Inflammation is often misunderstood. To many, the word conjures up images of redness, swelling, or aching joints. But at its core, inflammation is not an enemy—it’s a guardian. It’s the body’s natural response to injury, infection, or harmful stimuli, a primal and ancient biological mechanism that helps us heal and survive. Like a fire alarm triggering a response team, inflammation mobilizes immune cells to the site of trouble, cleans up damaged tissue, and initiates repair.
However, like a fire that rages out of control, inflammation can become destructive. When it fails to shut off, or when it is triggered unnecessarily, it begins to harm the very tissues it was meant to protect. In this way, chronic inflammation acts as a silent saboteur—a slow burn that contributes to some of the most debilitating diseases of modern life, including heart disease, diabetes, cancer, Alzheimer’s, and autoimmune disorders.
Understanding inflammation, therefore, means more than simply knowing what causes a swollen ankle or a sore throat. It means looking at one of biology’s oldest survival systems and seeing how, in the modern world, it sometimes betrays us.
The Ancient Defense Mechanism
To grasp inflammation’s importance, we must go back in evolutionary time. Long before the development of antibiotics or vaccines, our immune system was the first and last line of defense. It evolved not just to eliminate pathogens, but to sense when something in the body was amiss—when cells were dying, invaders had breached barriers, or tissues had suffered trauma.
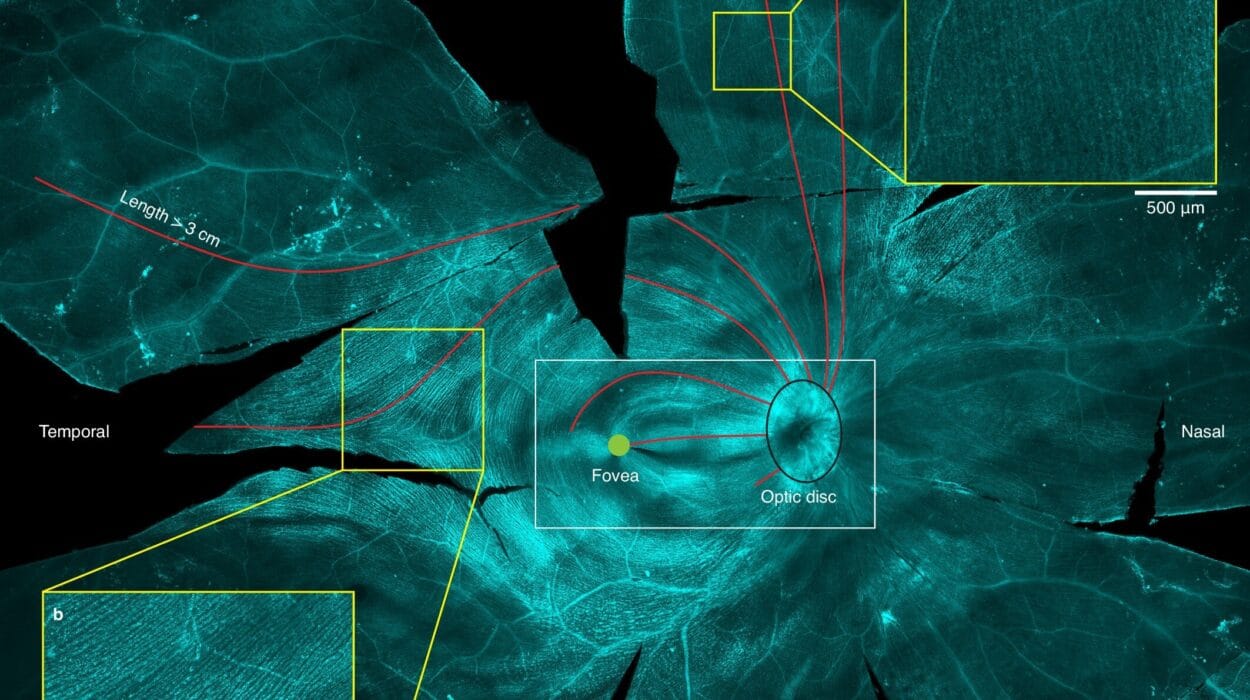
Inflammation begins with the immune system’s early warning network. Specialized cells called sentinel macrophages, mast cells, and dendritic cells patrol tissues constantly, scanning for danger. They look not just for foreign invaders like bacteria or viruses, but for signs of cellular stress and damage—molecules released when cells die, rupture, or lose function. These “danger signals” spark an alarm.
