Health is often described as the silent force that allows us to live fully, but for millions of people worldwide, this silence is disrupted by inherited conditions that leave an indelible mark on their lives. One such condition is thalassemia—a genetic blood disorder that touches not only the body but also the heart, the family, and entire communities.
For those who live with thalassemia, everyday life is shaped by fatigue, frequent hospital visits, and a constant need for medical care. Parents often discover the disorder in their child when anemia persists despite treatment. Behind every laboratory test and medical term lies a deeply human story of resilience, hope, and the pursuit of a normal life.
To understand thalassemia is to delve into science, but also into compassion. It is about unraveling the mysteries of hemoglobin, the protein that gives blood its life-sustaining power, and recognizing how small genetic changes can profoundly alter human existence. This article explores thalassemia in depth—its causes, symptoms, diagnosis, and treatment—through both a scientific lens and a human perspective.
What is Thalassemia?
Thalassemia is an inherited blood disorder characterized by the reduced or absent production of hemoglobin. Hemoglobin is the oxygen-carrying molecule found in red blood cells, and without it, oxygen cannot effectively reach tissues and organs.
In people with thalassemia, the genes responsible for producing hemoglobin are mutated, leading to a shortage of healthy red blood cells. This shortage causes anemia, which can range from mild to severe, depending on the type of thalassemia inherited.
The disorder is most prevalent in regions historically affected by malaria—such as South Asia, the Middle East, Africa, and the Mediterranean—because carrying one thalassemia gene provides partial protection against malaria. Over generations, this genetic trait became more common in these populations, even though inheriting two defective genes results in serious disease.
Hemoglobin and the Science of Blood
To appreciate thalassemia, one must first understand hemoglobin’s central role in life.
Hemoglobin is a complex protein inside red blood cells, made of four subunits: two alpha-globin chains and two beta-globin chains. These chains bind iron, allowing hemoglobin to capture oxygen in the lungs and deliver it to tissues.
In thalassemia, mutations in the genes responsible for alpha or beta chains disrupt this process. Without enough functional hemoglobin, red blood cells become fragile and break down faster than they should—a process called hemolysis. This leads to chronic anemia, forcing the body to compensate in ways that can damage organs, bones, and overall growth.
Types of Thalassemia
Thalassemia is classified based on which part of the hemoglobin chain is affected:
Alpha Thalassemia
- Caused by mutations in the genes responsible for alpha-globin production.
- Each person has four alpha-globin genes (two from each parent). The severity depends on how many are defective:
- Silent carrier (1 gene defect): No symptoms, normal life.
- Alpha-thalassemia trait (2 gene defects): Mild anemia, often mistaken for iron deficiency.
- Hemoglobin H disease (3 gene defects): Moderate to severe anemia, enlargement of spleen, bone deformities.
- Alpha-thalassemia major (4 gene defects): Also known as hydrops fetalis, usually fatal before or shortly after birth.
Beta Thalassemia
- Caused by mutations in the beta-globin gene. Each person has two beta-globin genes.
- Beta-thalassemia minor (1 gene defect): Mild anemia, usually no serious health issues.
- Beta-thalassemia intermedia (2 defective genes with partial function): Moderate anemia, may not always require transfusions.
- Beta-thalassemia major (2 nonfunctional genes): Also called Cooley’s anemia, it is the most severe form. Symptoms appear within the first two years of life, requiring lifelong treatment.
Causes of Thalassemia: The Genetic Code Written in Blood
The root cause of thalassemia is mutation in the globin genes. These mutations can be deletions, insertions, or point mutations that disrupt the normal production of hemoglobin chains.
Thalassemia is an autosomal recessive disorder. This means that for a child to develop the severe form, they must inherit a defective gene from both parents. If only one gene is defective, the child becomes a carrier, often with mild or no symptoms.
For couples in regions where thalassemia is common, genetic counseling is crucial. Two carriers have a 25% chance of having a child with severe thalassemia, a 50% chance of passing on carrier status, and a 25% chance of having a healthy, unaffected child.
Symptoms of Thalassemia
Thalassemia symptoms depend on the type and severity. In mild forms, individuals may live without realizing they have the disorder. In severe forms, symptoms can be life-threatening.
