A stroke is one of the most terrifying medical events that can happen to the human body. It strikes suddenly, often without warning, disrupting the very control center of our existence—the brain. A person may be speaking clearly one moment and unable to form words the next. A hand may drop, a face may go slack, or a leg might refuse to move. In seconds, everything can change.
But what is a stroke, exactly?
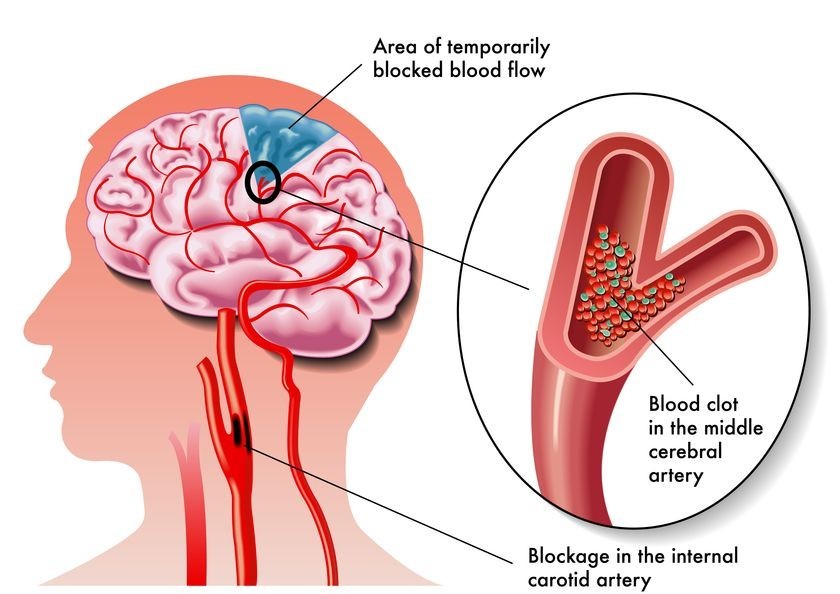
In medical terms, a stroke (also known as a cerebrovascular accident) occurs when blood flow to part of the brain is interrupted or severely reduced. This deprivation robs brain cells of oxygen and nutrients, causing them to begin dying within minutes. Because the brain controls every function of the body—from breathing to speech to movement—damage to even a small area can have catastrophic consequences.
Strokes are medical emergencies. But they are also preventable, treatable, and—crucially—survivable. To understand stroke is to gain power over one of the most formidable health threats we face today.
The Brain’s Delicate Balance
The human brain, despite weighing only about 3 pounds, is the most energy-hungry organ in the body. It consumes roughly 20% of all oxygen and calories you take in, every single day. That’s because it must continuously manage countless activities—both conscious and unconscious.
The brain’s billions of neurons rely on a constant supply of oxygen-rich blood to function. Unlike muscles, the brain cannot store energy in the form of glycogen. If blood flow stops, neurons begin dying almost immediately.
When blood flow to a part of the brain is interrupted—even briefly—the resulting damage can be severe. Which functions are affected depends entirely on where in the brain the stroke occurs.
A stroke in the left hemisphere might impair speech, logic, and the ability to understand language. A stroke in the right hemisphere might affect spatial awareness, facial recognition, or musical perception. A stroke in the brainstem can disrupt essential life functions like breathing or heartbeat.
That’s what makes strokes so dangerous—and so unpredictable.
Types of Stroke: The Two Major Categories
Strokes come in different forms, each with distinct causes and outcomes. Understanding these types is the first step toward grasping the nature of the disease.
Ischemic Stroke: The Most Common Type
About 85% of all strokes are ischemic. These occur when a blood clot blocks or narrows an artery leading to the brain, cutting off blood supply. This is similar to how a heart attack happens—but in the brain instead of the heart.
There are two main kinds of ischemic stroke:
Thrombotic strokes occur when a blood clot (thrombus) forms in one of the arteries supplying blood to the brain, often due to atherosclerosis (a buildup of fatty plaques).
