Pain is a quiet thief. It tiptoes into your joints, day after day, stealing comfort, freedom, and sometimes even joy. For millions around the globe, this thief has a name—arthritis. It’s not just a disease of old age. It doesn’t just arrive with wrinkles or gray hair. Arthritis can strike the young, burden the active, and change the life of someone overnight.
But while arthritis is one of the most common chronic health problems worldwide, it’s also deeply misunderstood. It’s not just one condition, but rather an umbrella term for over 100 different types of joint-related diseases. It can affect the joints, the tissues surrounding them, and even other organs in the body.
So what is arthritis, really? What causes it? How do we detect it, and what can be done to live with it—truly live, not merely exist in its shadow?
Let’s take a journey not just through the clinical aspects of arthritis but into its very human heart—a condition shaped by biology, yet experienced by people.
Understanding Arthritis: More Than Just Joint Pain
At its core, arthritis refers to inflammation of one or more joints. “Arthro” means joint, and “itis” means inflammation. While inflammation is the body’s natural defense mechanism against injury or infection, in arthritis, it becomes chronic and misdirected.
Imagine the hinge of a door slowly rusting. The parts still move, but they creak, they resist. In arthritis, that creaking happens inside you—stiffness when you wake, swelling after movement, or a sharp jolt that reminds you every step is a negotiation with pain.
But arthritis doesn’t look the same in everyone. For some, it’s a dull ache in the knees. For others, it’s the burning of swollen fingers or the invisible exhaustion of systemic inflammation.
The two most common types are:
- Osteoarthritis (OA) – often called “wear-and-tear” arthritis.
- Rheumatoid Arthritis (RA) – an autoimmune form of arthritis.
Yet there are many others: psoriatic arthritis, juvenile idiopathic arthritis, gout, ankylosing spondylitis, lupus-related arthritis, and more. Each has its own story, its own cause, and its own impact.
The Root of the Ache: Causes of Arthritis
The causes of arthritis are as varied as the people it affects. Some types are driven by genetics, others by environmental triggers, injury, or an overzealous immune system.
1. Osteoarthritis: The Slow Erosion of Time
Osteoarthritis is the most common form and usually develops with age. It affects the cartilage—the smooth tissue that cushions the ends of bones at the joints. As cartilage wears down, bones begin to rub against each other, causing pain, swelling, and loss of motion.
But OA isn’t just about aging. It can also result from:
- Joint injuries (like a torn ACL or dislocation)
- Repetitive stress from sports or occupation
- Obesity, which adds pressure and inflammation
- Genetic predisposition
Over time, the affected joint may change shape, and bony spurs may develop. For some, OA is mild; for others, it can be deeply disabling.
