In the early 1980s, a mysterious illness began to appear in hospitals across the United States. Young, otherwise healthy men were suddenly developing rare infections and aggressive cancers that doctors had never expected to see in such patients. What began as confusion and fear soon became one of the greatest public health crises of modern times: the HIV/AIDS epidemic.
More than four decades later, HIV/AIDS remains one of the most studied, feared, and misunderstood diseases in human history. It is a virus that has reshaped medicine, science, and society. Yet it is also a story of resilience, innovation, and hope. While millions have died, millions more are alive today thanks to advancements in diagnosis, treatment, and prevention.
To understand HIV/AIDS is to understand not just a disease, but also the human struggle against stigma, inequality, and despair. In exploring its causes, symptoms, diagnosis, and treatment, we uncover not only the biology of a virus but also the enduring spirit of those who continue to fight it.
What Is HIV/AIDS?
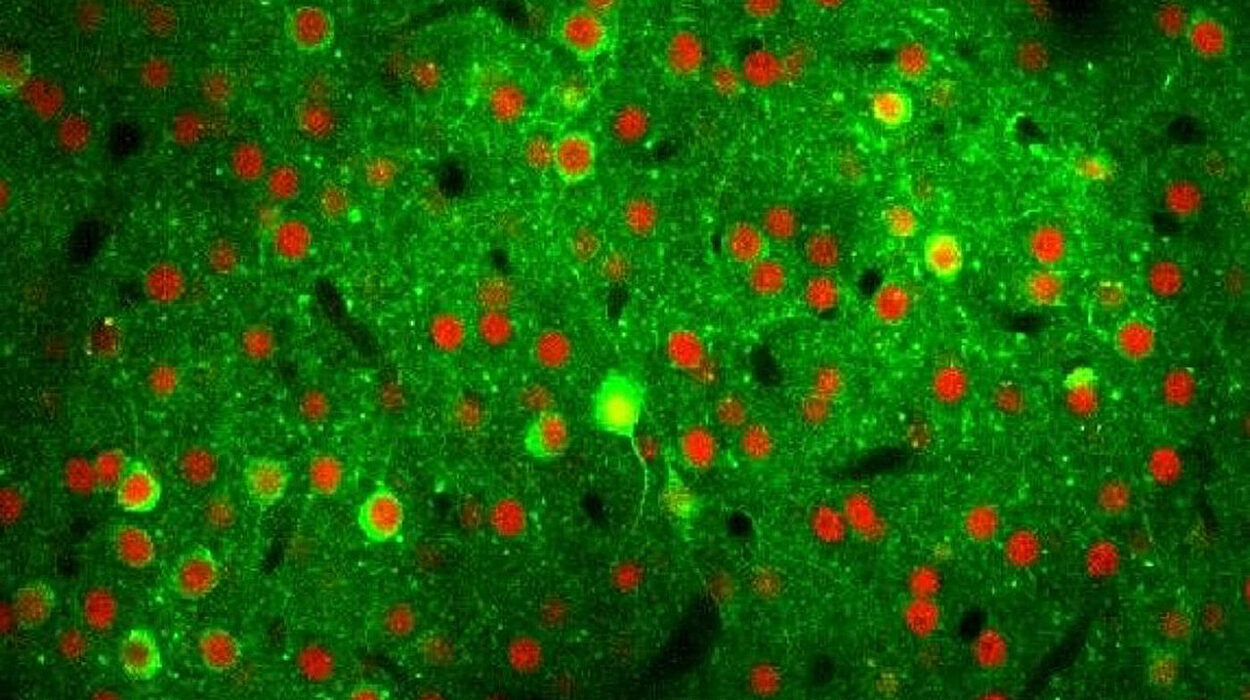
HIV, or Human Immunodeficiency Virus, is a virus that attacks the immune system—the body’s natural defense against infections. Specifically, HIV targets CD4 cells (also known as T-helper cells), which play a crucial role in coordinating the immune response. Over time, if left untreated, HIV destroys so many of these cells that the body becomes vulnerable to opportunistic infections and certain cancers.
AIDS, or Acquired Immunodeficiency Syndrome, is the most advanced stage of HIV infection. Not everyone with HIV develops AIDS, but without treatment, HIV almost inevitably progresses to this stage. AIDS is not a single disease but a collection of conditions that occur because the immune system can no longer defend itself.