In response, blood vessels in the affected area dilate and become more permeable. This allows immune cells and plasma proteins to rush in. The swelling and redness of inflammation come from this sudden influx. Pain results from chemical signals that sensitize nerves, alerting the brain that something is wrong. Heat—a hallmark of inflammation—is the result of increased blood flow and metabolic activity in the area.
This is the classic image of acute inflammation: rapid, aggressive, and usually self-limiting. Once the threat is neutralized and cleanup is underway, anti-inflammatory signals take over. These tell immune cells to stand down, restore balance, and rebuild.
In acute situations—say, a bacterial infection or a sprained ankle—this process is essential and life-saving. But if the system fails to turn off, or if the body keeps sensing danger where there is none, inflammation becomes chronic. It no longer heals—it harms.
Chronic Inflammation: The Hidden Threat
Unlike acute inflammation, which is loud and unmistakable, chronic inflammation is stealthy. It simmers rather than erupts. You might not feel sick. There may be no obvious swelling or redness. But under the surface, the immune system is stuck in a loop, producing low levels of inflammatory molecules that continue to affect tissues over weeks, months, or years.
This kind of inflammation is insidious because it is often misdirected or overreactive. Sometimes it responds to internal triggers—like abnormal proteins, dead cells, or metabolic byproducts. In other cases, it arises from lifestyle factors: a high-sugar diet, obesity, smoking, chronic stress, or environmental toxins.
What makes chronic inflammation especially dangerous is its ripple effect. Over time, it damages DNA, impairs cell function, and degrades tissue architecture. It wears down organs like rust on metal or termites in a wooden beam. And because this erosion happens gradually, it often goes unnoticed until disease has firmly taken hold.
Inflammation and Cardiovascular Disease
One of the most well-studied relationships in medicine is the link between chronic inflammation and heart disease. For decades, doctors believed that heart attacks were simply the result of high cholesterol clogging arteries. But research has revealed a far more complex story—one in which inflammation plays a starring role.
Atherosclerosis, the buildup of plaques inside arteries, begins not just with fat deposition but with immune activity. When low-density lipoprotein (LDL) cholesterol infiltrates the arterial wall, immune cells treat it as a threat. They release cytokines and oxidative enzymes, triggering inflammation and attempting to wall off the damage. But this response makes things worse. Over time, the plaques become inflamed, unstable, and prone to rupture. When they break apart, they can form clots that block blood flow to the heart or brain, causing heart attacks or strokes.
Elevated levels of C-reactive protein (CRP), an inflammatory marker, are now recognized as a strong predictor of cardiovascular events—sometimes even more so than cholesterol levels. And anti-inflammatory drugs like canakinumab have shown promise in reducing the risk of heart attacks, independent of lipid control. This has revolutionized how doctors think about heart health: not just as a matter of fat, but of fire.
Inflammation and Metabolic Dysfunction
Chronic inflammation also plays a central role in metabolic diseases, especially type 2 diabetes. Here, the trouble begins with insulin resistance—when cells stop responding to insulin, the hormone that signals them to take up glucose from the blood. For years, this was seen as a metabolic problem. But inflammation, it turns out, is deeply intertwined.
Adipose tissue, especially visceral fat around the abdomen, is not just an energy store—it’s a hormonally active organ. In obesity, fat cells grow larger and more dysfunctional. They attract immune cells, particularly macrophages, which begin secreting inflammatory cytokines like TNF-alpha and IL-6. These interfere with insulin signaling pathways, making it harder for glucose to enter cells and raising blood sugar levels.
