Cancer. The word alone has the power to inspire fear, confusion, and urgency. Despite decades of progress in medical science, this one disease—or rather, this vast family of diseases—continues to claim millions of lives each year. Nearly every person on Earth has been touched by cancer in some way—through personal experience, a family member, or a friend. It spares no age, nationality, or gender. It’s indiscriminate, unpredictable, and for many, still not fully understood.
Yet despite its seeming mystery, science has uncovered a great deal about cancer—what causes it, how it grows, how it mutates, and how it might be stopped. This article will explore, in depth, the known causes of cancer, from genetic mutations to environmental exposures, and from viruses to lifestyle choices. We’ll look into the biology of how cancer begins and evolves, how it outsmarts the immune system, and what researchers are doing to combat it.
This isn’t just about disease—it’s about biology, chemistry, history, and the human condition. And above all, it’s about hope through understanding.
The Fundamentals: What Exactly Is Cancer?
Before we dive into causes, it’s important to answer the fundamental question: What is cancer?
At its core, cancer is a disease of uncontrolled cell growth. Your body is made of trillions of cells, each with specific roles. These cells grow, divide, and die in an organized and regulated fashion. The process is tightly controlled by genes—segments of DNA that tell cells how to function.
Cancer occurs when this process goes haywire.
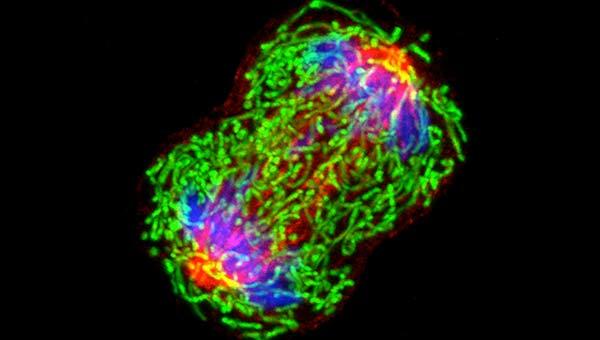
Instead of dying when they should, damaged or abnormal cells begin to divide uncontrollably. These rogue cells can form masses called tumors, and in many cases, they can invade nearby tissues and spread to other parts of the body—a process called metastasis.
Not all cancers form solid tumors. For example, leukemias, or blood cancers, involve abnormal cells circulating through the bloodstream or accumulating in the bone marrow. But whether solid or liquid, localized or metastatic, all cancers share a common feature: their origin lies in genetic damage that allows cells to escape the normal rules of life.
The Genetic Roots of Cancer: Mutation Is the Spark
At the molecular level, cancer starts with mutations—changes in DNA. These mutations can arise in two primary ways: they can be inherited or acquired.
Inherited mutations are passed down from parent to child. For example, mutations in the BRCA1 or BRCA2 genes significantly increase the risk of breast and ovarian cancer. These mutations are present in every cell of the body from birth.
Acquired mutations, on the other hand, happen during a person’s lifetime. They can be the result of environmental exposure, lifestyle choices, infections, or simply random errors during cell division. The majority of cancers are caused by acquired mutations rather than inherited ones.
But not all mutations cause cancer. The ones that do typically affect three types of genes:
- Oncogenes – These are genes that, when mutated, become overly active and tell cells to grow uncontrollably.
- Tumor suppressor genes – These genes normally slow down cell growth or signal when a cell should die. Mutations can silence these critical functions.
- DNA repair genes – These genes fix damage in DNA. When they are faulty, errors accumulate, leading to further mutations.
Cancer usually requires a combination of mutations over time. That’s why it’s more common in older people: they’ve had more time for damage to build up.
Environmental Carcinogens: Invisible Assailants
Now that we understand the role of mutations, the next question becomes: what causes those mutations?
One major category is environmental carcinogens—external substances or exposures that can damage DNA and increase cancer risk.
Tobacco smoke is perhaps the most notorious carcinogen. Smoking introduces over 7,000 chemicals into the lungs, including at least 70 known carcinogens. These chemicals cause direct DNA damage, especially to lung cells, and are the leading cause of lung cancer worldwide. But smoking doesn’t only cause lung cancer—it’s also linked to cancers of the mouth, throat, esophagus, bladder, kidney, pancreas, and more.
