Cancer is infamous for its cunning—its ability to infiltrate, disguise, adapt, and most crucially, manipulate. Among its most devious tricks is the hijacking of the very system meant to eliminate it: our immune system. Now, in a groundbreaking study, researchers at the Weizmann Institute of Science have cracked a major code in cancer’s playbook. Using advanced gene-editing, single-cell analysis, and artificial intelligence, the team discovered a genetic “master switch” that flips immune cells from cancer accomplices to cancer combatants.
This discovery, published in the journal Cancer Cell, doesn’t just advance our understanding of tumor biology—it opens an exciting new frontier in cancer therapy.
The Double Life of Macrophages
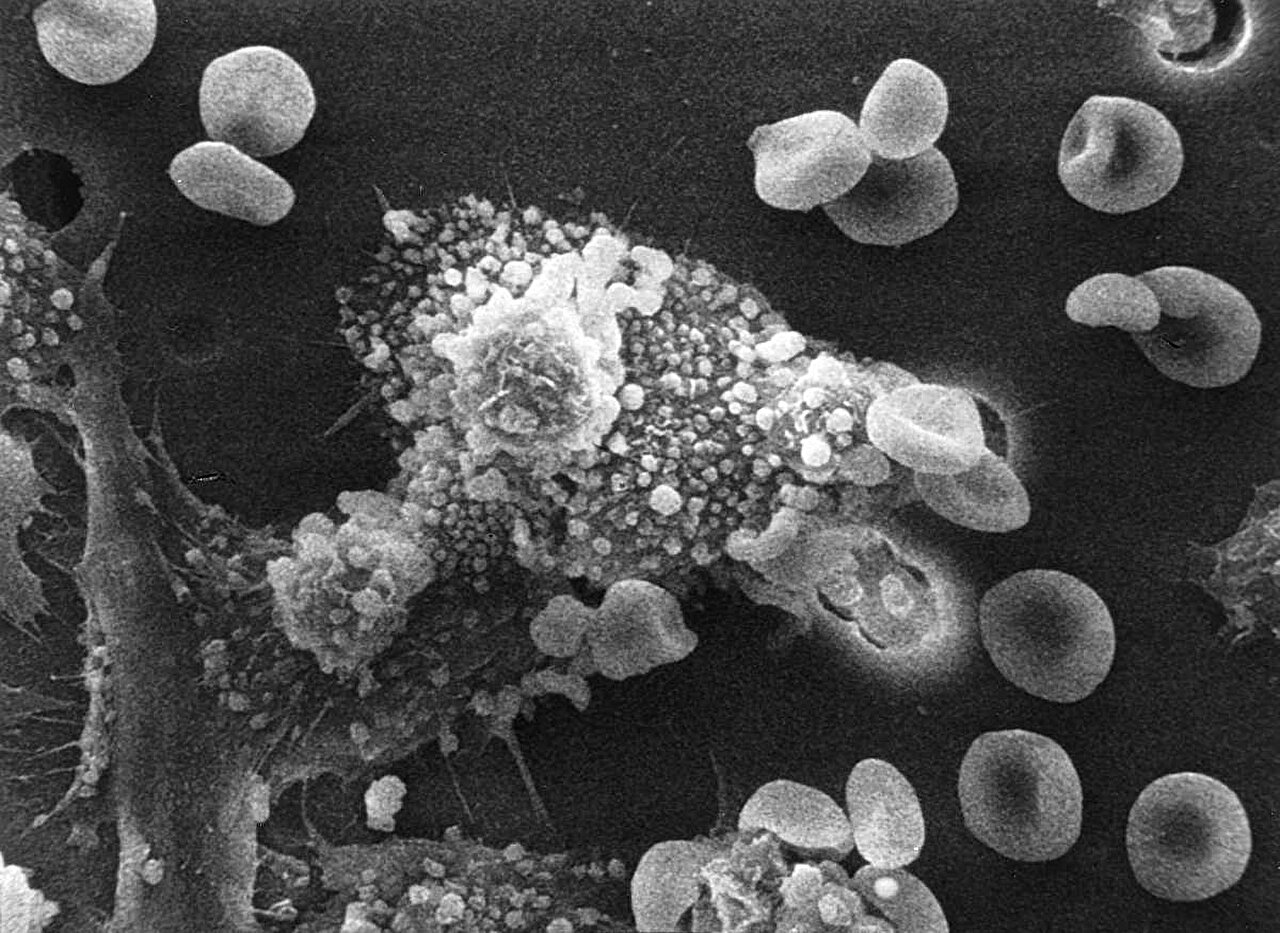
At the heart of this research lies a highly versatile and enigmatic immune cell: the macrophage. Often described as the “Swiss Army knife” of the immune system, macrophages are cellular multitaskers. They hunt down pathogens, clean up cellular debris, initiate inflammation when needed, and alert the immune cavalry when danger arises. But their complexity is also their Achilles’ heel.
In cancer, these immune sentinels are frequently co-opted and transformed into tumor enablers. Tumor-associated macrophages (TAMs), once defenders, become double agents. Instead of attacking tumors, they create a protective shield around them, suppress other immune cells, stimulate blood vessel formation (angiogenesis), and even help cancer spread to distant organs.
“By doing that,” says Professor Ido Amit, senior author of the study, “tumors protect themselves from the macrophages’ ‘nasty’ side, and instead unleash functions that serve their own growth.”
