Deep within the human body runs the aorta, the largest artery, carrying oxygen-rich blood from the heart to the rest of the body. Most of the time, we don’t think about it. But for millions of people around the world, a section of this critical vessel in the abdomen can slowly weaken and swell like a balloon. This condition, called an abdominal aortic aneurysm, often gives no warning signs until the danger is at its peak.
When an aneurysm ruptures, it can be fatal within minutes. For decades, doctors have had few tools beyond surgery to treat this silent but deadly disease. But now, new research from the Cleveland Clinic points to an unexpected culprit in its development: a molecule produced not by our own cells, but by the bacteria living inside our gut.
What the Cleveland Clinic Discovered
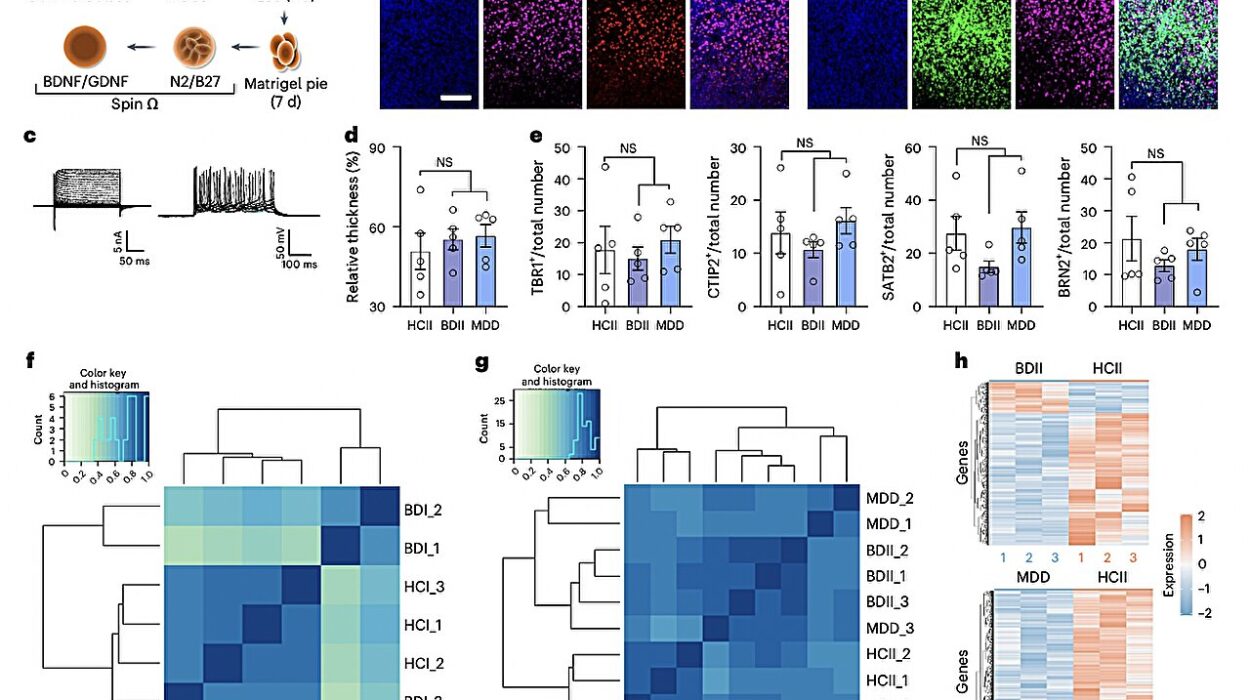
Scientists at the Cleveland Clinic have found that high blood levels of a compound called trimethylamine N-oxide (TMAO) are linked to a greater risk of abdominal aortic aneurysm. Their findings, recently published in JAMA Cardiology, suggest that TMAO may not only contribute to the formation of aneurysms, but also drive their progression and increase the likelihood that patients will eventually need surgery.
“TMAO seems to accelerate aneurysm expansion,” explained Dr. Scott Cameron, section head of Vascular Medicine at Cleveland Clinic and lead author of the study. “Right now, surgery is the only effective treatment we have. If we can target TMAO, we may finally have a way to prevent or slow aneurysm disease before it becomes life-threatening.”