Ultraviolet (UV) radiation from the sun is another powerful carcinogen. UV rays penetrate the skin and cause mutations in the DNA of skin cells. Over time, this can lead to skin cancers, including melanoma, one of the deadliest forms. Tanning beds are even more dangerous, delivering concentrated doses of UV radiation.
Ionizing radiation, such as from X-rays or radioactive materials, is also a known carcinogen. Survivors of atomic bomb explosions and those exposed to nuclear accidents, like Chernobyl, have shown higher rates of cancers, especially thyroid cancer.
Chemical exposure in workplaces or industries can also increase cancer risk. For example, asbestos, once widely used in construction, is strongly linked to mesothelioma, a rare but aggressive cancer of the lung lining. Benzene, used in manufacturing, has been linked to leukemia.
The key takeaway: many environmental carcinogens are avoidable, and public health measures—like smoking bans and workplace safety regulations—have made a significant difference in cancer prevention.
Viral and Bacterial Triggers: The Infectious Connection
It may surprise you to learn that certain infections can lead to cancer. In fact, viruses and bacteria are responsible for an estimated 15% of cancers worldwide.
The human papillomavirus (HPV) is perhaps the most well-known. HPV is a sexually transmitted virus, and certain high-risk strains can cause cervical cancer, as well as cancers of the throat, anus, penis, and vagina. The good news is that vaccines against HPV are highly effective and can prevent the majority of these cancers.
The hepatitis B and C viruses can cause chronic liver infections that increase the risk of liver cancer. Again, vaccination and antiviral treatments play a key role in prevention.
Helicobacter pylori, a type of bacteria that infects the stomach lining, has been linked to stomach cancer and gastric lymphoma. It’s treatable with antibiotics, which can significantly reduce cancer risk.
Epstein-Barr virus (EBV), known for causing mononucleosis, has also been associated with certain lymphomas and nasopharyngeal carcinoma.
These infectious agents cause cancer not just by triggering chronic inflammation but also by inserting viral genes into human DNA, disrupting normal cellular functions and paving the way for malignancy.
Lifestyle Factors: Choices That Matter
While we can’t control our genes or completely avoid environmental carcinogens, we can make lifestyle choices that either reduce or increase cancer risk.
Diet and nutrition play a major role. High consumption of processed meats like bacon and sausages has been linked to colorectal cancer, likely due to nitrates and nitrites. Diets rich in fruits, vegetables, and fiber appear to be protective, though the exact mechanisms are still being studied.
Alcohol is another risk factor. Ethanol, the active component in alcoholic drinks, is a Group 1 carcinogen, the same category as tobacco and asbestos. Alcohol can increase the risk of cancers of the liver, breast, esophagus, and more.
Obesity is linked to at least 13 different types of cancer. Excess fat leads to chronic inflammation and hormone imbalances, particularly increased levels of estrogen and insulin, which can promote tumor growth.
Physical inactivity is also a risk. Regular exercise has been shown to reduce the risk of colon, breast, and endometrial cancer, among others.
And let’s not forget sleep. Disrupted circadian rhythms, especially in night shift workers, have been associated with higher cancer rates—possibly due to hormone changes and immune suppression.
In short, the body is an ecosystem. How you treat it affects how likely it is to succumb to disease—including cancer.
The Immune System: Friend, Foe, and Battleground
One of the most fascinating aspects of cancer biology is the relationship between tumors and the immune system.
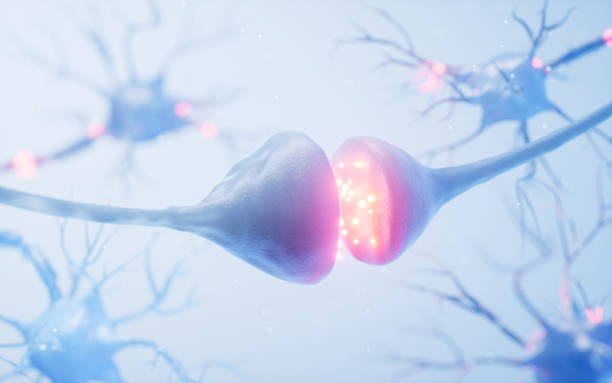
Ordinarily, your immune system is vigilant. It can recognize and destroy abnormal cells before they become a problem—a process known as immune surveillance. However, cancer cells can develop tricks to evade detection. They might hide their abnormal proteins, release chemicals that suppress immune responses, or even hijack immune cells to help them grow.
