In a world increasingly shaped by science and policy, health remains one of the greatest mirrors of our societal values—and its inequalities. A new landmark study, led by Angela Chang of the University of Southern Denmark and published in PLOS Medicine, lifts the veil on a stubborn, underrecognized reality: across much of the globe, men are more likely than women to fall sick and die from major health conditions like hypertension, diabetes, and HIV/AIDS, and yet, paradoxically, less likely to seek or receive medical care. This discovery has sparked fresh conversations about the critical role of sex and gender in shaping health outcomes—and why our one-size-fits-all approach to health policy may be failing half the population.
A Hidden Disparity in Plain Sight
At first glance, this may seem counterintuitive. Much of the public health discourse over the past decades has rightly focused on addressing the unique health needs of women—especially around maternal health, reproductive rights, and access to care. But the new findings reveal a contrasting and equally urgent truth: men’s health is slipping through the cracks, not only because of biological vulnerability but because of ingrained gender norms, risky behaviors, and systemic neglect.
The researchers dove into a treasure trove of global health data spanning numerous age groups and over 200 countries. They focused on three widespread, high-burden diseases: hypertension (high blood pressure), diabetes, and HIV/AIDS. These are not exotic or rare illnesses—they are everyday killers that collectively claim millions of lives each year. Yet, how they affect men and women can differ strikingly, as can the responses from health systems.
What they found was both sobering and enlightening.
Tracing the Health Pathway: Where Men and Women Diverge
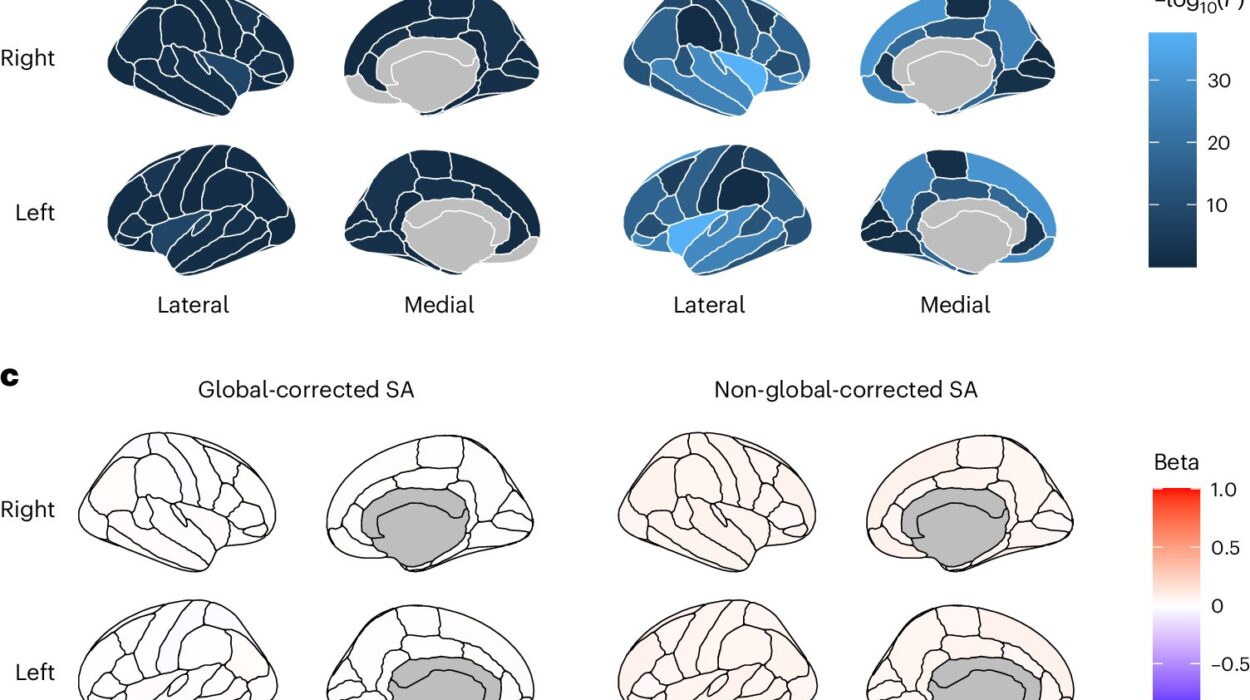
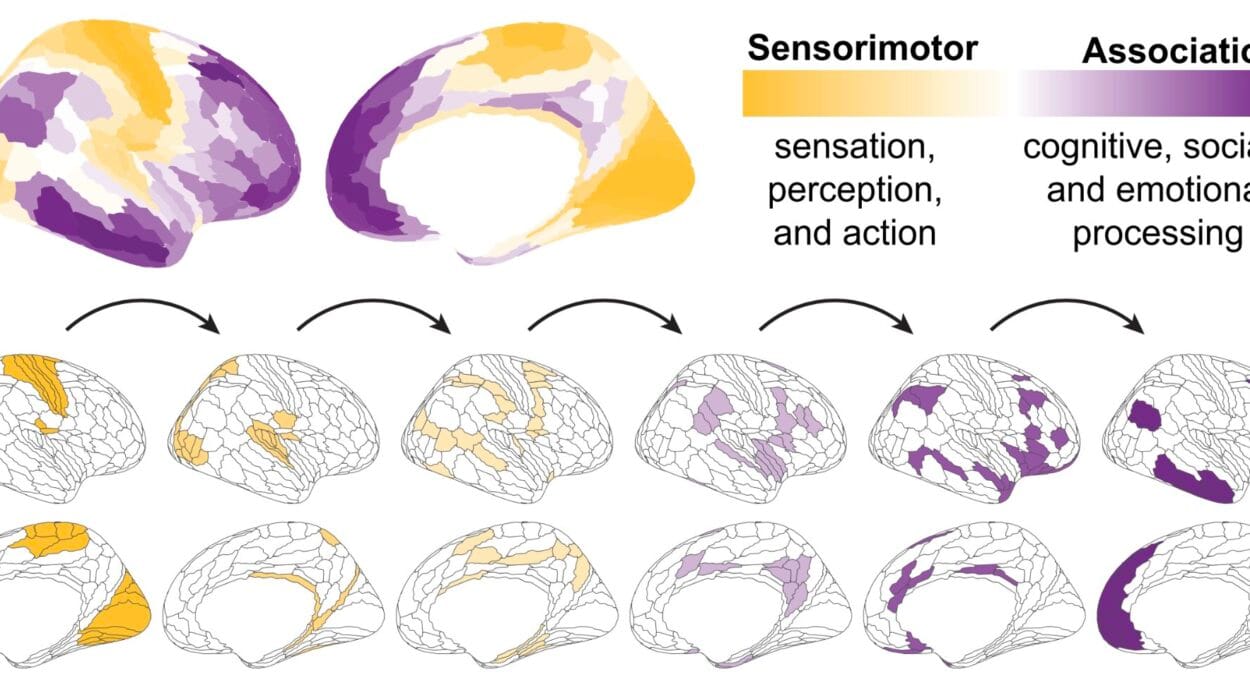