This creates a vicious cycle: inflammation leads to insulin resistance, which leads to more glucose and fat in the blood, which promotes more inflammation. Over time, this contributes to the full spectrum of metabolic syndrome—obesity, high blood pressure, abnormal lipids, and increased risk of cardiovascular disease.
Efforts to treat diabetes have begun to recognize this inflammatory component. Some experimental therapies target immune pathways directly. Even weight loss, exercise, and healthy eating appear to exert part of their benefit not just by reducing fat, but by calming inflammation.
Neuroinflammation: The Brain on Fire
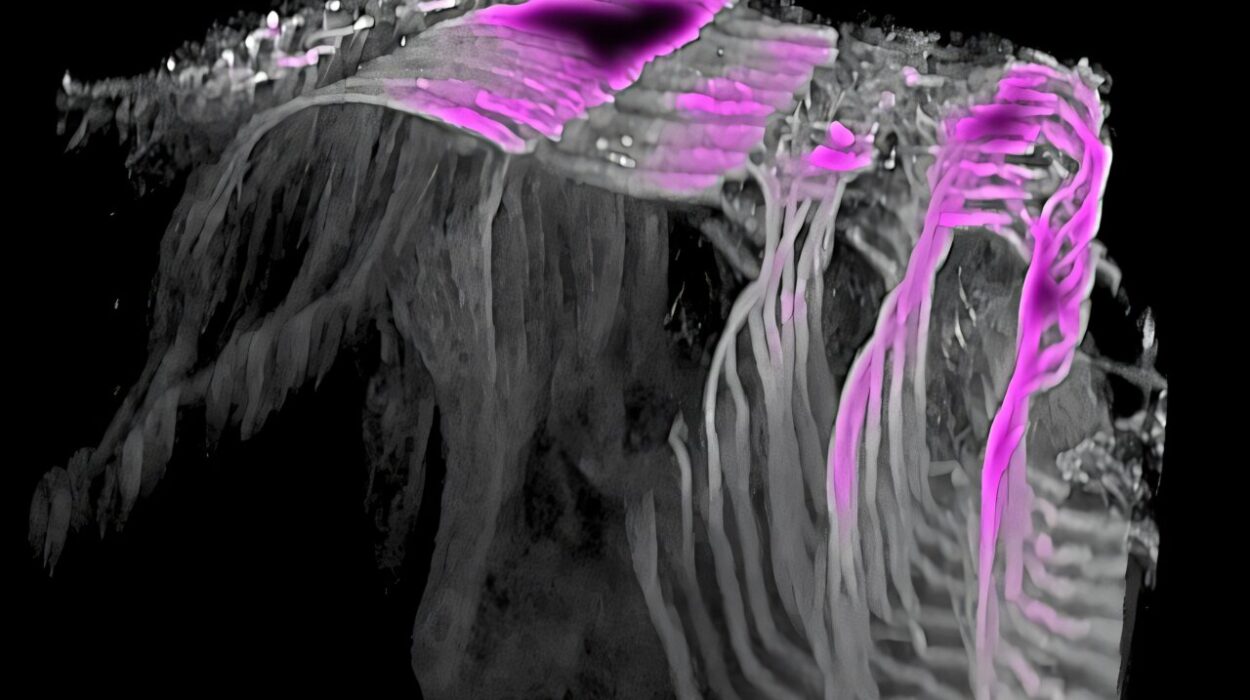
For many years, the brain was thought to be immune-privileged—a fortress protected from immune activity by the blood-brain barrier. But modern research has shattered that illusion. The brain has its own immune cells, called microglia, and when these cells become overactive, they can produce a storm of inflammatory signals that damage neurons.
This process, known as neuroinflammation, is now implicated in a wide array of neurological and psychiatric disorders, including Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and even depression. In Alzheimer’s, for instance, the brain accumulates amyloid-beta plaques and tau tangles. But it’s not just these abnormal proteins that cause damage—it’s the immune system’s response to them. Microglia surround the plaques and release inflammatory mediators that harm nearby neurons.
