The human heart is no larger than a clenched fist, yet it beats with a thunderous importance that defines life itself. It pulses more than 100,000 times each day, pushing blood—our life’s currency—through 60,000 miles of arteries, veins, and capillaries. Each contraction is a whisper of life; each beat a promise of survival.
But what happens when this engine begins to fail—not suddenly, but gradually, silently, over decades? That’s the story of heart disease, the world’s leading cause of death. It doesn’t announce itself with drama at first. It sneaks in like a thief, unnoticed until the chest tightens or the breath shortens.
This is a story not just of biology, but of lifestyle, behavior, and choices—of science and humanity. It is the story of how heart disease develops—and, just as crucially, how it can be prevented.
The Anatomy of a Threat: What is Heart Disease?
“Heart disease” isn’t one illness—it’s a family of related conditions, all targeting the cardiovascular system. The most common type is coronary artery disease (CAD), which involves the narrowing or blockage of the coronary arteries, the blood vessels that supply the heart muscle with oxygen-rich blood. Other types include:
- Heart failure – when the heart cannot pump blood efficiently.
- Arrhythmias – irregular heartbeats that disrupt normal rhythms.
- Valvular heart disease – damage to one or more of the heart’s valves.
- Congenital heart defects – structural issues present at birth.
- Cardiomyopathy – disease of the heart muscle itself.
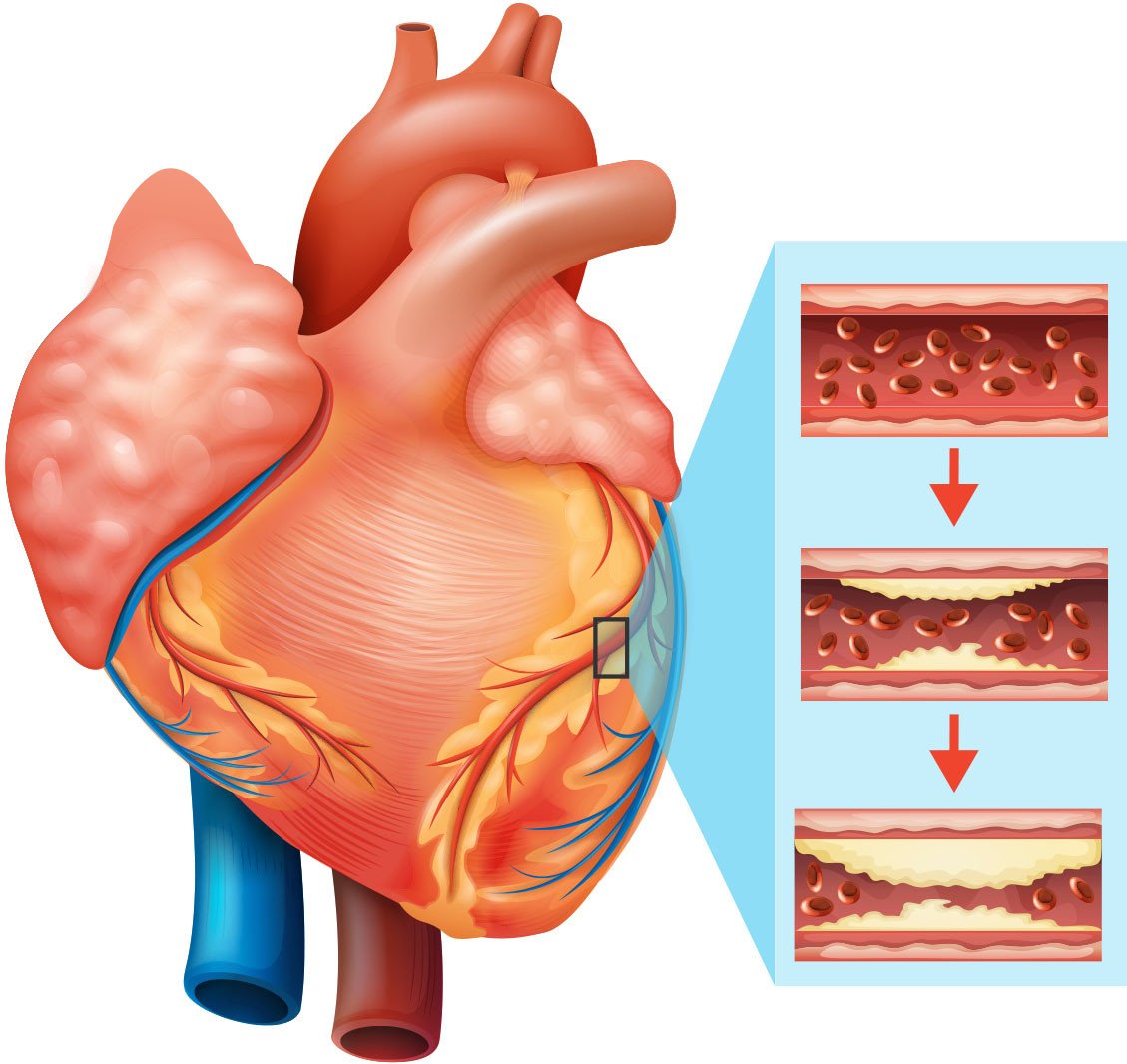
But for most people, when we talk about “heart disease,” we’re referring to atherosclerosis—the buildup of plaque inside the arteries. This is the slow-motion disaster that drives most heart attacks and strokes. And this is where our exploration begins.
