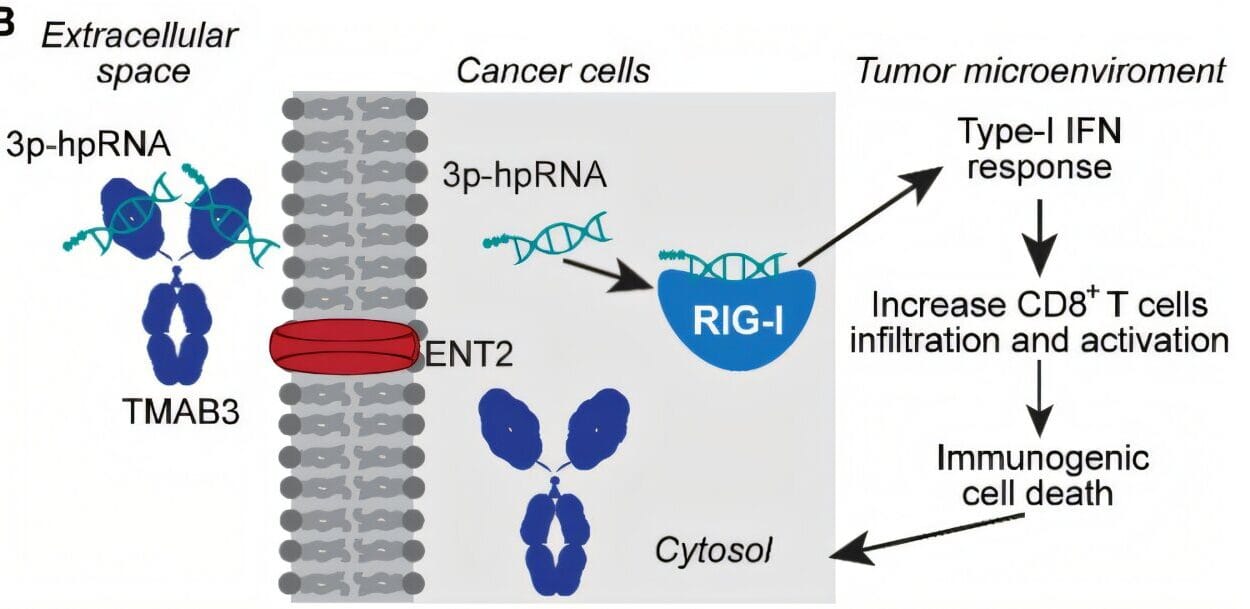
At the center of this miscommunication are T cells, a type of white blood cell that typically identifies and eliminates infected or abnormal cells. In people with psoriasis, these T cells become activated without a clear threat and begin releasing inflammatory signals—cytokines—that tell the skin to make new cells faster. It’s as if the immune system is shouting “Emergency!” in a room where nothing is wrong, setting off a chaotic cascade of reactions.
One of the key cytokines involved in this process is called tumor necrosis factor-alpha (TNF-α), along with others like interleukin-17 (IL-17) and interleukin-23 (IL-23). These messengers fuel inflammation and prompt skin cells to divide and rise to the surface rapidly. The result is a relentless loop: immune cells call for reinforcements, skin cells respond by multiplying, and inflammation intensifies. It is this cellular feedback loop that sustains the chronic nature of psoriasis.
The Genetic Blueprint of Psoriasis
While psoriasis can strike anyone, not everyone is equally vulnerable. Genetics plays a powerful role in determining who develops the disease. Family history is a significant risk factor, with studies showing that if one parent has psoriasis, the child has about a 10 to 20 percent chance of developing it. If both parents are affected, the risk increases dramatically.
Researchers have identified dozens of genes linked to psoriasis, many of which influence immune function and skin barrier integrity. One of the most well-known genes is HLA-Cw6, a variant within the human leukocyte antigen (HLA) complex that is strongly associated with early-onset psoriasis. Other genetic players include those that regulate T-cell activation and cytokine signaling pathways.
However, having the genetic susceptibility does not guarantee that someone will develop psoriasis. This suggests that while the genetic blueprint lays the foundation, other factors must trigger the disease—factors that may include environmental exposures, infections, injuries, or even psychological stress.
Triggering the Flame: Environmental and Lifestyle Factors
The immune system doesn’t turn against the skin in a vacuum. Even in genetically predisposed individuals, psoriasis often needs a push—an environmental or internal trigger—to flare up. One of the most well-documented triggers is streptococcal infection, particularly in the case of guttate psoriasis, a form that often begins in childhood or adolescence with a sudden outbreak of small, teardrop-shaped lesions following a sore throat.
Other infections can also act as catalysts, as can skin injuries, a phenomenon known as the Koebner response, where psoriasis develops at the site of trauma. This can include cuts, burns, insect bites, tattoos, or surgical wounds. For reasons still being studied, the immune system seems particularly reactive to such disruptions in the skin barrier.
