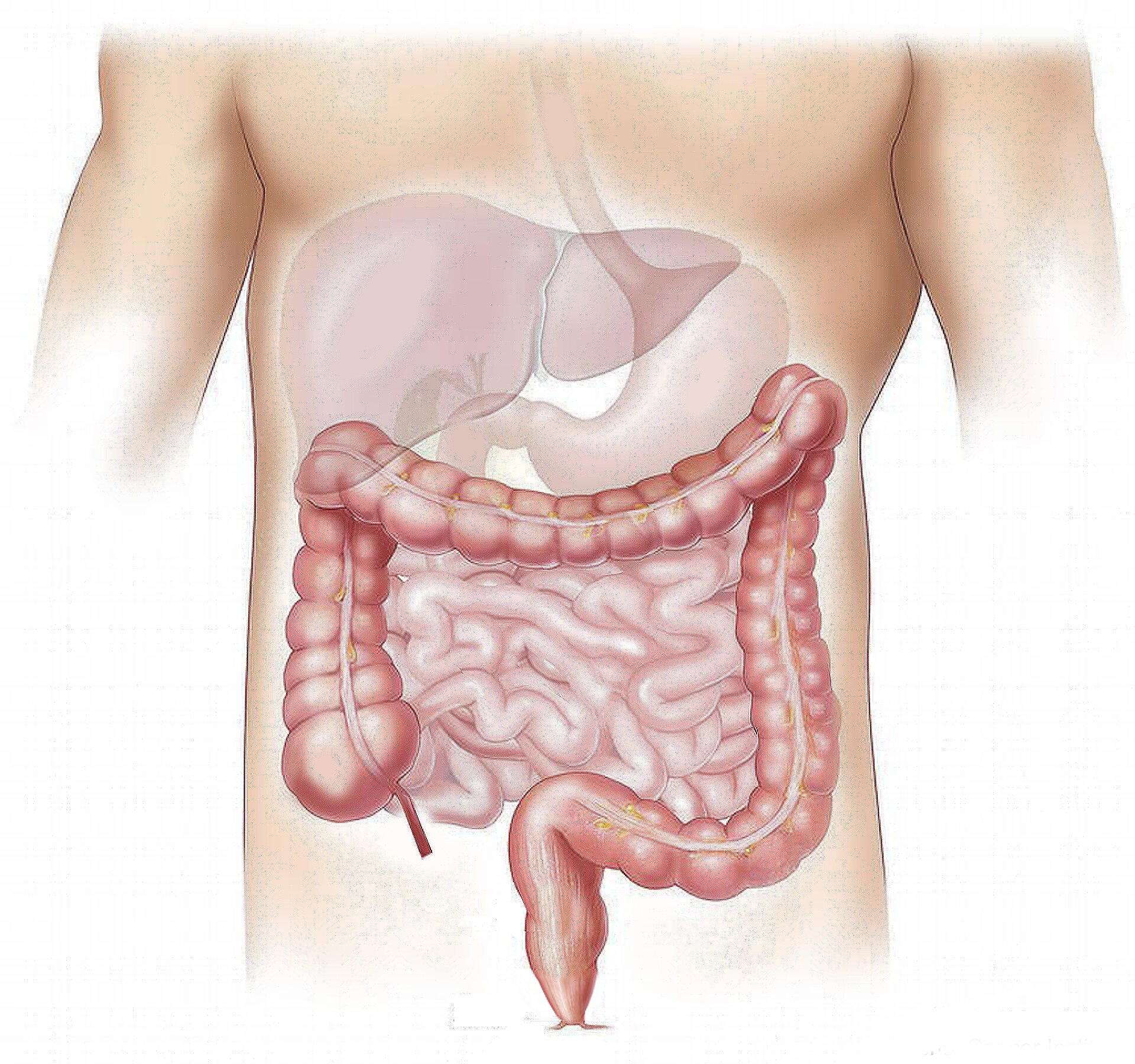
For decades, turning 50 came with a new health milestone: the dreaded yet potentially lifesaving colorectal cancer screening. But rising cancer rates among younger adults have disrupted that tradition, forcing a new question to the forefront of public health policy: should screening start earlier?
In 2021, the U.S. Preventive Services Task Force decided the answer was yes. It formally lowered the recommended age to begin routine colorectal cancer screening from 50 to 45, a move driven by mounting data showing increased cancer rates among people under 50. Now, a new study from Kaiser Permanente Northern California has added robust, real-world data to this discussion—and the results might just change how we approach early cancer detection altogether.
The Silent Threat Growing Louder
Colorectal cancer, once seen as a disease of the aging, has been steadily creeping into younger demographics. Over the past few decades, incidence rates among adults in their 40s have been climbing in the United States, even as overall rates in older populations have declined thanks to improved screening and awareness.
This reversal has left experts scrambling for answers. Is it lifestyle? Environment? Genetics? Likely, it’s a mix of all three. But regardless of the cause, one message has become clear: waiting until 50 to start screening may simply be too late for some.
This is where the Kaiser Permanente study steps in—not just as a data point, but as a possible game-changer in the way healthcare systems validate, refine, and implement life-saving guidelines.
A Closer Look at the Study
Published in JAMA under the title “Screening Colonoscopy Yields Among Adults Aged 45 to 49 Years After Lowering the Colon Cancer Screening Age,” the study isn’t just a dry academic exercise. It’s a carefully designed exploration into whether screening 45-year-olds is truly as effective—and necessary—as it is for those who traditionally began screening at 50.