One of the most illuminating aspects of the study is its focus on the “health pathway”—a sequence of stages that everyone theoretically moves through in the course of dealing with illness. This pathway includes exposure to risk, development of disease, diagnosis, treatment, and ultimately, recovery or death.
Across nearly every stage of this journey, men fared worse than women. They had higher rates of disease, were more likely to die from those conditions, and in many countries, were less likely to be diagnosed or treated in the first place.
For hypertension, differences in care between males and females were observed in 200 countries. For diabetes, disparities were found in 39 countries, and for HIV/AIDS, 76 countries showed unequal treatment patterns. The reasons are not always biological. In fact, many are deeply rooted in the social expectations and pressures placed upon men.
The Behavioral Trap: Risk, Masculinity, and Avoidance
The study found that men were more likely to engage in behaviors that increase health risks, such as smoking—a habit that remains far more common among males in many regions. Smoking rates are a leading driver of hypertension and cardiovascular disease, and yet tobacco control programs often fail to specifically address the unique cultural and psychological drivers of male smoking.
At the same time, women were more likely to be obese and engage in unsafe sex, another major risk factor—especially for HIV. These patterns reflect gendered differences in social behavior, access to education, economic autonomy, and exposure to violence, rather than innate differences in biology.
But even more alarming is the tendency among many men to delay or avoid seeking medical care, sometimes until it’s too late. In cultures that prize stoicism, toughness, and self-reliance in men, going to a clinic may be perceived as a sign of weakness. This reluctance can lead to late diagnoses, missed treatments, and preventable deaths. In the realm of public health, silence can be fatal.