Stress, both emotional and physical, is another potent trigger. The mind-body connection in psoriasis is well established. Stress can not only provoke flares but also make existing symptoms worse. This creates a vicious cycle where the visible nature of the disease leads to emotional distress, which in turn exacerbates the physical symptoms.
Certain medications are known to precipitate or worsen psoriasis. These include beta-blockers, lithium, and some antimalarial drugs. Smoking and alcohol use are also associated with increased severity of the disease. Meanwhile, dietary factors, though not direct causes, are thought to influence inflammation and may affect symptom intensity.
The Psoriasis Spectrum: More Than Skin Deep
Though psoriasis most visibly affects the skin, it is increasingly recognized as a systemic condition with implications that extend far beyond the surface. Many people with psoriasis develop psoriatic arthritis, a related autoimmune condition that causes joint pain, stiffness, and swelling. In fact, up to 30 percent of psoriasis patients eventually experience this form of inflammatory arthritis.
Moreover, the chronic inflammation that defines psoriasis may contribute to a range of comorbid conditions, including cardiovascular disease, metabolic syndrome, type 2 diabetes, and inflammatory bowel disease. The connection lies in the shared inflammatory pathways, particularly those involving cytokines like TNF-α and IL-17.
This broader view of psoriasis—as not merely a skin disease but a systemic inflammatory disorder—has revolutionized both its understanding and its treatment. It also reinforces the need for comprehensive care that addresses not only the skin but the whole person.
Diagnosis: The Art of Clinical Recognition
Psoriasis is usually diagnosed through clinical examination. Dermatologists can often identify it based on the appearance and location of the plaques, which have a distinctive thick, red, and scaly quality. Sometimes, a skin biopsy is performed to rule out other conditions or confirm the diagnosis, especially in atypical cases.
There is no single laboratory test to definitively diagnose psoriasis, nor is there a universally accepted way to measure its severity. Doctors often assess the extent of body surface area affected, the impact on quality of life, and the presence of associated conditions like joint pain.
Because psoriasis can resemble other skin disorders—eczema, fungal infections, or seborrheic dermatitis—experience and clinical intuition play an important role in accurate diagnosis. Early diagnosis is particularly important in detecting psoriatic arthritis, which can cause irreversible joint damage if left untreated.
Managing the Immune Storm
Treating psoriasis involves calming the overactive immune response and slowing the rapid production of skin cells. The choice of treatment depends on the severity of the disease, its impact on daily life, and the patient’s overall health.
For mild to moderate cases, topical treatments such as corticosteroids, vitamin D analogs, and coal tar preparations can reduce inflammation and scaling. These are often the first line of defense and can be very effective for localized plaques.
More severe or widespread psoriasis often requires systemic treatments. Traditional options include methotrexate, cyclosporine, and acitretin, which suppress immune function broadly. However, these drugs can have significant side effects and require careful monitoring.
The most transformative advance in recent years has been the development of biologic therapies—medications derived from living organisms that target specific parts of the immune system. Biologics like adalimumab, ustekinumab, secukinumab, and ixekizumab have dramatically improved the lives of many patients with moderate to severe psoriasis, offering high rates of skin clearance and improved quality of life.
In addition to medications, lifestyle factors are increasingly recognized as important in managing psoriasis. Weight loss, smoking cessation, alcohol moderation, stress reduction, and anti-inflammatory diets may help reduce flare-ups and improve treatment outcomes.
Hope on the Horizon: The Future of Psoriasis Research
The story of psoriasis is still being written. With every year, new discoveries shed light on its mechanisms and open doors to more targeted and effective treatments. Scientists are exploring the role of the gut-skin axis, the microbiome, and the genetic underpinnings that predispose individuals to this immune malfunction.
Advances in personalized medicine may eventually allow doctors to tailor treatments to the unique genetic and immunological profile of each patient. New biologics continue to emerge, some with even greater precision and fewer side effects. Researchers are also examining the possibility of reprogramming the immune system to restore tolerance and end the autoimmune attack on the skin.
Importantly, patient advocacy and public awareness have grown significantly. Psoriasis is no longer seen as a mere cosmetic issue but as a legitimate and life-altering disease that warrants serious attention and comprehensive care.
A Journey of Resilience
Living with psoriasis is not easy. It is a condition that affects not just the skin but the soul. The visible nature of the disease can lead to stigma, embarrassment, and emotional pain. But those who live with it—millions worldwide—demonstrate a remarkable resilience. They navigate flares, treatments, and uncertainties with courage, often becoming experts in their own care and powerful advocates for others.
Psoriasis may be rooted in a biological misfire, but it touches every facet of human life. Understanding its causes, especially the autoimmune origins that drive its relentless progression, is not just a scientific endeavor—it’s a step toward empathy, empowerment, and healing.