Fungal infections are often dismissed as minor nuisances—itchy skin rashes, athlete’s foot, yeast infections. But beneath that irritating surface lies a far more ominous truth: fungi can kill. Every year, more than one billion people worldwide suffer from fungal infections, and for millions, the consequences are not just uncomfortable—they’re deadly. Some fungi cause invasive infections in the lungs and brain, with mortality rates that rival or exceed those of many cancers. Yet despite the global scale of the problem, the arsenal of antifungal drugs remains woefully understocked.
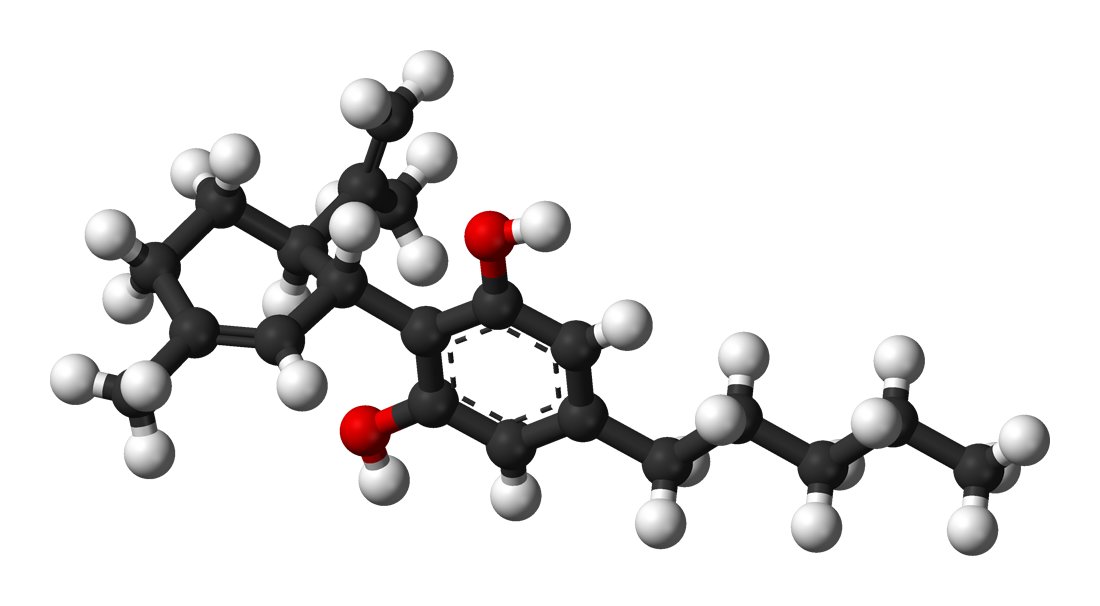
Now, a surprising new player is stepping onto the fungal battlefield: cannabis. In a groundbreaking study published in PLOS Neglected Tropical Diseases, researchers at Macquarie University have discovered that two cannabis-derived compounds—cannabidiol (CBD) and cannabidivarin (CBDV)—have potent antifungal properties. In laboratory tests, these cannabinoids not only wiped out the dangerous Cryptococcus neoformans, a pathogen that causes deadly brain infections, but they also eradicated common skin-infecting fungi more rapidly than conventional treatments.
These findings could usher in an entirely new class of antifungal agents—and they couldn’t come at a better time.
A Quiet Epidemic: The Global Threat of Fungal Pathogens
While bacteria and viruses dominate headlines, fungi quietly wreak havoc on global health. Fungal pathogens like Candida, Aspergillus, and Cryptococcus cause an estimated 1.5 million deaths per year. Many of these fungi are opportunistic, preying on people with weakened immune systems—from chemotherapy patients to those with HIV/AIDS. And as global warming and human encroachment change ecosystems, fungal diseases are becoming more aggressive, more resistant to treatment, and more widespread.
Compounding the problem is the lack of effective medications. Only a handful of antifungal drug classes exist, and their use is often limited by toxicity, drug interactions, and growing resistance. Developing new drugs is notoriously slow, taking 10 to 15 years on average—time we don’t have as fungal resistance spreads.
That’s why Macquarie University researcher Dr. Hue Dinh, a postdoctoral fellow in the School of Natural Science, took a different approach. Instead of starting from scratch, she and her colleagues looked to compounds already approved for use in humans. And that’s where cannabis came in.
Turning Over a New Leaf in Antimicrobial Research
When people hear the word cannabis, they might think of relaxation, pain relief, or the high from THC. But the cannabis plant is a pharmacological treasure chest, containing over 500 natural compounds, many of which are biologically active. While THC and CBD dominate headlines, lesser-known cannabinoids like CBDV are beginning to reveal their own medicinal potential.
Dr. Dinh teamed up with Associate Professor Amy Cain, a specialist in microbial resistance, and Professor Mark Connor, a pharmacologist at Macquarie Medical School with deep experience in cannabinoid biology. Their goal was bold: investigate whether any of these cannabis-derived compounds could kill some of the world’s most troubling fungal pathogens.
One target stood out immediately: Cryptococcus neoformans, a fungus that can infiltrate the lungs and brain, often triggering cryptococcal meningitis. This disease disproportionately affects people in developing countries and those with compromised immune systems, including HIV-positive individuals. Without rapid and effective treatment, the mortality rate soars.
But the available drugs for Cryptococcus infections—amphotericin B, flucytosine, and fluconazole—come with heavy side effects and increasing resistance. What if cannabinoids, with their relatively safe profile in humans, could offer a new weapon?