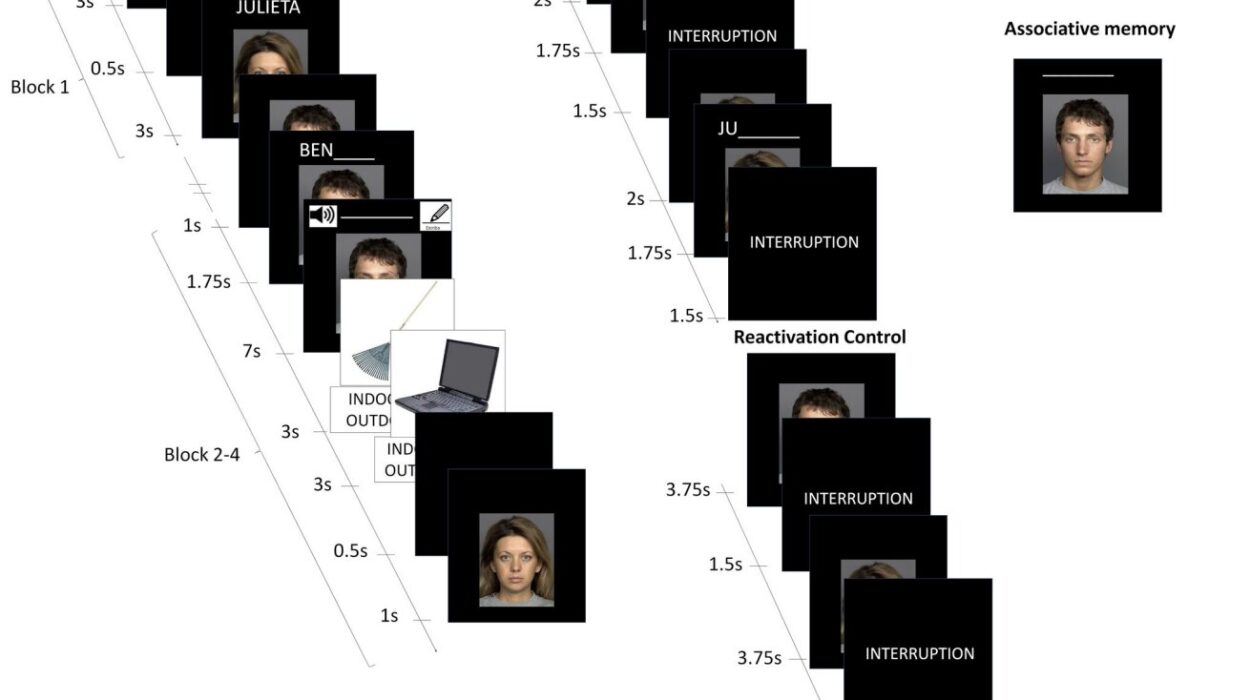
Recent studies have shown that people with high levels of systemic inflammation are more likely to experience cognitive decline. Inflammatory markers like CRP and IL-6 are elevated in individuals with dementia, and anti-inflammatory medications are being explored as potential treatments for neurodegenerative diseases.
Even in depression—a condition traditionally viewed through a chemical imbalance lens—inflammation is gaining ground as a contributing factor. Elevated cytokines have been found in many patients with depression, and anti-inflammatory drugs are being tested for their antidepressant potential.
Inflammation and Cancer: A Dangerous Liaison
Cancer and inflammation have a complicated relationship. On one hand, the immune system is essential for identifying and destroying cancer cells before they grow. On the other, chronic inflammation can create a fertile ground for cancer to develop and thrive.
Inflammatory environments are rich in growth factors, blood vessel promoters, and enzymes that remodel tissue—all conditions that favor tumor growth. Moreover, inflammatory mediators can cause DNA mutations, prevent normal cell death, and suppress immune surveillance. This is why chronic inflammatory conditions—like hepatitis (liver), gastritis (stomach), colitis (colon), and certain viral infections—are associated with higher cancer risk.