In short:
- HIV is the virus.
- AIDS is the condition that results from severe immune system damage caused by HIV.
The Causes: How HIV Infects the Body
The Virus Itself
HIV belongs to a group of viruses called retroviruses. Unlike many other viruses, retroviruses carry their genetic information in the form of RNA rather than DNA. When HIV infects a cell, it uses an enzyme called reverse transcriptase to convert its RNA into DNA, which is then integrated into the host’s genetic material. This allows the virus to hijack the cell’s machinery and produce more copies of itself.
The virus primarily targets CD4 cells. Once inside, HIV replicates and eventually destroys the host cell, releasing new viral particles that go on to infect other cells. This ongoing cycle gradually weakens the immune system.
Transmission: How HIV Spreads
HIV spreads through contact with certain body fluids of a person who has the virus. These fluids include:
- Blood
- Semen and pre-seminal fluid
- Vaginal fluids
- Rectal fluids
- Breast milk
The virus enters the body through mucous membranes (such as those in the genitals, rectum, or mouth), through damaged tissue, or directly into the bloodstream.
The most common routes of transmission include:
- Unprotected sexual intercourse
- Sharing needles or syringes
- Receiving contaminated blood transfusions or organ transplants (rare today due to screening)
- From mother to child during pregnancy, childbirth, or breastfeeding
It is important to emphasize that HIV cannot be spread through casual contact—such as hugging, kissing, sharing food, or touching objects. This fact has been central in debunking stigma and misinformation about the virus.
Risk Factors
Certain behaviors and conditions increase the risk of acquiring HIV. These include having multiple sexual partners without protection, engaging in unprotected anal sex (which has a higher risk of transmission than vaginal sex), sharing injection equipment, or living in areas with high prevalence and limited access to healthcare.
The Progression of HIV Infection
The course of HIV infection unfolds in several stages, each with distinct features.
Acute HIV Infection
Within 2 to 4 weeks after exposure, many people experience flu-like symptoms such as fever, sore throat, swollen lymph nodes, and rash. This is called acute HIV infection and represents the body’s initial immune response. During this stage, the virus is replicating rapidly, and viral load (the amount of virus in the blood) is very high, making transmission to others more likely.
Clinical Latency
After the acute phase, the virus enters a stage of relative calm known as clinical latency or chronic HIV infection. During this period, which can last several years, people may not have symptoms, but the virus continues to replicate at lower levels. Without treatment, the virus eventually weakens the immune system.
AIDS
When CD4 cell counts fall below 200 cells per cubic millimeter of blood, or when opportunistic infections and certain cancers appear, HIV infection is classified as AIDS. At this stage, the immune system is profoundly compromised. Without treatment, life expectancy is drastically reduced.
Symptoms: How HIV and AIDS Manifest
The symptoms of HIV vary depending on the stage of infection.
- Early symptoms (acute infection): fever, fatigue, swollen glands, rash, muscle aches, sore throat, night sweats.
- Chronic infection (latency): often no symptoms, though some may experience persistent swollen lymph nodes.
- Progression to AIDS: rapid weight loss, recurrent fevers, chronic diarrhea, extreme fatigue, pneumonia, skin lesions, neurological disorders, and recurrent opportunistic infections.
One of the cruelest aspects of HIV is that it can remain silent for years while still damaging the immune system. This is why early testing is critical.
Diagnosis: Detecting HIV
Diagnosing HIV has become much more accurate and accessible over the years.
Types of HIV Tests
- Antibody tests detect antibodies the body produces in response to HIV.
- Antigen/antibody combination tests (also known as fourth-generation tests) detect both HIV antibodies and a viral protein called p24 antigen, allowing for earlier detection.
- Nucleic acid tests (NATs) detect the virus’s genetic material directly and are the most sensitive, but they are costly and not used for routine screening.
The Window Period
After exposure, it takes time before HIV can be detected by tests. This is known as the “window period,” which typically ranges from 10 days to 3 months depending on the type of test. During this period, a person can be infectious even if their test results are negative.
Importance of Testing
Early diagnosis allows for timely treatment, which can prevent progression to AIDS and drastically reduce the risk of transmitting the virus to others. Widespread testing has been one of the cornerstones of global HIV prevention efforts.