To find answers, researchers followed a large cohort of 12,031 adults between the ages of 45 and 54 who underwent their very first screening colonoscopy between 2021 and 2024. All participants were part of Kaiser Permanente Northern California’s integrated health system, which ensured that their medical records were complete and their health histories closely monitored.
Importantly, the researchers excluded individuals with any prior history of colorectal disease, incomplete procedures, or those undergoing colonoscopy for diagnostic rather than screening purposes. The goal was to isolate the effectiveness of colonoscopy as a pure screening tool in this younger age group.
The study compared two age bands: those aged 45 to 49, and those aged 50 to 54. The question was simple—are younger adults showing enough early signs of colorectal neoplasia to justify their inclusion in standard screening protocols?
What They Found: Numbers That Speak Volumes
Among the younger group—those aged 45 to 49—any adenoma, a benign but potentially precancerous tumor, was detected in 35.4% of patients. For the older 50 to 54 group, the detection rate was 40.8%. Statistically, this is a modest but significant difference, with an adjusted risk ratio (aRR) of 0.86.
At first glance, that might seem like a reason to pause. Shouldn’t we be more concerned if the detection rate is lower? But when researchers looked deeper—particularly at more clinically concerning findings—the age gap all but disappeared.
Advanced adenomas, which are larger and have a higher potential to turn malignant, occurred in 3.8% of younger patients and 4.1% of older patients. That difference wasn’t statistically significant. Even more striking was the detection of actual colorectal cancer, which was rare in both groups—just 0.1%. Sessile serrated lesions and advanced serrated lesions, other high-risk precursors, also showed nearly identical rates across age groups.
What this means in plain language is that while slightly fewer benign growths were found in the younger age group, the rate of detecting serious or potentially cancerous lesions was almost exactly the same. In other words, 45-year-olds are already showing meaningful levels of disease. Waiting five more years to screen them could mean missing the critical window when intervention is most effective.
Why It Matters: More Than Just a Policy Check
In the world of medicine, changing a national guideline is no small feat. It requires a mountain of evidence, expert consensus, and often, a delicate balancing act between clinical benefit and cost-effectiveness. When the screening age was lowered to 45, many in the healthcare community welcomed the decision, but some remained cautious. Would the younger population yield enough results to justify such a shift? Would we be stretching already limited resources too thin?
This study offers clear, data-backed reassurance: not only is earlier screening justifiable—it’s essential.
Moreover, the study addressed a critical secondary concern: should we adjust detection benchmarks when screening younger people? The answer, according to the data, is no. Adenoma detection rates (ADRs) and serrated lesion detection rates (SDRs), important quality metrics for colonoscopy, don’t require recalibration based on age. Physicians can—and should—apply the same expectations for finding abnormalities in 45-year-olds as they do in those slightly older.
The Human Side of the Numbers
Behind the statistics lie stories. Stories of people who might have delayed their first colonoscopy until they were 50—only to discover cancer that could have been caught five years earlier. Stories of families spared the pain of late-stage diagnosis because a loved one got screened at 45. These are the invisible victories embedded in the data.
Take for example, a healthy 46-year-old with no family history or symptoms who goes in for a routine colonoscopy and learns that an advanced adenoma has been removed just in time. Without early screening, that lesion could have silently progressed for years. That’s not just prevention—that’s life-saving medicine in action.
The Road Ahead
Healthcare systems across the U.S. are still adapting to the updated screening guidelines. One of the biggest challenges is increasing public awareness, especially among younger adults who may not perceive themselves at risk. Unlike mammograms or blood pressure checks, colonoscopy still suffers from stigma, fear, and avoidance.
But as more studies like this surface, and as more lives are quietly saved through earlier detection, the hope is that the cultural conversation will shift. Just as we normalized getting vaccinated, wearing seat belts, and applying sunscreen, the next step may be to normalize cancer screening at 45.
Physicians will need to play a critical role, encouraging their patients to take the plunge sooner rather than later. Health systems, too, must ensure access, affordability, and culturally competent care to make early screening not just possible but routine.
Science as a Living Discipline
What this study truly highlights is that science is not static. It’s a living, breathing discipline—constantly evolving, constantly responding to new data. The decision to begin screening at 45 wasn’t just a bureaucratic maneuver; it was the result of sustained vigilance, research, and a commitment to saving lives.
With over 12,000 patients’ data backing the new guideline, the results are no longer hypothetical. They’re measurable, impactful, and most importantly, actionable.
The Bottom Line
Colorectal cancer doesn’t wait until you’re 50. It doesn’t care whether you’re young, fit, or asymptomatic. This new study from Kaiser Permanente Northern California underscores a growing truth in modern medicine: earlier screening isn’t just acceptable—it’s necessary.
For individuals between 45 and 49, the findings are a call to action. For doctors and policymakers, they’re a validation of a bold shift in cancer prevention. And for the wider world of science, they’re a reminder that listening to the data—even when it challenges tradition—can lead to better outcomes for everyone.
So if you’re approaching your mid-40s and haven’t yet considered colorectal screening, now’s the time. Not because a study says so—but because the life you save could be your own.
Reference: Jeffrey K. Lee et al, Screening Colonoscopy Yields Among Adults Aged 45 to 49 Years After Lowering the Colon Cancer Screening Age, JAMA (2025). DOI: 10.1001/jama.2025.7494