If the body were an orchestra, the female reproductive system would be the conductor of one of nature’s most profound performances: the creation of life. Hidden deep within the pelvis, largely unseen and often misunderstood, this system does far more than enable pregnancy. It is an intricate biological mechanism, a hormonal powerhouse, and a marvel of engineering that connects cycles, emotions, health, and identity.
The female reproductive system is not just about reproduction—it’s about regulation, transformation, renewal, and resilience. To understand it is to glimpse how biology shapes us all—from our first breath to our last heartbeat.
This article explores the female reproductive system in its full glory: from anatomy and hormones to menstruation, fertility, and beyond. Along the way, we’ll demystify the cycles, clarify the complexities, and marvel at the evolutionary elegance of the machinery of life.
The Architecture of Creation: Organs of the Female Reproductive System
Let’s begin with the basics: what is the female reproductive system made of?
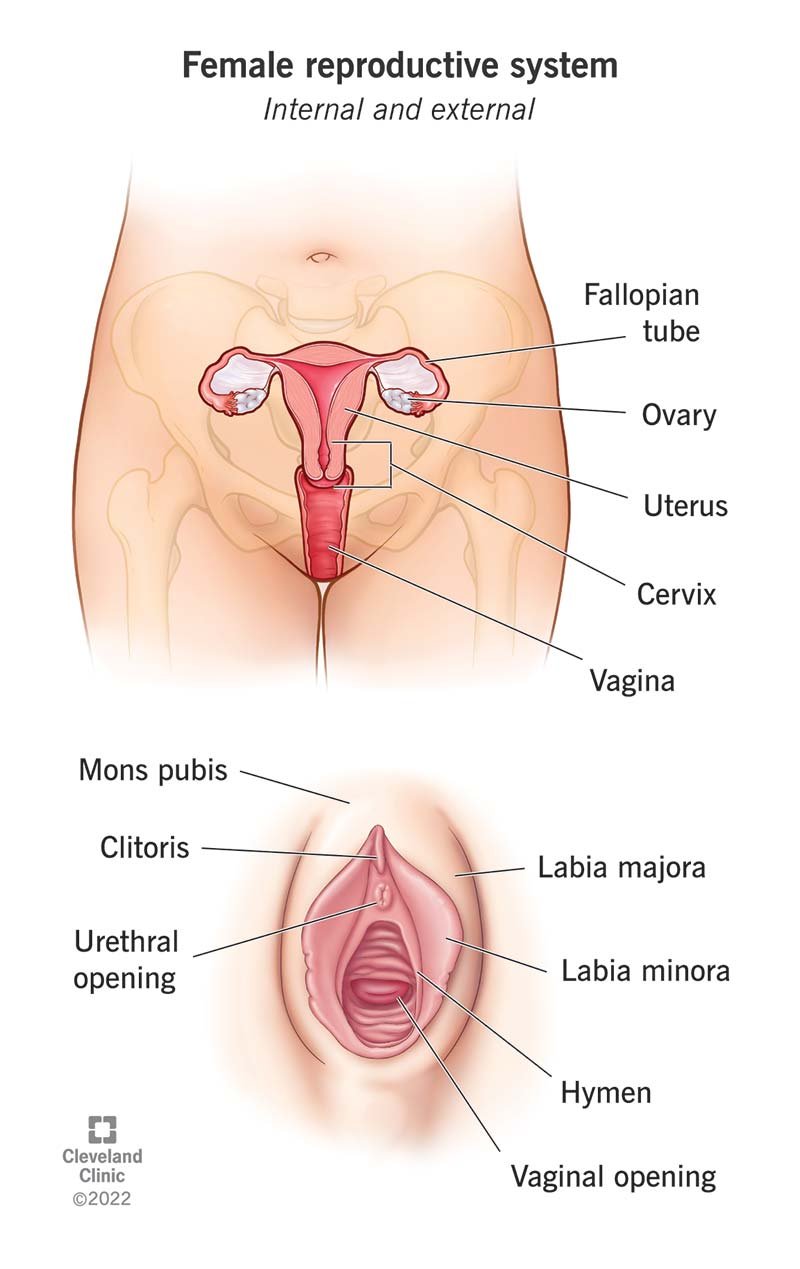
The core organs are divided into two categories—external and internal—each playing a vital role in the complex dance of hormones, cycles, and functions that define this system.
External Structures: The Vulva and Beyond
Often confused with the vagina, the vulva is the collective name for the external genital structures. These include:
- Mons pubis: the fatty tissue over the pubic bone, typically covered with pubic hair after puberty.