Common Symptoms
- Fatigue and weakness due to low oxygen supply.
- Pale or yellowish skin caused by anemia and increased breakdown of red blood cells.
- Delayed growth and development in children.
- Bone deformities, especially in the face and skull, due to the bone marrow working overtime to produce red blood cells.
- Enlarged spleen and liver as these organs attempt to filter defective cells.
- Dark urine from excess hemoglobin breakdown.
Severe Symptoms (Thalassemia Major)
- Severe anemia appearing in the first two years of life.
- Failure to thrive and frequent infections.
- Heart problems due to chronic low oxygen and iron overload.
- Shortness of breath and dizziness.
These symptoms not only affect physical health but also emotional well-being, as children and adults with thalassemia often face limitations in daily life and constant medical interventions.
Diagnosis of Thalassemia
Early diagnosis is critical, both for treatment and for preventing complications.
Physical Examination
Doctors often begin with a physical exam, looking for signs of anemia, enlarged spleen, or bone deformities.
Blood Tests
- Complete blood count (CBC): Reveals low hemoglobin and small red blood cells (microcytosis).
- Peripheral blood smear: Shows abnormally shaped red cells.
- Iron studies: Help distinguish thalassemia from iron-deficiency anemia.
Specialized Tests
- Hemoglobin electrophoresis: Identifies abnormal types of hemoglobin, such as HbF (fetal hemoglobin) or HbA2, which are elevated in thalassemia.
- DNA analysis: Detects specific gene mutations responsible for thalassemia.
Prenatal Testing
For couples at risk, prenatal tests such as chorionic villus sampling or amniocentesis can determine whether a fetus has thalassemia.
Treatment of Thalassemia
Treatment depends on the severity of the condition. While mild cases may not need therapy, severe thalassemia requires lifelong medical care.
Blood Transfusions
The cornerstone of treatment for thalassemia major is regular blood transfusions—often every 2–4 weeks. Transfusions supply healthy red blood cells, correcting anemia and allowing normal growth and development.
However, repeated transfusions lead to iron overload, a dangerous buildup of iron in the body that can damage the heart, liver, and endocrine organs.
Iron Chelation Therapy
To manage iron overload, patients require chelation therapy—medications such as deferoxamine, deferasirox, or deferiprone. These drugs bind excess iron and help the body eliminate it. Without chelation, iron overload is fatal.
Bone Marrow or Stem Cell Transplantation
The only known cure for thalassemia is a bone marrow or stem cell transplant, which replaces defective bone marrow with healthy donor cells. This treatment works best in young patients with a compatible donor but is not available to everyone due to cost and risks.
Emerging Therapies
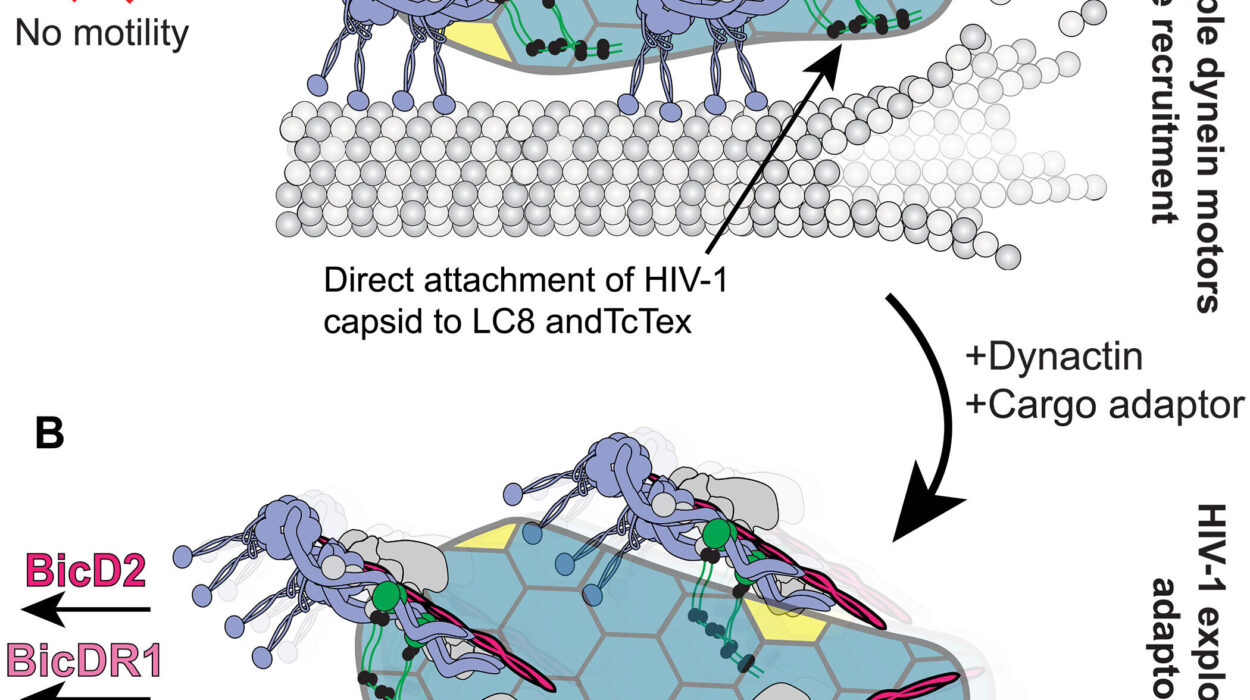
- Gene therapy: Scientists are exploring ways to correct or replace the defective globin genes. Some early trials have shown promise.
- CRISPR gene editing: A revolutionary technology that could potentially “repair” mutations at the DNA level.
- Drugs boosting fetal hemoglobin (HbF): Since HbF does not require beta chains, stimulating its production may reduce symptoms.
Supportive Care
- Folic acid supplements support red blood cell production.