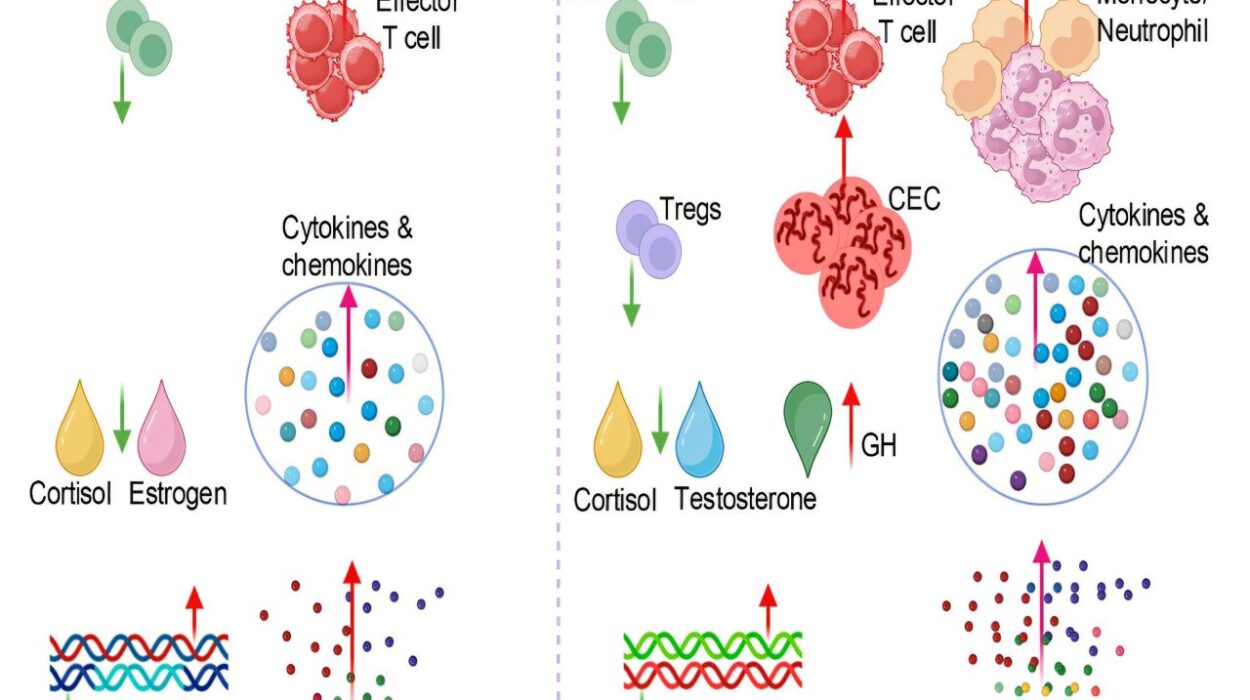
2. Rheumatoid Arthritis: When the Immune System Turns Rogue
Rheumatoid arthritis is not caused by wear and tear. It’s an autoimmune disease, where the body’s immune system mistakenly attacks its own joint tissues—particularly the synovium, the lining of the joints.
This immune misfire causes:
- Inflammation of the joints
- Swelling and warmth
- Pain and stiffness, especially in the morning
- Progressive joint damage
Over time, RA can lead to joint deformity and may affect organs like the lungs, heart, and eyes. The exact cause remains unclear, but it likely involves a complex mix of:
- Genetics (such as HLA-DR4 gene variants)
- Environmental factors (e.g., smoking)
- Hormonal influences
3. Other Forms and Causes
- Gout is caused by uric acid crystals building up in joints.
- Psoriatic arthritis affects some people with psoriasis.
- Lupus and ankylosing spondylitis involve systemic inflammation.
- Reactive arthritis follows infections.
- Juvenile idiopathic arthritis affects children, often with unknown cause.
In all these conditions, inflammation is the common thread—but what triggers it, and how it expresses itself, varies greatly.
The Body Speaks: Symptoms of Arthritis
Arthritis is more than just a list of symptoms; it is a lived experience. But medically, symptoms can help doctors narrow down the type and severity of the condition.
Common Symptoms Across Types:
- Joint pain (dull, aching, or sharp)
- Swelling in the affected joints
- Stiffness, especially in the morning or after rest
- Reduced range of motion
- Warmth or redness over the joint
Systemic Symptoms in Autoimmune Forms:
- Fatigue that doesn’t go away with rest
- Fever or malaise
- Weight loss
- Dry eyes or mouth (especially in Sjögren’s syndrome)
- Rashes or nodules
For many, the symptoms come and go in flares—periods of heightened activity followed by relative calm. These unpredictable cycles can wreak havoc on a person’s work, relationships, and mental health.
Diagnosing the Invisible: Testing for Arthritis
Diagnosing arthritis can be surprisingly complex. There is no single “arthritis test.” Instead, doctors rely on a combination of tools to piece together the puzzle.
1. Medical History and Physical Examination
The journey starts with a thorough history:
- When did symptoms begin?
- Which joints are affected?
- Is there a family history of arthritis?
- Are there signs of systemic disease?
During the physical exam, doctors check for:
- Joint swelling or deformities
- Range of motion
- Warmth or tenderness
- Muscle strength and reflexes
2. Imaging Tests
Imaging helps visualize joint damage and rule out other causes.
- X-rays show joint space narrowing, bone spurs, or erosion.
- MRI and ultrasound detect early inflammation and soft tissue damage.
- CT scans provide detailed cross-sectional views, especially in complex joints like the spine.
3. Laboratory Tests
Blood and fluid tests help differentiate types of arthritis.