- Labia majora and labia minora: the outer and inner lips of the vulva, which protect the internal genitalia and contain sweat and oil-secreting glands.
- Clitoris: a highly sensitive organ with more than 8,000 nerve endings, playing a central role in sexual pleasure.
- Urethral opening: through which urine exits the body.
- Vaginal opening: leading to the internal reproductive organs.
The vulva is the gateway, offering both protection and sensation.
Internal Organs: The Reproductive Core
Here’s where the magic happens—inside the body, out of sight but never inactive:
- Vagina: a muscular, elastic canal that connects the external genitals to the uterus. It serves as the passageway for menstrual flow, sexual intercourse, and childbirth.
- Uterus (womb): a pear-shaped, muscular organ that houses and nourishes a fetus during pregnancy. Its inner lining, the endometrium, thickens monthly in preparation for a possible embryo.
- Cervix: the narrow, lower part of the uterus that opens into the vagina. It produces mucus that changes in consistency throughout the cycle, aiding or preventing sperm movement.
- Fallopian tubes: slender tubes extending from each side of the uterus toward the ovaries. These are the sites of fertilization, where sperm and egg unite.
- Ovaries: the female gonads, two almond-shaped structures that produce eggs (ova) and secrete hormones such as estrogen and progesterone.
Together, these organs form a system that not only makes reproduction possible but also influences overall health, development, mood, and aging.
The Menstrual Cycle: Nature’s Calendar
Central to the female reproductive system is the menstrual cycle—a 28-day (on average) hormonal rhythm that prepares the body for pregnancy and sheds the uterine lining if fertilization doesn’t occur. It’s an elegant, self-regulating cycle that affects nearly every system in the body, not just the reproductive organs.
Phase 1: Menstruation (Day 1–5)
The cycle begins with menstruation, the shedding of the endometrial lining through the vagina. This happens when a fertilized egg doesn’t implant in the uterus and hormone levels—particularly progesterone—drop. The result is a discharge of blood, mucus, and uterine tissue lasting anywhere from 3 to 7 days.
Though often framed as a nuisance, menstruation is actually a sign of a healthy and responsive reproductive system.
Phase 2: The Follicular Phase (Day 1–13)
Overlapping with menstruation, this phase begins on the first day of the cycle. The pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the ovaries to develop follicles. Each follicle contains an immature egg.
As the follicles mature, the ovaries begin producing estrogen, which helps rebuild the uterine lining and signals to the body that ovulation is approaching.
Usually, only one follicle becomes dominant—the one destined to release an egg.
Phase 3: Ovulation (Day 14)
Ovulation is the biological climax of the menstrual cycle. A surge in luteinizing hormone (LH) causes the dominant follicle to burst, releasing the mature egg from the ovary into the fallopian tube.
This egg has about 12–24 hours to be fertilized by sperm. If it is, it continues down to the uterus to implant. If not, it will disintegrate.
Ovulation is often accompanied by subtle signs—slight pain, increased libido, or changes in cervical mucus consistency—and it’s the window of peak fertility.
Phase 4: The Luteal Phase (Day 15–28)
After releasing the egg, the ruptured follicle transforms into the corpus luteum, a temporary endocrine structure that secretes progesterone and some estrogen. These hormones prepare the uterus for a potential pregnancy by thickening the endometrial lining.
If the egg is not fertilized, the corpus luteum shrinks, progesterone drops, and the endometrium begins to break down. The next period begins, and the cycle repeats.
This 28-day hormonal rhythm governs not only reproductive readiness but also mood, energy levels, skin health, and even sleep patterns.
Hormonal Command Center: The Endocrine Control System
While the reproductive organs are the visible actors, the hypothalamus, pituitary gland, and ovaries act as directors behind the scenes.
The Hypothalamus: The Master Switch
Located in the brain, the hypothalamus detects hormone levels in the blood and responds by releasing gonadotropin-releasing hormone (GnRH). GnRH is the first domino that triggers the pituitary gland to release FSH and LH.
The Pituitary Gland: The Hormonal Conductor
Situated below the brain, the pituitary gland secretes FSH and LH, which then influence the ovaries to mature eggs, ovulate, and produce hormones.
The Ovaries: Dual Roles
The ovaries not only release eggs but also act as endocrine glands, producing estrogen and progesterone—the hormones that regulate the menstrual cycle, impact secondary sex characteristics, and support pregnancy.