Embolic strokes happen when a clot forms elsewhere in the body—often the heart—and travels to the brain, where it lodges in a smaller vessel. This is common in people with atrial fibrillation, a type of irregular heartbeat that can cause blood to pool and clot.
Hemorrhagic Stroke: When Blood Vessels Burst
The other 15% of strokes are hemorrhagic, caused by the rupture of a blood vessel in the brain. Instead of a blockage, these strokes involve bleeding into or around the brain, which causes pressure and damage to surrounding tissue.
Hemorrhagic strokes are often more severe and have a higher risk of death. They include:
Intracerebral hemorrhage, where an artery inside the brain bursts and leaks into brain tissue.
Subarachnoid hemorrhage, where bleeding occurs in the space between the brain and the thin tissues covering it, often caused by a ruptured aneurysm.
Risk factors for hemorrhagic stroke include high blood pressure, head trauma, blood thinners, and vascular malformations.
Warning Signs: The Brain’s Cry for Help
The key to surviving a stroke lies in speed. Time lost is brain lost. Every minute counts.
The symptoms of stroke can vary based on the type and location, but the most common signs can be remembered using the acronym F.A.S.T.:
- Face: Ask the person to smile. Does one side droop?
- Arms: Ask them to raise both arms. Does one drift downward?
- Speech: Ask them to speak. Is speech slurred or strange?
- Time: If you see any of these signs, call emergency services immediately.
Other warning signs may include:
- Sudden confusion or difficulty understanding speech
- Sudden numbness or weakness, especially on one side
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, or loss of balance
- Sudden severe headache with no known cause
It’s important to note that these symptoms can be brief or subtle, especially with a transient ischemic attack (TIA)—sometimes called a “mini-stroke.” But even if symptoms disappear, a TIA is a red flag. It often precedes a full-blown stroke, and immediate medical attention is critical.
Behind the Blockage: Causes and Risk Factors
Stroke is not a random bolt from the blue. In most cases, it is the result of long-term damage to the circulatory system and brain. Many of the causes are preventable or manageable.
High Blood Pressure: The Silent Killer
Hypertension is the single most significant risk factor for stroke. High pressure can damage blood vessels over time, making them more prone to rupture or clot formation. Many people live with high blood pressure without symptoms until a crisis occurs.
Atrial Fibrillation: The Irregular Risk
Atrial fibrillation (AFib), a common heart rhythm disorder, increases stroke risk fivefold. Irregular heartbeats can lead to blood pooling and clot formation in the heart, which can then travel to the brain.
Smoking: Poison for the Brain
Smoking thickens blood, promotes clot formation, damages blood vessels, and raises blood pressure—all perfect ingredients for a stroke. Quitting smoking immediately lowers risk.
Diabetes: Sugar and the Brain
Diabetes damages blood vessels throughout the body, including those in the brain. It also increases the risk of atherosclerosis, hypertension, and heart disease—all stroke risk factors.
Cholesterol and Atherosclerosis
High LDL cholesterol can lead to plaque buildup in arteries, narrowing them and setting the stage for thrombotic strokes. HDL cholesterol, the “good” kind, helps clear excess cholesterol from the bloodstream.
Obesity and Inactivity
Being overweight strains the heart and circulatory system. Sedentary lifestyles also increase risk, while regular exercise helps regulate weight, blood pressure, and cholesterol.
Alcohol and Drug Use
Heavy drinking can raise blood pressure and increase the likelihood of hemorrhagic stroke. Cocaine and other stimulants can cause sudden blood vessel rupture or extreme hypertension.
Diagnosis: Imaging the Crisis
When a patient arrives at the hospital with stroke symptoms, the first priority is diagnosis. Determining whether the stroke is ischemic or hemorrhagic is critical, as treatments for each are radically different.
CT Scan and MRI
A CT (computed tomography) scan is often the first test, used to detect bleeding or other abnormalities. A MRI (magnetic resonance imaging) provides more detailed images of brain tissue and can show areas of damage.
Angiography
Cerebral angiography uses dye and X-rays to visualize blood vessels in the brain. This can help identify blockages, aneurysms, or malformed vessels.