The Role of Gut Bacteria
So where does TMAO come from? The answer lies in the trillions of microbes that live in the human gut. When we eat foods rich in certain nutrients—especially red meat, eggs, and other animal products—gut bacteria digest compounds like choline and carnitine, producing trimethylamine (TMA). The liver then converts TMA into TMAO, which circulates in the blood.
Research over the last decade has revealed that elevated TMAO levels are tied to higher risks of heart attack, stroke, and kidney disease. Now, abdominal aortic aneurysms can be added to the list.
Dr. Stanley Hazen, senior author of the study and chair of Cleveland Clinic’s Cardiovascular and Metabolic Sciences Department, has been at the forefront of uncovering the gut microbiome’s surprising role in cardiovascular health. “What we eat doesn’t just feed us—it feeds our microbes,” Hazen noted. “And their byproducts, like TMAO, can directly influence the health of our blood vessels.”
Why Aneurysms Are So Dangerous
An abdominal aortic aneurysm begins quietly. Over time, the wall of the aorta weakens and bulges outward. Aging, smoking, high blood pressure, and genetics are well-known risk factors. The danger lies in rupture: as the aneurysm grows, the chances of it bursting rise sharply.
The condition kills thousands each year, often suddenly, because most patients never feel symptoms until it’s too late. Large aneurysms are typically repaired with either open surgery or endovascular procedures, where a stent graft is placed inside the artery. But these are major interventions. There has never been a widely available drug or lifestyle-based therapy proven to slow aneurysm growth—until now, the only strategy was “watchful waiting” until surgery was necessary.
That’s why the link between TMAO and aneurysm progression is so important. It opens the door to new ways of predicting who is at risk and potentially preventing aneurysms from worsening before surgery is needed.
Diet, Microbes, and the Future of Treatment
The Cleveland Clinic team’s findings raise an exciting possibility: what if targeting TMAO—through diet, medication, or microbiome-based therapies—could protect patients from aneurysms?
In animal studies, drugs that block the production of TMAO have been shown to reduce aneurysm formation and rupture. These therapies are not yet available for humans, but clinical trials could be on the horizon. Meanwhile, dietary choices may offer a practical way to lower TMAO levels. Plant-based diets, fish, and foods rich in fiber tend to produce less TMAO than diets heavy in red meat and eggs.
Dr. Hazen emphasized that this is not just about avoiding certain foods, but about rethinking the powerful connection between gut microbes, diet, and vascular health. “Our gut bacteria are part of the story of heart and vessel disease,” he said. “What this research shows is that their chemistry may directly contribute to life-threatening conditions like aneurysm.”
A Decade of Research Connecting TMAO to Disease
This discovery builds on more than ten years of work from Hazen’s team, which has repeatedly demonstrated how TMAO is linked to poor outcomes in cardiovascular health. Elevated TMAO has been tied to higher risks of heart attack, stroke, kidney disease, and now aneurysms. These findings have been confirmed by research groups worldwide, leading to the development of clinical TMAO testing.
Today, many hospitals and clinics already offer blood tests that measure TMAO as a marker of cardiovascular risk. If further studies confirm the aneurysm connection, doctors may soon be able to use TMAO testing not just to predict heart attacks, but also to identify patients at high risk for aneurysm growth.
Hope for the Future
Abdominal aortic aneurysms remain a devastating condition, claiming lives every year. But the Cleveland Clinic’s findings suggest a future where a simple blood test might identify patients at risk, and new therapies—whether medications or microbiome-based approaches—could slow aneurysm growth.
For now, the research offers patients and doctors a new lens through which to view the disease. It underscores the power of the gut microbiome, the influence of diet, and the promise of personalized medicine. Perhaps most importantly, it provides hope that one day, a condition long considered untreatable outside of surgery may finally have preventive solutions.
More information: Circulating Trimethylamine N-Oxide and Growth Rate of Abdominal Aortic Aneurysms and Surgical Risk, JAMA Cardiology (2025). DOI: 10.1001/jamacardio.2025.2698