Together, this hormonal axis is sometimes referred to as the hypothalamic-pituitary-ovarian (HPO) axis, a finely tuned system of feedback loops that keeps everything in balance.
Puberty: The Beginning of the Reproductive Journey
For girls, the reproductive system “wakes up” during puberty, typically between ages 8 and 13. Under the influence of hormones, dramatic changes occur:
- Breasts begin to develop.
- Pubic and underarm hair grows.
- Menstruation begins (menarche).
- The body gains fat, especially around hips and thighs, as it prepares for potential childbearing.
These changes can be confusing or even overwhelming, but they are part of a natural transformation designed to prepare the body for adulthood and fertility.
Fertility and Conception: When It All Comes Together
When sperm meets egg under the right conditions, a new human life can begin.
After ovulation, the egg travels down the fallopian tube. If sperm are present (usually from intercourse within five days prior), fertilization can occur.
The fertilized egg, now called a zygote, divides rapidly and becomes a blastocyst by the time it reaches the uterus. There, it implants into the uterine wall, triggering pregnancy.
The body responds with a flood of hormones—especially human chorionic gonadotropin (hCG), the hormone detected by pregnancy tests. The menstrual cycle pauses, and the uterus transforms into a nurturing cradle for the developing fetus.
Pregnancy: Transformation and Triumph
Pregnancy is not just the presence of a fetus—it’s a physiological revolution.
The uterus expands from the size of a pear to the size of a watermelon. Blood volume increases by nearly 50%. Hormones surge to maintain the pregnancy, prepare the body for birth, and shape the baby’s development.
The placenta, a temporary organ, forms to provide nutrients, oxygen, and waste removal for the fetus. It also produces hormones, making it a critical part of the endocrine system during pregnancy.
The cervix softens, the pelvis loosens, and the breasts prepare to produce milk. Every part of the reproductive system—and beyond—adapts to this monumental task.
Childbirth: The Culmination of Creation
When pregnancy reaches full term (about 40 weeks), the body initiates labor, a complex series of hormonal and muscular events that result in childbirth.
The uterus contracts rhythmically, the cervix dilates, and the baby moves down the birth canal. It is a process of pain, strength, endurance, and often joy. After delivery, the placenta is expelled, and the reproductive system begins its slow return to its pre-pregnancy state.
Childbirth is a biological act, but also a deeply emotional and often spiritual experience, rooted in the deepest capabilities of the female body.
Menopause: The End of Reproductive Life, Not of Life Itself
Around the ages of 45–55, most women experience menopause—the natural end of menstruation and fertility.
Ovarian function declines, estrogen and progesterone levels drop, and the menstrual cycle stops. This transition can take several years (known as perimenopause) and involves symptoms like hot flashes, mood swings, and sleep disturbances.
But menopause is not an end—it’s a new beginning. It marks a phase of freedom from the hormonal ups and downs of the cycle, and many women experience a resurgence in energy, confidence, and purpose.
Disorders of the Reproductive System
Like any system, the female reproductive system is vulnerable to disorders:
- Endometriosis: growth of uterine tissue outside the uterus, causing pain and infertility.
- Polycystic Ovary Syndrome (PCOS): a hormonal imbalance affecting ovulation, periods, and fertility.
- Uterine fibroids: benign growths in the uterus that can cause heavy bleeding or discomfort.
- Cervical, ovarian, and uterine cancers.
- Pelvic Inflammatory Disease (PID): infection of reproductive organs, often caused by sexually transmitted infections (STIs).
- Infertility, which can have various causes, from ovulatory disorders to structural issues.
Early detection, regular gynecological care, and open conversations about reproductive health are crucial in addressing these issues.
The Emotional and Cultural Dimensions
The female reproductive system is not just biological—it is deeply tied to identity, culture, emotion, and experience.
Menstruation, fertility, childbirth, and menopause are experienced differently around the world, influenced by beliefs, taboos, and social norms. In some cultures, menstruation is celebrated; in others, it is shrouded in secrecy.
The reproductive system is also deeply connected to sexuality—a powerful part of human expression and intimacy. Understanding the body can empower individuals to make informed decisions about pleasure, safety, and consent.
Conclusion: A System of Strength and Beauty
The female reproductive system is one of nature’s most intricate creations. It is capable of cycles, self-renewal, healing, pleasure, and even growing new life. From menstruation to menopause, it tells a story of change, resilience, and power.
To understand it is to respect it. To respect it is to protect it.
Whether you’re learning for the first time or deepening your knowledge, one truth becomes clear: the female reproductive system is not just a biological feature—it is a marvel of life itself.