Blood Tests
Blood tests can check for clotting problems, infection, blood sugar levels, and chemical imbalances that might contribute to stroke symptoms.
ECG and Echocardiogram
Heart tests like electrocardiograms (ECG) and echocardiograms can detect atrial fibrillation, heart disease, or clots in the heart that may have caused an embolic stroke.
Emergency Treatment: Racing Against Time
For ischemic stroke, time is everything. The main goal is to restore blood flow to the brain as quickly as possible.
Thrombolytic Therapy
Tissue plasminogen activator (tPA) is a clot-busting drug that can dissolve blockages in arteries. It must be administered within a narrow window—generally 3 to 4.5 hours after symptoms begin.
tPA can dramatically improve outcomes, but it carries risks, especially of bleeding, so precise diagnosis is essential.
Mechanical Thrombectomy
In some cases, surgeons can remove a clot using a catheter inserted into a blood vessel—called a mechanical thrombectomy. This is most effective within 6 to 24 hours of symptom onset and depends on the stroke’s location.
Hemorrhagic Stroke Interventions
For hemorrhagic strokes, the focus shifts to stopping the bleeding and relieving pressure in the brain. This may involve:
- Surgery to remove blood or repair a ruptured vessel
- Medications to lower blood pressure
- Drugs to reverse the effects of blood thinners
Rehabilitation: The Road to Recovery
Surviving a stroke is just the beginning. Recovery can be a long and arduous process, requiring tremendous patience, determination, and support.
The brain is a resilient organ with some capacity to rewire itself—a phenomenon known as neuroplasticity. With therapy, lost functions can sometimes be regained or relearned.
Physical Therapy
Physical therapy focuses on restoring strength, coordination, and balance. Stroke survivors may need to relearn how to walk, use their arms, or perform everyday tasks.
Occupational Therapy
Occupational therapy helps people regain independence by retraining them in basic activities like eating, dressing, and writing. It may also involve adapting the home environment for accessibility.
Speech and Language Therapy
If the stroke affected speech or language centers, a speech-language pathologist can help with speaking, understanding, reading, and writing. Swallowing therapy may also be needed.
Psychological Support
Stroke often brings emotional and psychological challenges, including depression, anxiety, and frustration. Counseling, support groups, and medications can help survivors and caregivers alike.
Cognitive Rehabilitation
Cognitive therapy addresses problems with memory, attention, and problem-solving. It’s especially important for those who wish to return to work or complex activities.
The Personal Journey: Stories of Survival
Behind every stroke statistic is a human story—one of loss, courage, adaptation, and sometimes remarkable recovery.
Some survivors regain nearly all function. Others face permanent disability. But many find new purpose, strength, and meaning in their journey, becoming advocates, artists, athletes, or educators.
Survivors often say that a stroke forces you to slow down, re-evaluate life, and value each moment. Families grow closer. Communities form. Hope re-emerges.
These stories remind us that while stroke can be devastating, it is not the end.
Prevention: A Powerful Shield
Up to 80% of strokes are preventable. That’s a staggering number—and a call to action.
You can reduce your risk significantly by:
- Controlling blood pressure
- Managing cholesterol and diabetes
- Eating a heart-healthy diet (rich in fruits, vegetables, and whole grains)
- Exercising regularly
- Avoiding smoking and excessive alcohol
- Treating atrial fibrillation
- Getting regular checkups
Know your numbers—blood pressure, cholesterol, blood sugar—and talk with your healthcare provider about any concerns.
Conclusion: A Call to Awareness
Stroke is one of the leading causes of death and disability in the world, but it is also one of the most misunderstood. By demystifying its causes, symptoms, treatment, and recovery, we can replace fear with knowledge—and knowledge with action.
Whether you are a survivor, caregiver, medical professional, or simply someone who wants to protect your future, understanding stroke is the first step.
Remember: the brain is the seat of who you are. Protect it. Listen to it. Learn from it. And if ever a stroke strikes—know that with speed, science, and support, survival is possible. And recovery is real.