Imagine your body as a finely tuned orchestra. Each organ, hormone, and cell plays a role in harmony, creating a masterpiece of health. Now picture a disruption in that harmony—a single instrument out of tune. That’s what happens with diabetes. It’s not merely a disease of “too much sugar” in the blood. It’s a complex condition that affects nearly every part of the body, reshaping lives, daily habits, and long-term health outcomes. Yet despite being one of the most studied chronic illnesses on the planet, many people don’t fully understand what diabetes really is, why it happens, how it feels, and how it can be managed—or even prevented.
Diabetes isn’t just one disease. It’s a group of metabolic disorders. And it doesn’t discriminate. It touches the lives of the young and old, rich and poor, from the bustling cities of the West to remote villages of the East. It’s silent, progressive, and can be deadly if ignored. But with awareness, early detection, and careful management, people with diabetes can lead full, vibrant lives.
This article dives deep into the world of diabetes: what it is, what causes it, what symptoms to look out for, and how we can treat and manage it. Let’s embark on this journey to unravel one of the most important health issues of our time.
What Exactly Is Diabetes?
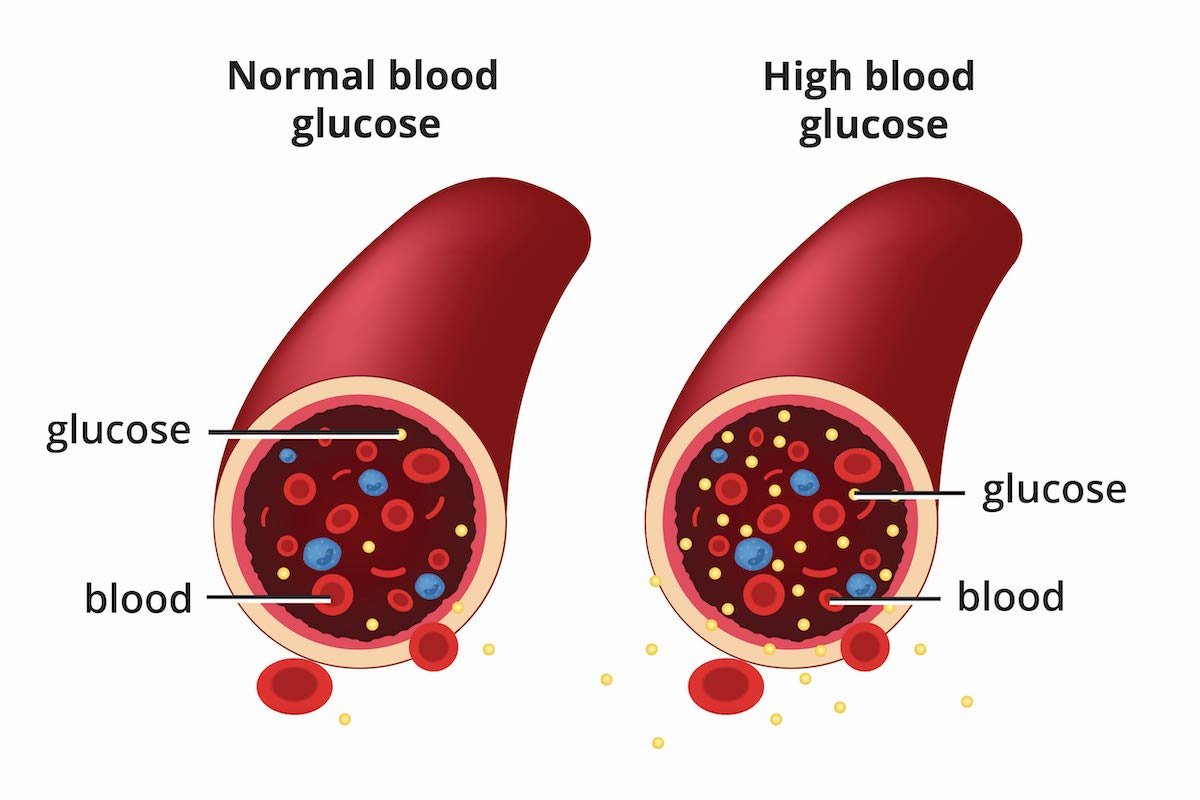
At its core, diabetes mellitus is a chronic condition that affects how your body turns food into energy. Most of what you eat is broken down into glucose (a type of sugar) and released into the bloodstream. When your blood sugar rises, your pancreas is supposed to release insulin—a hormone that acts like a key to let glucose enter your cells and be used for energy.
But in diabetes, one of two things happens: either your body doesn’t make enough insulin, or it doesn’t use insulin properly. As a result, too much glucose stays in the bloodstream. Over time, this excess sugar can lead to serious health problems like heart disease, vision loss, kidney failure, and nerve damage.
