Eczema is one of the most common chronic skin conditions in the world, yet it remains deeply misunderstood. For many, eczema is not just a patch of dry or irritated skin—it is a daily struggle that affects physical comfort, self-confidence, and even emotional well-being. The condition, also known medically as atopic dermatitis, is often seen in childhood but can persist into adulthood or even begin later in life.
Imagine the constant urge to scratch, the red inflamed patches that refuse to heal, the frustration of trying every cream and still waking up in the middle of the night because the itch is unbearable. This is the reality for millions of people living with eczema. It is a condition that not only affects the skin but ripples into sleep, relationships, work, and overall quality of life.
But what exactly is eczema? Why does it happen? And most importantly, how can it be managed? To answer these questions, we need to dive deep into the science of the skin, the immune system, and the intricate dance between genetics, environment, and lifestyle.
What is Eczema?
The term “eczema” comes from the Greek word ekzein, meaning “to boil over,” a fitting description of the red, inflamed, and irritated patches it causes. Eczema is not a single disease but rather an umbrella term used to describe several conditions that cause inflammation of the skin. The most common form is atopic dermatitis, which is chronic, relapsing, and often linked to allergic tendencies.
Other forms include contact dermatitis (triggered by irritants or allergens), dyshidrotic eczema (characterized by small blisters on the hands and feet), and seborrheic dermatitis (associated with oily, flaky skin). Despite their differences, all types of eczema share one hallmark feature: a disrupted skin barrier that makes the skin more vulnerable to irritants, allergens, and infection.
The Skin Barrier: The Body’s First Line of Defense
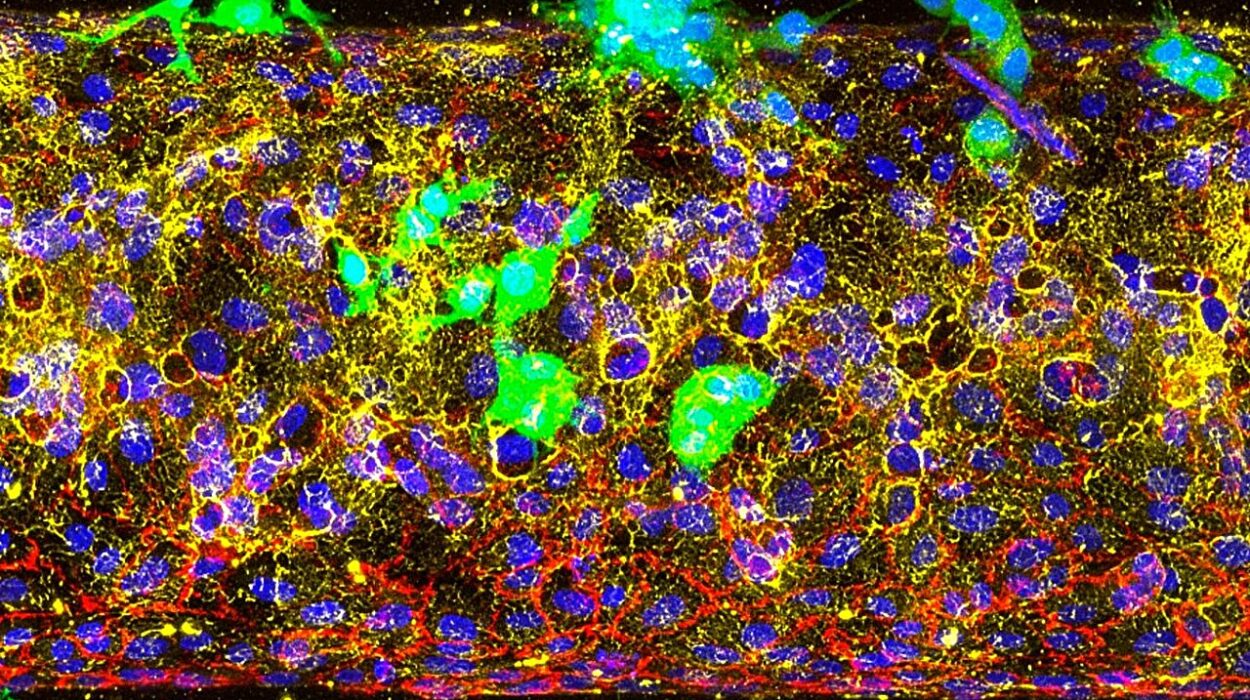
To understand eczema, it’s crucial to understand the skin barrier. The skin is not just a covering for our bodies—it is a living, breathing shield that protects us from the outside world. The outermost layer, the stratum corneum, acts like a brick wall: skin cells are the “bricks,” and lipids (fats) are the “mortar.”