For example, in inflammatory bowel disease, ongoing immune activity in the colon increases the risk of colorectal cancer. In chronic hepatitis, the liver is constantly inflamed, raising the risk of hepatocellular carcinoma. Even smoking-induced inflammation in the lungs is a major driver of lung cancer.
Targeting inflammation is an emerging strategy in oncology. Drugs like aspirin, which reduce inflammation, are being studied for their ability to lower cancer risk or improve outcomes in certain patients. Some immunotherapies also seek to redirect the immune system from a pro-tumor to an anti-tumor mode.
Autoimmunity: When the Body Turns on Itself
Nowhere is the destructive potential of inflammation more evident than in autoimmune diseases. These conditions arise when the immune system mistakes the body’s own tissues for invaders and mounts an attack. The result is self-inflicted inflammation, often chronic and disabling.
Diseases like rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes are driven by misdirected immune responses. In rheumatoid arthritis, the joints become inflamed as immune cells infiltrate the synovial lining. In lupus, inflammation spreads across multiple organs, including the skin, kidneys, and brain. In multiple sclerosis, immune cells attack the myelin sheath around nerves, disrupting signal transmission.
What triggers autoimmunity remains partly mysterious, but genetic predisposition, infections, hormonal factors, and environmental exposures all seem to play a role. Treatments typically focus on suppressing inflammation—using steroids, immunosuppressants, or biologic drugs that block specific inflammatory pathways.
The goal in these diseases is not to silence the immune system entirely but to restore balance—to rein in the fire without extinguishing the necessary sparks that keep us alive.
The Inflammatory Lifestyle
While some inflammation is unavoidable, much of it is influenced by how we live. Diet, exercise, stress, sleep, and environment all shape the inflammatory landscape of our bodies.
Diets high in processed sugars, refined carbs, and saturated fats promote inflammation, while diets rich in fruits, vegetables, whole grains, fatty fish, and olive oil—like the Mediterranean diet—tend to reduce it. Physical activity helps regulate immune responses and decrease pro-inflammatory markers. Chronic stress, by contrast, raises cortisol levels and can provoke a state of low-grade inflammation. Poor sleep disrupts immune rhythms. Environmental toxins like air pollution, cigarette smoke, and certain industrial chemicals can all trigger inflammatory responses.
Modern life, with its fast food, sedentary habits, and chronic psychological stress, creates a perfect storm for inflammation to persist. The very things that make our lives easier often fan the flames of disease beneath the surface.
Toward an Anti-Inflammatory Future
The future of medicine may well hinge on our ability to understand and control inflammation. Already, anti-inflammatory therapies are revolutionizing treatment across specialties—from cardiology to oncology, neurology to psychiatry.
But perhaps the most exciting frontier is personalized inflammation profiling. Just as we measure blood pressure and cholesterol, future check-ups may include inflammatory biomarkers. This could allow doctors to detect disease risk early, tailor therapies, and monitor responses more precisely.
In parallel, research into the microbiome—the vast community of microbes in our guts—is revealing how profoundly these organisms influence our inflammatory status. A healthy, diverse microbiome appears to regulate immune tolerance and keep inflammation in check. Probiotics, prebiotics, and microbiota transplants may one day become tools in the anti-inflammatory arsenal.
Gene editing technologies like CRISPR could also open new doors, allowing us to correct faulty immune pathways at their source. And regenerative medicine may help repair tissues already damaged by years of inflammatory assault.
The Balancing Act
Inflammation is not inherently evil. It is a tool—powerful, ancient, and indispensable. But like all tools, it must be used wisely. When it strikes in precision, we heal. When it burns out of control, we suffer.
In understanding inflammation, we come to appreciate the delicate balance that sustains life. We glimpse the immune system not as a warrior always at war, but as a conductor—tuning its responses to the music of health and disease.
The more we learn, the better we can protect ourselves not by fighting inflammation blindly, but by restoring harmony to a system that was designed, above all, to preserve us.