Diabetes is often categorized into three main types—Type 1, Type 2, and gestational diabetes. Each has its own causes, characteristics, and management strategies. Understanding these differences is crucial to navigating the journey of treatment and care.
Type 1 Diabetes: The Autoimmune Intruder
Type 1 diabetes is an autoimmune condition. Here, the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Think of it as friendly fire—your body harming its own machinery. Once these cells are gone, the body can no longer produce insulin.
This type usually appears in childhood or adolescence, which is why it was once called juvenile diabetes, though it can develop at any age. The onset is often sudden and dramatic. A previously healthy child may suddenly become extremely thirsty, lose weight rapidly, and feel tired all the time. Without insulin, they can’t survive.
But insulin therapy changes everything. Type 1 diabetics must take insulin every day, either through injections or an insulin pump. It’s a lifelong commitment to balancing food, activity, and insulin to keep blood sugar in check.
Researchers are still trying to understand why some people’s immune systems go rogue. Genetics play a role, as do environmental triggers like viruses. But there’s no known way to prevent Type 1 diabetes—for now.
Type 2 Diabetes: The Lifestyle Tsunami
Type 2 diabetes is by far the most common form, accounting for over 90% of all diabetes cases worldwide. It usually develops in adults over the age of 45, but alarmingly, it’s now appearing in teenagers and even children due to rising obesity rates and sedentary lifestyles.
In Type 2 diabetes, the body still produces insulin—but the cells stop responding to it properly. This is called insulin resistance. Over time, the pancreas struggles to keep up with the demand and insulin production dwindles.
The development of Type 2 diabetes is influenced by a mix of genetics, environment, and lifestyle. Being overweight or obese, especially with fat concentrated around the abdomen, significantly increases risk. So does physical inactivity, an unhealthy diet high in refined carbs and sugars, and chronic stress.
Unlike Type 1, Type 2 diabetes can sometimes be reversed—or at least put into remission—with dramatic lifestyle changes. Weight loss, increased physical activity, and dietary improvements can all restore insulin sensitivity and lower blood sugar naturally. When lifestyle isn’t enough, oral medications and eventually insulin may be needed.
Gestational Diabetes: When Pregnancy Takes a Detour
Gestational diabetes occurs during pregnancy, usually in the second or third trimester. Hormones produced by the placenta can interfere with insulin, leading to elevated blood sugar levels. While it usually resolves after childbirth, it can pose risks to both mother and baby.
Women with gestational diabetes are at higher risk for complications such as preeclampsia, high birth weight, and delivery via C-section. Their babies may suffer from low blood sugar at birth or face a higher risk of developing obesity or Type 2 diabetes later in life.
Though gestational diabetes often goes away after birth, it’s a warning sign. Mothers who experience it are at significantly higher risk of developing Type 2 diabetes later in life. That’s why postpartum screening and healthy lifestyle changes are so important.
Prediabetes: The Red Flag Before the Storm
Prediabetes is the gray zone between normal and diabetic blood sugar levels. It’s a crucial stage that offers a window of opportunity. People with prediabetes often feel perfectly fine—but their blood sugar levels are elevated enough to increase the risk of progressing to full-blown Type 2 diabetes.
More than 80% of people with prediabetes don’t even know they have it. But with early action—diet, exercise, weight loss—it’s possible to turn the tide and prevent diabetes altogether. It’s the moment when the body is sounding an alarm. Will we listen?
Symptoms: The Body’s Cry for Help
The symptoms of diabetes can vary widely depending on the type, but there are some classic signs that the body sends out when blood sugar is too high. These include:
- Excessive thirst (polydipsia)
- Frequent urination (polyuria)
- Extreme hunger (polyphagia)
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing wounds
- Frequent infections, especially skin or urinary
- Numbness or tingling, particularly in hands or feet
In Type 1 diabetes, these symptoms often develop quickly and can be life-threatening if not treated immediately. In Type 2 diabetes, they may develop slowly and be easy to ignore. That’s why regular screenings are so important—especially if you’re over 40, overweight, or have a family history.
Causes: A Multi-Factorial Puzzle
Diabetes is never caused by one single thing. It arises from an interplay of multiple factors—some you can control, others you can’t.
Genetics play a strong role, especially in Type 2 diabetes. If your parents or siblings have diabetes, your risk goes up. However, having a genetic predisposition doesn’t guarantee you’ll get diabetes. Environment and lifestyle often determine whether the disease is triggered.
Obesity, particularly central obesity (fat around the waist), is one of the strongest modifiable risk factors. Fat tissue isn’t inert—it releases inflammatory substances that impair insulin’s function.
Diet, particularly one high in processed carbs, sugary drinks, red meats, and low in fiber, contributes heavily to insulin resistance.