- Rheumatoid factor (RF) and anti-CCP antibodies – often positive in RA
- ANA (antinuclear antibodies) – suggestive of lupus
- ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) – markers of inflammation
- Uric acid levels – elevated in gout
- Synovial fluid analysis – may show crystals, bacteria, or inflammatory cells
4. Arthroscopy
In some cases, a small camera is inserted into the joint to directly observe damage—especially if diagnosis remains uncertain.
Getting a diagnosis can take time, and for many, that waiting period is filled with anxiety. But proper diagnosis is crucial, because the treatments for one type of arthritis may be ineffective—or even harmful—for another.
Paths Toward Relief: Treating Arthritis
There is no universal cure for arthritis, but modern medicine offers a wide toolkit to reduce symptoms, slow disease progression, and improve quality of life. The best treatment plans are multifaceted—combining medication, lifestyle changes, physical therapy, and sometimes surgery.
1. Medications: From Pain Relief to Disease Control
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): Ibuprofen and naproxen reduce pain and inflammation.
- Acetaminophen: Offers pain relief without anti-inflammatory effects.
- Corticosteroids: Potent inflammation fighters, used short-term.
- DMARDs (Disease-Modifying Antirheumatic Drugs): Used in RA and other autoimmune forms to slow progression (e.g., methotrexate, sulfasalazine).
- Biologic agents: Target specific immune system pathways (e.g., TNF inhibitors like adalimumab or IL-6 inhibitors).
- JAK inhibitors: A newer class of oral drugs that interfere with immune signaling.
- Uric acid reducers: Like allopurinol for gout.
Each medication carries risks, and finding the right one may take trial and error.
2. Physical Therapy and Exercise
Contrary to what many believe, movement is vital for arthritis. Physical therapists can help maintain joint function, reduce stiffness, and build supportive muscle.
- Low-impact exercises like swimming, walking, or tai chi
- Strength training and flexibility routines
- Joint protection techniques and assistive devices
3. Lifestyle Modifications
- Weight management: Reduces pressure on joints
- Anti-inflammatory diets: Rich in omega-3s, fruits, and vegetables
- Heat and cold therapy
- Stress reduction: Meditation, yoga, and mental health support
4. Surgical Interventions
When joint damage becomes severe, surgery may be the best option:
- Joint replacement (knee, hip, shoulder)
- Arthroscopy for cleaning damaged tissue
- Joint fusion in smaller joints
These procedures can be life-changing but require careful consideration and rehabilitation.
The Emotional Landscape of Arthritis
Arthritis doesn’t just affect the joints—it affects the soul. The unpredictability of flares, the loss of mobility, the chronic pain—it all takes a toll on mental health.
Depression and anxiety are common companions to arthritis, yet they are often overlooked. People with arthritis may feel isolated, frustrated, or like a burden. They may grieve for the version of themselves that once moved freely.
Support—both emotional and practical—is essential. This includes:
- Counseling or therapy
- Arthritis support groups
- Open communication with loved ones
- Advocacy and education to fight stigma
Hope on the Horizon: Research and Future Therapies
Science marches on, and the future for arthritis sufferers grows brighter each year.
- Stem cell therapy: Being explored for regenerating cartilage.
- Gene editing (CRISPR): May one day modify immune responses.
- Personalized medicine: Tailoring treatment based on genetic profiles.
- New biologics and small molecules are in development to more precisely control immune pathways.
Early diagnosis and treatment remain key. With advancing tools, some forms of arthritis—once disabling—can now be managed effectively, even reversed in their early stages.
Living Fully, Even with Arthritis
Arthritis may alter the way you live, but it does not have to define your life. From grandparents playing with grandchildren to young professionals navigating careers, millions around the world live rich, full lives despite arthritis.
They adapt. They endure. They innovate.
And while pain may never fully vanish, the combination of modern medicine, personal resilience, and compassionate care offers hope—and power. Power to reclaim motion. Power to find joy in new ways. Power to live beyond the diagnosis.
Arthritis is not the end of the story.
It’s the beginning of a different chapter—one written with courage, science, and an unshakable belief that pain does not get the final word.