You accidentally bite the inside of your cheek while chewing. It hurts, stings for a moment, and then, astonishingly, it vanishes. Within a day or two, the wound is gone, leaving no scar, no trace—just smooth tissue, perfectly repaired.
This everyday miracle has long baffled scientists. Why does the mouth heal so fast, while a scraped knee or a surgical incision can take weeks and often leaves a permanent scar?
Now, a breakthrough study published in Science Translational Medicine offers an answer. A team of researchers from Cedars-Sinai, Stanford Medicine, and the University of California, San Francisco (UCSF), have uncovered a biological pathway that makes oral tissues heal faster and without scarring—and they believe this discovery could revolutionize how we treat skin wounds.
Why the Mouth Holds the Healing Key
“Our research began with two simple but profound questions,” said Dr. Ophir Klein, executive vice dean of Children’s Health at Cedars-Sinai and co-leader of the study. “Why does your mouth heal better than your skin? And if we can figure that out, can we use that knowledge to help the rest of the body heal in the same way?”
Unlike the outer layers of skin, the tissue inside the mouth—known as the oral mucosa—can regenerate rapidly. A small cut or bite typically heals within 24 to 72 hours, often without even leaving a mark. Meanwhile, similar skin injuries can take up to a week or longer, and they often end with scars.
That contrast intrigued the researchers, prompting a deeper investigation into the molecular machinery behind it.
Mice, Molecules, and a Clue in the Code
To solve the mystery, scientists turned to laboratory mice, analyzing samples from two parts of their bodies: the facial skin and the lining of their mouths. Under the microscope, the difference wasn’t just visible—it was molecular.
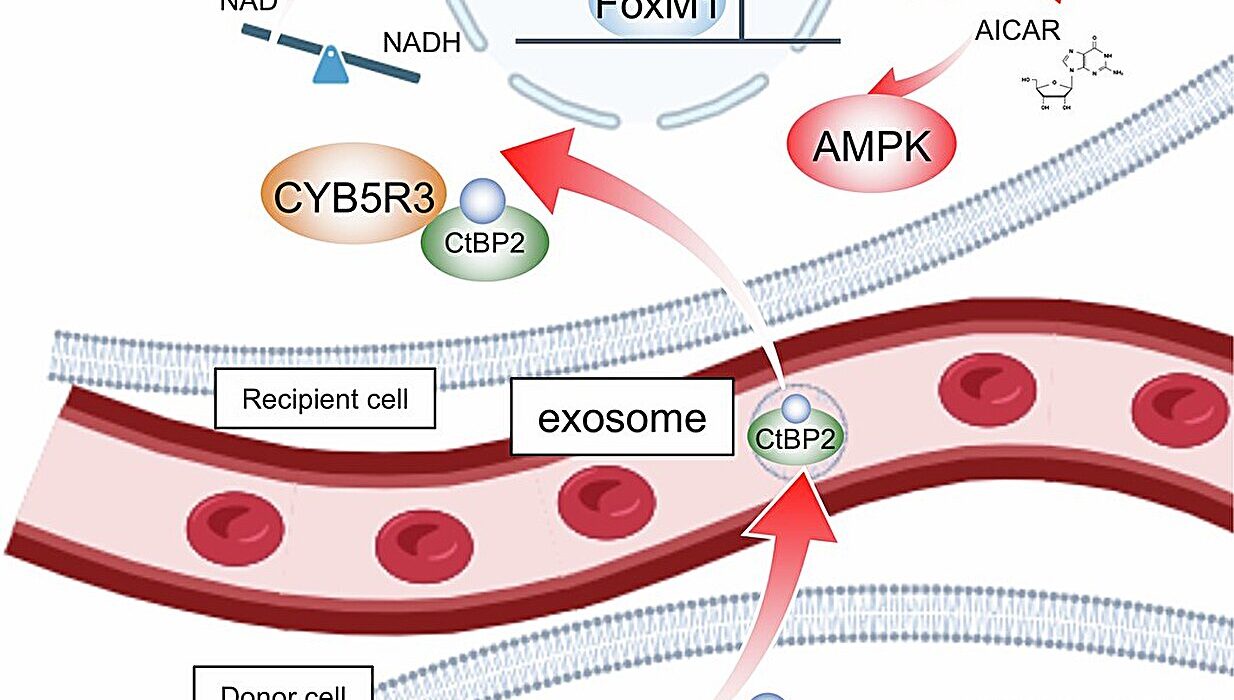
They discovered a specific communication system, or signaling pathway, at work in the mouth tissue. At the center of this system is a protein called GAS6 and an enzyme called AXL. These two interact in a way that effectively silences another signaling system known as FAK, which is notorious for promoting inflammation and fibrosis—a fancy term for scarring.