The consequence? A tumor not just tolerated but actively supported by the immune system—a cellular coup d’état.
Why Past Efforts to Reprogram Macrophages Fell Short
For years, scientists have tried to flip these traitorous macrophages back to their original purpose. Many therapies attempted to categorize macrophages as either “good” (antitumor) or “bad” (protumor), seeking to suppress the latter or promote the former. But this binary framework oversimplified a profoundly intricate reality.
“Those efforts failed because they separated macrophages into two very general categories,” explains Amit. “Today we know that this categorization misses much of the complexity of macrophage function.”
Instead of settling for an outdated dichotomy, Amit’s team turned to the technologies of tomorrow: deep-learning AI, single-cell sequencing, and CRISPR gene editing. Their goal was ambitious—map the full functional landscape of macrophages and find the hidden regulators controlling their behavior.
Enter Zeb2: The Master Switch
The Weizmann team, led by Dr. Fadi Sheban, began by mining macrophage gene expression data from human tumors, building a massive functional atlas of these cells. From this data, they identified 120 genes suspected of influencing the pro- or antitumor behavior of macrophages. But how to know which of these genes really mattered?
Here, the researchers leveraged their cutting-edge platform: a combination of CRISPR-Cas9 gene editing and single-cell RNA sequencing. By deleting each of the 120 candidate genes—one by one—in individual macrophages and then analyzing over 100,000 cells, they generated an extraordinarily rich dataset detailing how each gene tweak altered macrophage function.
But even with this data in hand, the complexity was overwhelming.
“It was a complete mess,” recalls Sheban. “We couldn’t tell which genes were the most important or what they really did.”
That’s when artificial intelligence stepped in. Using a custom deep-learning model named MrVI—developed by Prof. Nir Yosef—the researchers translated their data into a visual map of macrophage behavior. Each gene was represented as a node, connected to patterns of immune activity. Suddenly, the fog cleared.
One gene, Zeb2, lit up like a flare.
“When we silenced Zeb2, the macrophages flipped—from promoting tumor growth to fighting the tumor,” says Sheban. “It was like flipping a master switch.”
Zeb2, it turns out, is not just a molecular regulator—it’s a genomic architect. It reshapes the epigenome, the dynamic structure of DNA that determines which genes are turned “on” or “off.” When Zeb2 is active, it opens the pages of the genome that promote tumor-friendly behavior and slams shut those that support immune attack. Remove it, and the genome rewrites itself to favor cancer destruction.
From Discovery to Therapy: Reprogramming Macrophages in Living Mice
Of course, finding a master switch in a lab dish is only the beginning. The next step was to translate this knowledge into a therapy—one that could actually work inside a living body.
Enter Prof. Marcin Kortylewski from the City of Hope National Medical Center in California. His team had developed a clever delivery system: a DNA molecule that acts like a Trojan horse. This molecule homes in on macrophages and is swallowed by them. Attached to it is a short piece of RNA specifically designed to silence Zeb2.
In a series of experiments, the Weizmann team injected this engineered molecule into the tumors of mice with bladder cancer—a notoriously difficult cancer with limited treatment options. The results were dramatic.
The macrophages were reprogrammed on-site. They stopped helping the tumor and began attacking it. The tumor mass shrank significantly.
“We saw the macrophages become cancer killers again,” says Amit. “This was not just a lab phenomenon—it worked in live organisms.”
A New Frontier in Cancer Immunotherapy
While the therapy is still in the early stages, its implications are profound. First, it shows that reprogramming the immune system is not only possible—it can be achieved with precision. Second, it highlights the enormous potential of combining technologies: genomics, gene editing, artificial intelligence, and targeted drug delivery.
Third, it opens a new chapter in cancer immunotherapy, one that focuses not only on activating T cells (as in checkpoint inhibitors) but also on remodeling the immune environment of the tumor itself.
Most exciting of all, the approach is modular. The same platform used to identify Zeb2 could potentially discover other “master switches” in different immune cells—offering new strategies against a wide range of cancers and even other diseases.
Looking Ahead: Zeb2 and Beyond
The study’s implications reach far beyond bladder cancer. Follow-up analysis of human cancer data revealed that patients with high Zeb2 expression in their macrophages tend to have worse outcomes and more aggressive disease. In other words, this gene is not just a theoretical target—it’s clinically relevant.
The next big challenge? Human trials.
“We’re now working on developing this approach into a viable therapy for patients,” says Amit. “We’ve demonstrated a proof of concept. The next step is scaling up, ensuring safety, and ultimately testing its effectiveness in humans.”
As the world continues to seek smarter, more personalized, and more effective ways to fight cancer, this research marks a thrilling step forward. It shows that sometimes, the key to beating cancer isn’t just attacking it harder—it’s understanding its tactics, outsmarting it at the cellular level, and using the body’s own defenses to turn the tide.
Cancer has long relied on stealth and sabotage. But now, with technologies that peer into the deepest recesses of our immune cells, we may be witnessing the beginning of a new era—one in which cancer’s secrets are no longer safe.
Reference: ZEB2 is a Master Switch Controlling the Tumor-Associated Macrophage Program, Cancer Cell (2025). DOI: 10.1016/j.ccell.2025.03.021. www.cell.com/cancer-cell/fullt … 1535-6108(25)00122-9