Medical Blind Spots: A System Built for Everyone, But Designed for No One
Despite these gendered patterns in disease and behavior, many health policies remain frustratingly neutral—designed without consideration for sex or gender. This is not equality; it is negligence. When we ignore the differences, we fail to provide equity.
Angela Chang and her team emphasize the dangers of this “gender blindness.” Interventions that do not account for who is at risk and why will inevitably miss their targets. As Chang explains, “Without sex-disaggregated cascade data, we’re flying blind—unable to detect who is falling through the cracks in prevention, diagnosis, and care.”
Indeed, when health data is not broken down by sex, we lose the ability to design targeted, effective solutions. A blood pressure screening campaign might reach fewer men if it takes place only at antenatal clinics. HIV education might be less effective if it ignores the different social pressures faced by men and women in their relationships. Treatment adherence programs may fall short if they don’t understand how gender roles influence who can attend follow-ups or access medication.
Global Gaps, Local Consequences
The disparities are not evenly distributed across the world. In some countries, men die from non-communicable diseases like hypertension and diabetes at twice the rate of women, while in others, the differences are more subtle but still significant. In Sub-Saharan Africa, for example, men living with HIV are more likely to die than women, largely because they are diagnosed later and enter care later, if at all.
In high-income countries, the gaps may stem more from behavioral and social factors. In the United States and many European nations, for example, male reluctance to visit doctors is a persistent challenge. Studies show that men often underreport symptoms, miss routine check-ups, and avoid mental health services entirely.
Even when health systems are technically available to all, they may not be equally accessible. Health information campaigns may use language or imagery that resonates more with women. Clinic hours might be better suited to women’s schedules. Medications might be prescribed in ways that don’t account for differences in body weight, metabolism, or even life expectancy.
Gender Is Not Biology: The Power of Social Construct
It’s important to distinguish between sex, which refers to biological differences, and gender, which refers to social roles and expectations. While some health disparities do stem from biological differences—such as hormonal influences or genetic predispositions—many are shaped more by culture than chromosomes.
Professors Kent Buse and Sarah Hawkes, co-founders of the gender equity initiative Global 50/50, stress that the key lies in recognizing how socially-constructed gender norms shape health behaviors and access. “Most of these differences are not explained by sex (biology) alone, but by socially-constructed gender—highlighting the importance of taking a gender justice approach to reducing health inequities.”
In other words, it’s not just that men and women are biologically different. It’s that we treat them differently, expect different things of them, and provide health services in ways that reinforce those expectations.
A Path Forward: From Data to Justice
The solution, say experts, lies not in ignoring gender, but in embracing it thoughtfully and analytically. That begins with better data. Without reliable, sex-disaggregated statistics, we cannot see the true scope of the problem—let alone fix it. Every health system needs to examine its own data, ask who is being left behind, and design interventions that target those gaps.
Second, public health messaging must evolve. Campaigns that normalize care-seeking for men, especially in mental health and chronic disease management, can be transformative. Male-friendly spaces in clinics, flexible hours, and male outreach workers could help break down long-standing stigmas.
Third, we need gender-aware training for healthcare providers. Doctors, nurses, and administrators must be equipped to recognize how gender influences symptoms, reporting, and adherence. They must also question their own biases—conscious or not.
Finally, policies must be reshaped to reflect true equity, not just equality. That means directing resources where they are most needed, whether that’s increasing outreach to men for diabetes screening, tailoring HIV education to match the cultural context, or addressing domestic violence as a driver of poor health outcomes for women.
Conclusion: Health for All Means Looking Deeper
The findings of Angela Chang and colleagues ring like a wake-up call: health systems cannot afford to be gender-blind. If we want to achieve truly universal health coverage, we must acknowledge and address the diverse journeys that people take through the healthcare system—journeys that are shaped not only by biology, but by culture, identity, and expectation.
Men, often assumed to be the stronger sex, are in many cases the more vulnerable one—not because of what they are, but because of how society tells them to behave. Meanwhile, women continue to face their own unique challenges, not just in disease burden but in care and autonomy.
Only by recognizing these differences and acting on them can we build a future where health is not a privilege of gender, but a right for everyone.
Reference: Feraldi A, et al. Sex-disaggregated data along the gendered health pathways: A review and analysis of global data on hypertension, diabetes, HIV, and AIDS. PLOS Medicine (2025). DOI: 10.1371/journal.pmed.1004592