In healthy skin, this barrier keeps moisture in and harmful substances out. But in eczema, this wall is weakened. Cracks appear in the mortar, water escapes, and irritants and microbes sneak in. This not only leads to dry, itchy skin but also triggers an immune response that fuels further inflammation.
For many people with eczema, the barrier dysfunction is linked to a genetic mutation in a protein called filaggrin, which plays a key role in maintaining skin hydration and structure. Without enough filaggrin, the skin struggles to hold moisture and defend against external irritants.
Causes of Eczema: Why Does It Happen?
Eczema does not have a single cause. Instead, it arises from a complex interplay of genetics, immune system dysfunction, environmental triggers, and lifestyle factors.
Genetic Factors
Eczema often runs in families. Children with parents who have eczema, asthma, or hay fever are more likely to develop it themselves. This familial link points to a genetic predisposition, particularly involving genes that regulate skin barrier proteins and immune responses.
The filaggrin mutation mentioned earlier is one example. People with this mutation often have drier, more permeable skin, which sets the stage for eczema flare-ups.
Immune System Imbalance
Eczema is fundamentally an inflammatory condition. In people with eczema, the immune system is hyperactive and reacts too strongly to otherwise harmless substances. Specialized immune cells release inflammatory molecules, such as cytokines, that cause redness, swelling, and itching.
This immune overreaction explains why eczema is often associated with other allergic conditions, including asthma and allergic rhinitis—a combination known as the “atopic triad.”
Environmental Triggers
The modern environment is full of substances that can irritate sensitive skin. Common triggers include:
- Harsh soaps, detergents, or fragrances
- Pollutants and chemicals
- Rough fabrics like wool
- Cold, dry air in winter or excessive heat and sweat in summer
Even emotional stress can provoke flare-ups, as stress hormones disrupt immune balance and weaken the skin barrier.
Allergens
Certain allergens—like pollen, pet dander, mold, and dust mites—can spark eczema flares in sensitive individuals. Food allergies may also play a role, particularly in children, though the relationship between food and eczema is complex and not the same for everyone.
Symptoms of Eczema: Recognizing the Signs
Eczema looks and feels different depending on the person’s age, skin tone, and the type of eczema they have. Yet, there are common threads:
- Itching: Often intense, sometimes unbearable, and usually worse at night.
- Redness and inflammation: On lighter skin, eczema often appears red or pink; on darker skin, it may look purple, gray, or dark brown.
- Dryness and scaling: The skin becomes rough, flaky, and prone to cracking.
- Thickened skin: Chronic scratching can lead to lichenification—areas where the skin becomes thick, leathery, and darker.
- Blisters or oozing: In some cases, small fluid-filled bumps appear, which may ooze and crust over if scratched.
In infants, eczema often begins on the cheeks and scalp, while in older children and adults it tends to appear on the insides of elbows, backs of knees, neck, and hands.
The Burden of Eczema: Beyond the Skin
Eczema is not just a surface problem. The relentless itching can rob people of sleep, leading to fatigue and reduced concentration. Children with eczema may struggle in school due to discomfort or bullying. Adults may feel embarrassed about visible lesions, affecting relationships and self-esteem.
The psychological impact is significant: people with eczema are more likely to experience anxiety and depression. This emotional toll, in turn, can worsen flare-ups, creating a vicious cycle.
Diagnosis: How Eczema is Identified
There is no single test for eczema. Diagnosis is primarily clinical, based on a careful history and physical examination by a dermatologist or healthcare provider.
Key factors doctors consider include:
- Age of onset: Eczema often begins in early childhood.
- Family history: Presence of eczema, asthma, or allergies in relatives.
- Symptoms: Itching, redness, recurrent flare-ups, and chronic dryness.
- Appearance and distribution of lesions: Typical locations such as elbows, knees, and neck.
Sometimes, additional tests may be used to rule out other conditions or identify triggers:
- Patch testing for allergic contact dermatitis
- Blood tests for elevated IgE (an antibody linked to allergies)
- Skin biopsy in atypical cases
Treatment: Managing Eczema, Not Just Suppressing It
Eczema currently has no cure, but it can be managed effectively. Treatment focuses on controlling symptoms, repairing the skin barrier, and reducing inflammation. The approach often involves a combination of lifestyle changes, topical therapies, and sometimes systemic medications.