The Beginning: How Heart Disease Starts
Heart disease doesn’t erupt in a single moment. It begins with damage to the endothelium, the delicate inner lining of blood vessels. This damage can be caused by a variety of factors:
- High blood pressure, which creates turbulence in the arteries.
- Smoking, which fills the blood with toxic chemicals.
- High levels of LDL (“bad”) cholesterol, which invades the damaged vessel walls.
- High blood sugar, which is corrosive over time.
Once the endothelium is compromised, the body reacts with inflammation. White blood cells rush in, cholesterol deposits accumulate, and over time, a plaque begins to form—composed of fat, cholesterol, calcium, and cellular debris.
This plaque doesn’t just sit there. It can grow, harden, and calcify, reducing blood flow like a clogged pipe. Worse, it can rupture, triggering the formation of a blood clot that completely blocks the artery. When that happens in the heart, it’s called a heart attack. In the brain, it’s a stroke.
The tragedy is not just in the event—it’s in how quietly the danger builds.
Risk Factors: The Fuel That Feeds the Fire
Why does this happen to some people and not others? The answer lies in risk factors, both controllable and uncontrollable.
Uncontrollable risk factors include:
- Age – Risk increases with age.
- Genetics – A family history of heart disease raises your own risk.
- Gender – Men tend to develop heart disease earlier, though women catch up after menopause.
Controllable risk factors are where the fight is truly won or lost:
- High blood pressure – Damages arteries and accelerates plaque formation.
- High LDL cholesterol – A primary ingredient of plaque.
- Low HDL cholesterol – HDL helps remove bad cholesterol from the bloodstream.
- Smoking – Causes inflammation and vascular damage.
- Poor diet – High in saturated fats, trans fats, and sugar.
- Physical inactivity – Contributes to obesity and metabolic problems.
- Obesity – Linked to all other risk factors.
- Diabetes – High blood sugar damages arteries and increases clot risk.
- Chronic stress – Triggers hormonal changes that affect blood pressure and inflammation.
These risk factors don’t act alone. They conspire. A sedentary lifestyle can lead to obesity, which increases blood pressure, which damages arteries—and so the cascade begins.
The Turning Point: When Symptoms Appear
For years—even decades—heart disease can grow unnoticed. But eventually, the body begins to whisper its distress:
- Chest pain or discomfort (angina), especially during exertion.
- Shortness of breath, often mistaken for aging or deconditioning.
- Fatigue, particularly after physical activity.
- Heart palpitations, where the beat feels off or irregular.
- Swelling in legs and ankles, a sign of poor circulation.
Sometimes, the first symptom is the worst one—a heart attack.
Women often experience different or subtler symptoms: nausea, jaw pain, back pain, lightheadedness. Because these are harder to recognize, women are more likely to ignore early signs.
The earlier symptoms are recognized, the better the outcome. But catching heart disease early depends not just on awareness—but on prevention.
The Ticking Clock: Why Prevention Matters
Heart disease isn’t inevitable. In fact, most forms of it are preventable. That’s not just a theory—it’s a proven reality. Studies from the American Heart Association and numerous longitudinal health surveys show that lifestyle changes can prevent or dramatically reduce the risk of heart disease, even for those with genetic predispositions.
Why is prevention so powerful?
Because by the time you feel pain, damage has already occurred. Prevention means stopping the damage before it starts—or before it becomes irreversible.
It’s not just about living longer. It’s about living better—more energy, fewer medications, a sharper mind, and the freedom to enjoy life without the burden of chronic illness.
The Heart-Smart Diet: Eating to Live
Your plate may be the most important battlefield in the war against heart disease.
A heart-healthy diet is not about deprivation. It’s about nourishment, balance, and sustainability. The key principles are simple:
- Eat more plants: Fruits, vegetables, whole grains, legumes, nuts, and seeds provide fiber, antioxidants, and healthy fats.
- Reduce saturated fats: Found in red meat, butter, cheese, and fried foods, these increase LDL cholesterol.
- Eliminate trans fats: These artificial fats are banned in many places but can still lurk in processed snacks and baked goods.
- Increase omega-3s: Found in fatty fish like salmon and flaxseeds, omega-3s reduce inflammation and lower triglycerides.