Breaking the Mold: Cannabinoids vs. Fungi
The team screened a wide array of cannabis-derived molecules. Among the top contenders were CBD, a non-intoxicating cannabinoid already used in epilepsy treatment, and CBDV, its molecular cousin, which has shown promise in autism and seizure research. The researchers exposed Cryptococcus neoformans cultures to both compounds—and the results were stunning.
“They worked faster than our current antifungal drugs,” says Dr. Dinh. “We weren’t expecting such strong activity. They not only halted fungal growth but killed the pathogens outright.”
The effectiveness didn’t stop with Cryptococcus. The cannabinoids were tested against 33 additional fungal strains, spanning clinical, veterinary, and environmental origins. The results showed that both CBD and CBDV had broad-spectrum activity, eliminating Cryptococcus species as well as dermatophytes—the fungi behind athlete’s foot, ringworm, and other common skin infections.
The findings suggest that cannabinoids don’t just suppress fungal growth; they destroy the fungal cells—a crucial difference that could translate into shorter treatment times and fewer relapses.
An Unlikely Ally: The Wax Moth Larva
Lab tests in petri dishes are one thing, but to truly explore medical potential, researchers need a living model. Enter Galleria mellonella—the wax moth larva.
This squirmy little insect has become a rising star in biomedical research. Its immune system shares surprising similarities with that of mammals, and it offers an ethically sound, cost-effective way to test the toxicity and efficacy of new drugs before moving into mammalian trials.
Using Macquarie’s specialized Galleria Research Facility, the team infected the larvae with fungal pathogens and then treated them with the cannabis compounds. The larvae survived. Not only that, the cannabinoids demonstrated real antifungal action in vivo—a crucial step forward in bringing lab results closer to human application.
The compounds showed low toxicity and good tolerability in the larvae, further supporting their promise as therapeutic agents.
A Topical Revolution on the Horizon
While the idea of injecting cannabis compounds into the bloodstream to treat fungal meningitis sounds tantalizing, the practical hurdles remain high. Cannabinoids are notoriously difficult to dissolve, particularly for intravenous use. Their lipophilic nature makes formulation tricky, especially when trying to target the central nervous system or deep lung tissues.
But Dr. Dinh sees a more immediate application: topical antifungal treatments. The cannabinoids’ rapid action against skin pathogens and their known safety profile in humans make them ideal candidates for creams, lotions, and gels. “If we can demonstrate that these ones work well for common infections, you could actually just get some CBD oil and then rub it on your skin to treat it,” she explains.
This could be a game-changer for millions suffering from chronic or recurrent fungal skin infections, especially in regions where access to prescription antifungals is limited.
Perhaps even more exciting, preliminary data suggest that fungi are less likely to develop resistance to cannabinoids compared to conventional drugs. This resistance-stability may stem from the unique way cannabinoids disrupt cell membranes or interfere with fungal metabolism—mechanisms that pathogens find harder to adapt to over time.
From Plant to Pharmacy: What Comes Next
Dr. Dinh and Associate Professor Cain are already working with commercial partners to translate these lab discoveries into practical products. The goal is to develop over-the-counter treatments using CBD and CBDV to tackle skin fungal infections safely and effectively.
The researchers are also expanding their studies to examine how cannabinoids could be combined with existing antifungal agents, potentially lowering the required dosages and reducing side effects. Hybrid therapies may offer a powerful one-two punch: cannabinoids to kill the fungi, and existing drugs to mop up any lingering cells.
Still, the path to clinical use is complex. Even with an existing safety record, topical formulations require stability testing, absorption studies, and possibly human trials to gain regulatory approval. And while CBD is already widely available in many countries, CBDV remains less studied and more tightly regulated.
Nevertheless, the groundwork laid by this Macquarie-led team offers a hopeful blueprint: take known compounds, test them in new ways, and open doors to unexpected treatments.
Cannabis and the Future of Infectious Disease
This research comes amid a broader renaissance in cannabinoid science. Beyond pain management and neurological conditions, researchers are now looking at cannabis compounds for antibacterial, antiviral, and now antifungal purposes. The cannabis plant, long vilified and misunderstood, is revealing a pharmacological profile as diverse and rich as any rainforest.
In this context, Dr. Dinh’s work is part of a larger shift: an acknowledgment that our next medical breakthroughs may not come from synthetic compounds or high-tech engineering, but from the molecules nature has already provided—molecules hidden in plain sight.
As fungal infections continue to rise, and as resistance erodes the efficacy of existing drugs, the world desperately needs alternatives. And perhaps, in the resinous leaves of Cannabis sativa, we’ve found one.
Conclusion: The Green Frontier in Medical Mycology
The idea that cannabis compounds could help treat life-threatening fungal infections might once have sounded like science fiction—or wishful thinking. But the rigorous research emerging from Macquarie University has transformed that notion into scientific possibility.
With CBD and CBDV showing strong efficacy in both lab dishes and living organisms, the future of antifungal therapy may well be greener than we imagined. Though challenges remain—particularly for systemic infections—the promise of topical cannabinoid-based treatments is closer than ever.
In the end, this story is not just about cannabis. It’s about reimagining what’s possible in medicine. It’s about asking new questions, testing old ideas in new ways, and daring to believe that some of the most powerful weapons in the fight against disease might already be growing in the ground beneath our feet.
Reference: Uncovering the antifungal potential of Cannabidiol and Cannabidivarin, PLOS Neglected Tropical Diseases (2025). DOI: 10.1371/journal.pntd.0013081. journals.plos.org/plosntds/art … journal.pntd.0013081