Moisturizing the Skin
Moisturizers are the cornerstone of eczema care. Regular use of emollients restores the skin barrier, locks in hydration, and reduces flare frequency. Thick creams or ointments are generally more effective than lotions. Applying them right after bathing helps trap moisture.
Topical Medications
When flare-ups occur, medicated creams may be necessary. These include:
- Topical corticosteroids: Reduce inflammation quickly but should be used carefully to avoid thinning of the skin with long-term use.
- Topical calcineurin inhibitors (like tacrolimus and pimecrolimus): Non-steroid alternatives that calm the immune response, particularly useful for delicate areas such as the face.
- Topical phosphodiesterase-4 inhibitors (such as crisaborole): Newer options that target inflammation pathways.
Antihistamines and Itch Relief
While antihistamines may not always stop eczema itch, they can help some individuals, especially at night when itching disrupts sleep. Cool compresses and oatmeal baths also provide relief.
Systemic Treatments
For moderate to severe cases that don’t respond to topical therapy, systemic medications may be prescribed:
- Oral corticosteroids (short-term use only)
- Immunosuppressants such as cyclosporine or methotrexate
- Biologic therapies like dupilumab, a groundbreaking drug that targets specific immune pathways involved in eczema.
Phototherapy
Controlled exposure to ultraviolet (UV) light can reduce inflammation and itching for some patients. This treatment is usually done under medical supervision in dermatology clinics.
Lifestyle Management: Living with Eczema
Daily habits play a huge role in managing eczema. Some practical strategies include:
- Bathing in lukewarm water with gentle cleansers, followed by immediate moisturizing.
- Wearing soft, breathable fabrics like cotton and avoiding rough or synthetic materials.
- Managing stress with techniques like yoga, meditation, or journaling.
- Keeping nails short to minimize skin damage from scratching.
- Identifying and avoiding personal triggers, whether they are certain foods, pets, or seasonal allergens.
Emerging Research and the Future of Eczema Treatment
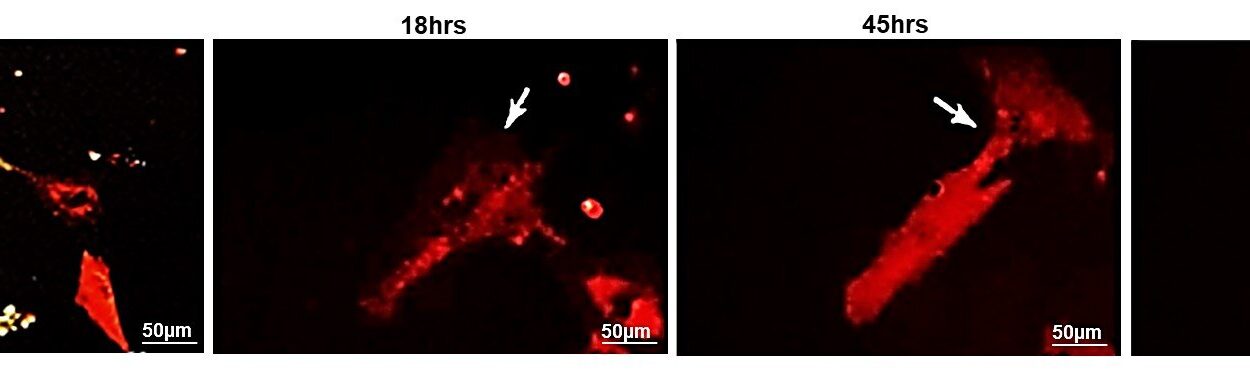
The landscape of eczema research is rapidly evolving. Scientists are uncovering more about the role of the microbiome—the community of bacteria and other microorganisms living on the skin. People with eczema often have an overgrowth of Staphylococcus aureus, which worsens inflammation. Future treatments may involve probiotics, prebiotics, or microbiome-based therapies to restore healthy skin flora.
Biologics and targeted therapies are also expanding. Drugs that block specific immune signals are offering new hope for patients with severe, treatment-resistant eczema. Personalized medicine, based on genetic and molecular profiling, could one day allow doctors to tailor therapies to each patient’s unique biology.
Eczema in Perspective: More Than a Condition
Eczema is a reminder of how interconnected the body truly is. It shows us that the skin is not just a barrier but a messenger—reflecting the state of our immune system, our genetics, our environment, and even our emotions.
Living with eczema is not easy. It requires patience, resilience, and often a lifelong commitment to care. But with modern science, supportive care, and growing awareness, people with eczema can lead fulfilling, vibrant lives.
Ultimately, eczema teaches us empathy—for those whose battles are visible on their skin, and for those whose struggles go deeper, hidden beneath the surface.