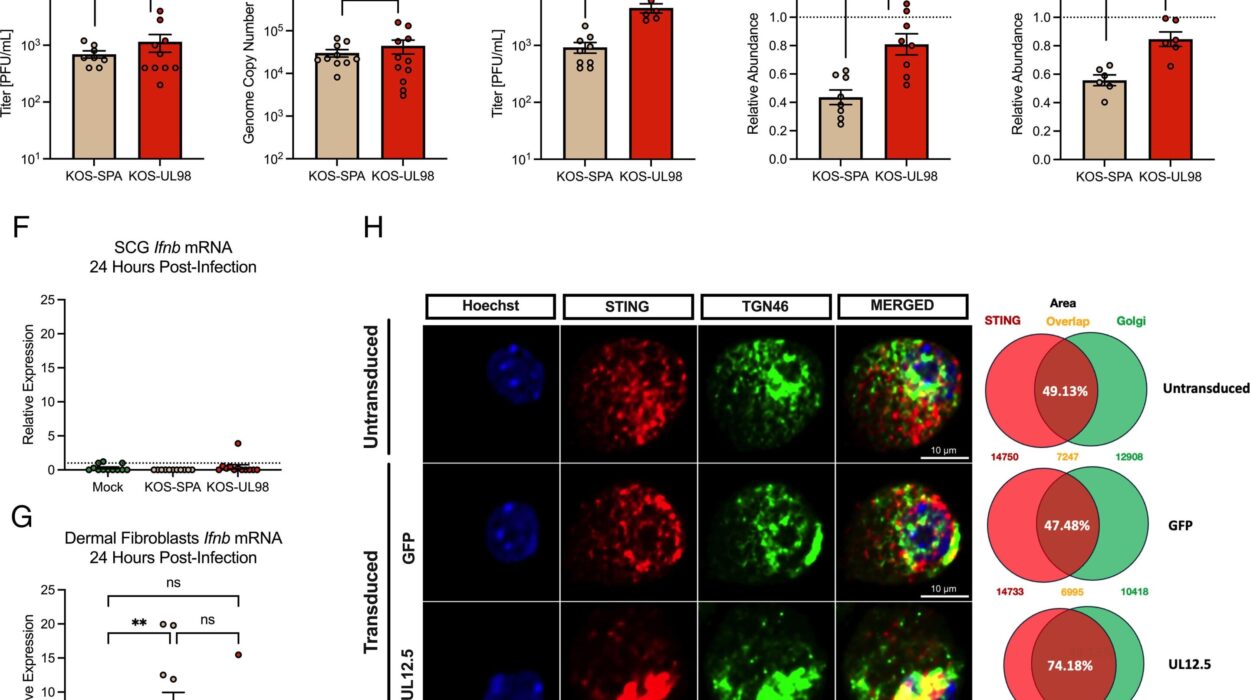
When AXL is active, the FAK pathway is suppressed, and the tissue heals cleanly, without scar tissue. But if AXL is inhibited, the healing in the mouth slows down and starts to resemble the slower, scar-prone process of the skin.
To test this, the team blocked AXL in the oral tissue of mice. The results were dramatic: healing slowed and scars appeared. Conversely, when they stimulated AXL in skin wounds, something extraordinary happened—those wounds began to heal more like oral wounds, faster and with fewer signs of scarring.
“This data shows that the GAS6-AXL pathway is potentially important for scarless healing in the mouth,” said Dr. Klein, “and that manipulating it may help reduce skin scars as well.”
The Science of Scar-Free Healing
Scarring is a natural part of the body’s healing process. When skin is injured, a cascade of chemical signals rushes to the scene, summoning cells that close the wound, kill off invaders, and begin to rebuild tissue. But that repair job is messy—it often results in tough, fibrous tissue that doesn’t quite match the original skin.
In the mouth, however, the body uses a different playbook. The GAS6-AXL pathway seems to orchestrate a more precise, efficient healing strategy—one that repairs without overreacting.
“Unfortunately, current treatments do not adequately prevent scarring because we don’t fully understand the mechanisms that control it,” Klein added. “Our research helps fill that gap.”
Understanding how this scarless repair works in the mouth opens the door to replicating it elsewhere. It’s not just a curiosity—it could be a roadmap to better healing for burn victims, surgery patients, and anyone suffering from chronic wounds or disfiguring injuries.
From Mice to Medicine: What’s Next?
The implications of the study are exciting—but there’s still a journey ahead before this healing insight becomes a clinical treatment.
“This is a preclinical study,” explained Dr. Michael Longaker, co-author of the study and the Dean P. and Louise Mitchell Professor at Stanford University. “The next steps are to determine how this applies to human tissue and to begin developing therapies that can enhance skin healing based on this pathway.”
This means conducting further clinical trials and testing potential medications or treatments that can safely activate the GAS6-AXL pathway in humans. If successful, such therapies could transform wound care, plastic surgery, and dermatology—perhaps even helping soldiers, trauma victims, or surgical patients heal with little or no visible trace.
“Further clinical studies should be performed to assess the nature of the relationship between AXL and scarring in humans,” Longaker emphasized.
A Future Without Scars?
The dream of scarless healing has been with humanity for centuries, hinted at in myth and medicine alike. From the regenerative powers of salamanders to science-fiction visions of instant repair, the idea that the body could heal perfectly has always fascinated us.
Now, we may be one step closer to that future—and the key may have been hiding inside our mouths all along.
With deeper understanding of the GAS6-AXL pathway, researchers are not just unraveling the secrets of how we heal—they’re offering hope for millions of people worldwide who live with the physical and emotional scars of injury and surgery.
And so, the next time you accidentally bite your cheek, take a moment to marvel—not just at how fast it disappears, but at the quiet, complex biological symphony that just might hold the key to healing the rest of your body too.
Reference: Michelle Griffin et al, Growth arrest specific-6 and angiotoxin receptor-like signaling drives oral regenerative wound repair, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.adk2101. www.science.org/doi/10.1126/scitranslmed.adk2101