- Watch your salt: Excess sodium raises blood pressure. Processed foods are the main culprits.
- Cut added sugars: Sugar overload contributes to obesity, diabetes, and lipid problems.
- Stay hydrated: Water helps regulate blood pressure and supports metabolism.
Popular dietary patterns like the Mediterranean Diet or DASH Diet (Dietary Approaches to Stop Hypertension) are backed by decades of research for their heart-protective effects.
The secret isn’t a magic food. It’s consistency. Small changes, sustained over time, transform your biology.
Move That Body: The Power of Exercise
If diet is one leg of the heart-health stool, exercise is the second.
The heart is a muscle—and like any muscle, it gets stronger with use. Regular physical activity improves circulation, strengthens the heart, reduces blood pressure, and improves insulin sensitivity.
It also burns calories, improves mood, reduces stress, and even boosts brain function.
The magic number? At least 150 minutes of moderate-intensity aerobic exercise (like brisk walking, swimming, or cycling) per week, plus muscle-strengthening activities on two days.
Even short bursts of activity—taking the stairs, walking after meals, dancing—add up.
For those with mobility issues or chronic conditions, even gentle movement like stretching, tai chi, or chair yoga can improve heart health.
Breaking the Chains: Quit Smoking, Reduce Alcohol
No single behavior causes more harm to the cardiovascular system than smoking.
Every puff damages the arteries, thickens the blood, lowers HDL cholesterol, and raises blood pressure. Smoking is directly linked to heart attacks, strokes, and sudden cardiac death.
But the good news is astonishing: The heart begins to heal almost immediately after quitting. Within a year, risk of heart disease drops by half. Within five years, the risk of stroke is close to that of a non-smoker.
Alcohol is more complicated. Some studies suggest moderate drinking (especially red wine) may offer a small benefit. But excessive alcohol is clearly harmful, raising blood pressure and contributing to obesity and arrhythmias.
The safest approach: Moderation, or abstinence, depending on your health profile.
Stress and the Heart: A Hidden Enemy
Stress isn’t just a feeling. It’s a physical state that floods the body with adrenaline and cortisol, raising heart rate and blood pressure. Chronic stress can lead to unhealthy behaviors—overeating, drinking, smoking—as well as direct damage to blood vessels.
Stress also affects sleep, and poor sleep is a significant risk factor for heart disease.
What can help?
- Mindfulness and meditation
- Deep breathing
- Regular physical activity
- Quality sleep (7–9 hours)
- Social connection and support
- Time in nature
It’s not about eliminating stress—life doesn’t work that way. It’s about managing it with tools and habits that give the heart a break.
Know Your Numbers: Regular Checkups Matter
Many of heart disease’s deadliest risks are silent. High blood pressure, high cholesterol, and high blood sugar can do immense damage without symptoms.
That’s why regular checkups and lab tests are critical. These include:
- Blood pressure
- Cholesterol profile (LDL, HDL, triglycerides)
- Blood glucose (and HbA1c for diabetics)
- Weight and body mass index
- Electrocardiogram (ECG)
- Coronary calcium scan (for high-risk individuals)
Knowing your numbers means knowing your risk—and taking action before it’s too late.
The Role of Medication: When Lifestyle Isn’t Enough
For many people, lifestyle changes can bring cholesterol, blood pressure, and glucose under control. But some individuals, especially those with genetic risks, may need medication.
Common drugs include:
- Statins – lower LDL cholesterol and reduce plaque formation.
- ACE inhibitors and ARBs – lower blood pressure and protect arteries.
- Beta-blockers – reduce heart rate and blood pressure.
- Aspirin – thins the blood (though now used more selectively).
Medication isn’t a sign of failure. It’s a tool—often a life-saving one. But it works best when combined with healthy habits.
Reversing the Course: Can Heart Disease Be Undone?
This is one of the most exciting areas of cardiovascular medicine. Emerging evidence suggests that some forms of heart disease can be reversed—especially in early stages.
Dr. Dean Ornish and others have shown that intensive lifestyle changes—plant-based diet, exercise, stress reduction, and support—can reduce plaque and improve blood flow.
Other studies show that weight loss, blood pressure control, and smoking cessation can stabilize plaques and reduce the risk of rupture.
The heart, in many ways, is remarkably resilient.
Conclusion: Your Heart, Your Future
Heart disease may be the world’s top killer—but it is not fate.
It’s the result of millions of small decisions, made every day, over years. That means it can be prevented by millions of small decisions made differently—starting now.
Whether you’re 20 or 70, healthy or at risk, your heart’s future is shaped by what you do today.
Eat well. Move often. Rest deeply. Breathe fully. Love widely. Get your checkups. Know your numbers. Take action—not in fear, but in empowerment.
Because this small, silent engine in your chest beats for one reason: to carry you through a life worth living.
And you have the power to keep it beating strong.