- Vaccinations and antibiotics protect against infections, especially in patients with spleen issues.
- Lifestyle management—balanced nutrition, regular checkups, and avoiding infections—is critical to long-term health.
Living with Thalassemia
Beyond the science and treatment, thalassemia is a lifelong journey. Children often face disrupted schooling due to hospital visits. Adults may struggle with fatigue or social stigma. Families cope with emotional stress, financial strain, and the burden of constant care.
Yet, many patients live fulfilling lives thanks to advances in treatment. Support groups and awareness campaigns help reduce stigma and provide emotional strength. Education, empowerment, and access to healthcare are vital in transforming thalassemia from a life-limiting condition to a manageable one.
Prevention: Breaking the Cycle
Since thalassemia is inherited, prevention lies in awareness and genetic counseling. In many countries, screening programs identify carriers before marriage or childbirth. By knowing their genetic status, couples can make informed choices about family planning.
Public health initiatives that promote premarital screening have successfully reduced new cases in countries like Cyprus, Iran, and Thailand. This highlights that prevention is not only possible but achievable through community awareness and policy action.
The Global Burden of Thalassemia
Thalassemia is most common in regions spanning from the Mediterranean to Southeast Asia, with high prevalence in India, Bangladesh, Pakistan, the Middle East, and parts of Africa. Global migration has spread the disorder to Western countries as well.
According to estimates, about 300,000–400,000 babies are born each year with severe hemoglobin disorders, including thalassemia. While developed nations offer advanced treatments, many children in low-income countries lack access to transfusions and chelation therapy, leading to early deaths.
This inequality underscores the need for international collaboration, affordable treatments, and expanded access to cures.
Hope for the Future
The story of thalassemia is not just one of struggle, but also of progress. Where once children with severe thalassemia rarely survived beyond early childhood, many now live into adulthood, study, work, and start families.
With ongoing research into gene therapy, stem cell transplantation, and new medications, the future looks brighter than ever. What was once considered a fatal genetic fate is slowly becoming a manageable, even curable, condition.
Conclusion: Science, Compassion, and the Human Spirit
Thalassemia is more than a genetic mutation—it is a human experience shaped by biology, culture, society, and medicine. It reminds us of the fragility of life, but also of resilience. Behind every scientific discovery and medical advance are the faces of children hoping to play freely, parents longing for their child’s health, and communities striving for awareness and prevention.
Understanding thalassemia means embracing both science and humanity. It is about decoding the genetic script of hemoglobin, but also about listening to the stories of those who live with it. The journey toward a world without thalassemia is still ongoing, but with knowledge, compassion, and innovation, it is a future within reach.