Treatment: From Fatal to Manageable
When HIV was first discovered, a diagnosis was often seen as a death sentence. But today, thanks to advances in medicine, HIV is a manageable chronic condition for many people.
Antiretroviral Therapy (ART)
The primary treatment for HIV is antiretroviral therapy, or ART. This involves taking a combination of medicines that target different stages of the virus’s life cycle. By attacking the virus from multiple angles, ART reduces the viral load to undetectable levels.
Key outcomes of ART include:
- Restoring and preserving immune function
- Reducing the risk of opportunistic infections
- Preventing progression to AIDS
- Dramatically reducing the risk of transmitting HIV to others (“undetectable = untransmittable”)
ART does not cure HIV, but with consistent use, people with HIV can live long, healthy lives.
Adherence and Challenges
Treatment is lifelong and requires strict adherence. Missing doses can allow the virus to rebound and develop resistance. This makes counseling, education, and support systems crucial in HIV care.
Barriers such as poverty, stigma, lack of access to healthcare, and mental health challenges can interfere with treatment adherence. Addressing these barriers is as important as providing the medication itself.
Preventing Opportunistic Infections
In addition to ART, patients may need preventive medications to guard against opportunistic infections like tuberculosis, pneumonia, or fungal infections. Vaccinations, healthy lifestyle choices, and regular medical monitoring are also key.
Prevention: Stopping HIV Before It Spreads
While treatment is vital, prevention remains the most effective weapon against HIV/AIDS.
- Condom use dramatically reduces the risk of sexual transmission.
- Pre-exposure prophylaxis (PrEP) is a daily medication that can reduce the risk of acquiring HIV by more than 90% when taken consistently.
- Post-exposure prophylaxis (PEP) is a short-term treatment started within 72 hours after potential exposure to prevent infection.
- Harm reduction programs for people who inject drugs, such as needle exchange programs, significantly reduce transmission.
- Mother-to-child transmission prevention through ART during pregnancy, delivery, and breastfeeding can reduce the risk of transmission to below 2%.
Living with HIV: Beyond Biology
A diagnosis of HIV is not only a medical matter—it carries profound emotional, social, and cultural implications.
Stigma remains one of the greatest challenges. People living with HIV often face discrimination in healthcare, employment, and relationships. Fear and misinformation continue to fuel prejudice, despite decades of education campaigns.
Yet, stories of resilience abound. Many individuals and communities have turned their struggle into activism, leading to global movements that demand research, funding, and justice. From the early days of protests by AIDS activists to the present-day fight for equal access to treatment in low-income countries, the history of HIV/AIDS is also a history of courage.
The Global Picture
HIV/AIDS is a global pandemic, though its impact varies across regions. Sub-Saharan Africa carries the highest burden, with millions living with the virus and hundreds of thousands of new infections each year. Progress has been made, but inequalities in healthcare access continue to shape outcomes.
In wealthier nations, new infections have declined thanks to education, prevention, and treatment. But challenges persist, especially among marginalized groups such as men who have sex with men, transgender people, sex workers, and people who inject drugs.
Ending the epidemic will require not only medical tools but also social change—addressing poverty, inequality, and discrimination.
The Future: Hope on the Horizon
The story of HIV/AIDS is far from over, but there is reason for optimism. Researchers are pursuing vaccines, long-acting injectable treatments, and even potential cures. Clinical trials are exploring gene-editing technologies and immune-based therapies that could one day eliminate the virus from the body.
At the same time, global initiatives aim to expand access to testing, treatment, and prevention. The United Nations has set ambitious goals to end the epidemic as a public health threat.
Whether these goals will be met depends not only on science but also on political will, funding, and our collective commitment to equity and compassion.
A Human Perspective
Behind every statistic is a human being: a mother raising children, a teenager dreaming of the future, a worker striving for dignity. To understand HIV/AIDS is not only to grasp the science but also to recognize the humanity of those affected.
HIV/AIDS teaches us that health is not just about biology—it is about justice, resilience, and the power of community. It shows us that even in the face of one of history’s deadliest pandemics, humanity can innovate, adapt, and hope.
The journey is not over, but each breakthrough, each life saved, and each barrier overcome brings us closer to a world where HIV/AIDS is no longer a shadow over human life, but a challenge we have finally conquered.