Sedentary lifestyle reduces insulin sensitivity and promotes weight gain. Exercise is a powerful insulin sensitizer.
Age increases risk, especially after 45. But younger people aren’t immune—especially if they’re inactive or overweight.
Ethnicity matters too. People of South Asian, African, Hispanic, and Native American descent have higher risks of Type 2 diabetes.
Hormonal disorders, pancreatic diseases, certain medications, and even viral infections can all contribute to diabetes in specific cases.
Diagnosis: Uncovering the Hidden Truth
Diagnosing diabetes involves a few different blood tests:
- Fasting Blood Glucose – measures blood sugar after 8 hours of fasting. A level of 126 mg/dL or higher suggests diabetes.
- Oral Glucose Tolerance Test (OGTT) – blood sugar is tested 2 hours after drinking a sugary liquid. A result of 200 mg/dL or more indicates diabetes.
- Hemoglobin A1c – reflects average blood sugar over the past 2–3 months. A level of 6.5% or higher confirms diabetes.
Doctors may also perform urine tests, lipid panels, kidney function tests, and eye exams to assess complications.
Treatment: The Trilogy of Care
The cornerstone of diabetes treatment revolves around three pillars: diet, exercise, and medication.
Diet: Food as Medicine
A healthy diet is critical. The focus is on:
- Low glycemic index foods that don’t spike blood sugar
- Whole grains, legumes, vegetables, and lean proteins
- Healthy fats like olive oil and nuts
- Avoiding sugary drinks, refined carbs, and trans fats
Portion control, balanced meals, and carb counting are key skills. Dietitians can tailor plans based on individual needs and culture.
Exercise: Moving Toward Better Health
Physical activity lowers blood sugar by improving insulin sensitivity and helping muscles use glucose. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, plus strength training twice a week.
Even small changes matter—walking after meals, taking the stairs, stretching at work.
Medication: Chemistry in Control
When lifestyle isn’t enough, medication steps in. Options include:
- Metformin – the first-line drug that lowers glucose production in the liver.
- Sulfonylureas – stimulate the pancreas to produce more insulin.
- DPP-4 inhibitors, GLP-1 agonists, and SGLT2 inhibitors – newer classes that control blood sugar through different mechanisms.
- Insulin therapy – essential for Type 1, and sometimes needed in advanced Type 2.
Each medication has its pros, cons, and side effects. Personalized treatment is crucial.
Complications: The Ripple Effect
Uncontrolled diabetes can damage nearly every system in the body. Over time, it increases the risk of:
- Heart disease and stroke
- Kidney failure (nephropathy)
- Nerve damage (neuropathy) leading to pain, numbness, or even amputation
- Eye damage (retinopathy) and blindness
- Foot ulcers that don’t heal
- Skin infections
- Mental health issues, including depression and anxiety
These complications are why tight blood sugar control is so vital—and why regular checkups are non-negotiable.
Living Well With Diabetes
A diabetes diagnosis can feel overwhelming. But it’s not a death sentence. With knowledge, support, and tools, people with diabetes can thrive.
Education is power. Learn how food, stress, illness, and activity affect your blood sugar.
Monitoring with a glucometer or continuous glucose monitor helps make informed choices.
Support networks, online communities, and diabetes educators offer emotional and practical help.
Technology, from insulin pumps to smartphone apps, is revolutionizing diabetes care.
It takes work, but it’s worth it. Many people with diabetes become healthier than they were before diagnosis—because it forces them to pay attention to their bodies, eat better, move more, and take ownership of their health.
The Future of Diabetes: Hope on the Horizon
The fight against diabetes is far from over, but science is advancing fast. Some promising developments include:
- Artificial pancreases that automatically regulate blood sugar
- Stem cell therapies to regenerate insulin-producing cells
- Immunotherapies for preventing or reversing Type 1 diabetes
- New drug classes with cardiovascular and kidney benefits
- Precision nutrition and genetic testing to personalize treatment
Perhaps the most powerful tool, however, is prevention. Public health campaigns, community education, and systemic changes to diet and exercise habits could drastically reduce new cases of Type 2 diabetes worldwide.
Conclusion: A Balancing Act Worth Mastering
Diabetes is a complex, multifaceted condition. It involves biology and behavior, genetics and lifestyle, medicine and mindset. It can be a silent menace—but also a call to transformation.
With early diagnosis, informed choices, and consistent care, diabetes can be managed. And with continued research and public awareness, future generations may look back on it not as a crisis—but as a challenge we rose to meet.
The key lies in understanding. The more we learn, the more we listen to our bodies, and the more we support one another, the better our chances of winning the battle—one drop of blood, one smart choice, one hopeful heartbeat at a time.