This has led to one of the most promising advances in modern medicine: immunotherapy. Drugs known as checkpoint inhibitors—like pembrolizumab or nivolumab—essentially take the brakes off the immune system, allowing it to recognize and attack tumors. Other approaches include CAR-T cell therapy, in which a patient’s immune cells are genetically engineered to hunt down cancer.
The immune system is not just a passive observer—it’s a battlefield. And in the war against cancer, it may be our greatest weapon.
Epigenetics: More Than Just Genes
Beyond genetic mutations lies a lesser-known but equally important field: epigenetics.
Epigenetics refers to changes in how genes are expressed—without altering the DNA sequence itself. It’s like a dimmer switch that can turn genes up or down.
Cancer can arise when epigenetic regulators go awry. For instance, a tumor suppressor gene might be silenced not by mutation, but by chemical tags (like methyl groups) added to its DNA. This subtle sabotage can be just as dangerous as a mutation.
The exciting part is that epigenetic changes are reversible. This has opened the door to epigenetic therapies, drugs that can “reprogram” cancer cells or make them more susceptible to other treatments.
Epigenetics also explains why identical twins—with the same DNA—can have different cancer risks. Lifestyle and environment can literally change how genes behave, for better or worse.
Stem Cells and the Cancer Hierarchy
Recent research has shown that not all cancer cells are equal. In some tumors, a small subset of cells—called cancer stem cells—have the unique ability to self-renew and regenerate the entire tumor population.
This has huge implications. Cancer stem cells are often more resistant to treatment, and even if 99% of a tumor is destroyed, these few survivors can cause a relapse.
Understanding and targeting cancer stem cells is a frontier in oncology. If we can cut the root, the tree cannot regrow.
Aging and Cancer: A Natural Link
Age is the single biggest risk factor for cancer. As we get older, our cells accumulate more mutations, our immune system weakens, and our tissues become more susceptible to transformation.
But aging is more than just time. It involves biological processes like telomere shortening, oxidative stress, and inflammation—all of which can contribute to cancer development.
Scientists are exploring ways to slow aging, not just to increase lifespan, but to reduce age-related diseases like cancer. In doing so, they may uncover new strategies for prevention and therapy.
The Future: Prevention, Precision, and Personalization
Medical science has come a long way in understanding the causes of cancer. We now know it’s a multifactorial disease—a result of genetic predisposition, environmental exposures, infections, lifestyle choices, and aging. But knowledge alone isn’t enough. What matters is how we use it.
Cancer prevention is one of the most effective strategies we have. Vaccination (against HPV and hepatitis), tobacco cessation, healthy diet, exercise, and regular screenings can drastically reduce cancer incidence.
Precision medicine is transforming cancer care. By analyzing a tumor’s genetic profile, doctors can choose targeted therapies that are more effective and less toxic. A breast cancer patient with a HER2-positive tumor, for example, can receive trastuzumab, a drug that specifically targets the HER2 receptor.
Artificial intelligence, liquid biopsies, and gene editing (like CRISPR) are rapidly advancing the way we diagnose, monitor, and treat cancer.
We’re moving from a one-size-fits-all approach to personalized oncology—where treatment is tailored not just to the type of cancer, but to the individual patient’s biology.
Conclusion: Understanding Brings Power
Cancer is not a single disease. It’s a complex, evolving, and deeply personal journey shaped by countless biological and environmental variables. While its causes are diverse—from gene mutations to viral infections, from lifestyle to aging—they are increasingly within our grasp to understand, predict, and even prevent.
The battle against cancer is far from over. But thanks to science, it is no longer shrouded in mystery. Every breakthrough, every discovery, every piece of knowledge adds a new weapon to our arsenal.
And as we continue to explore not just what causes cancer—but how to stop it—we move closer to a future where cancer may not just be treatable, but preventable and curable.
Understanding cancer is not just a medical necessity—it’s a human triumph.