Few words in the language of medicine carry the same weight as cancer. For many, hearing this diagnosis feels like standing at the edge of an abyss—filled with fear, uncertainty, and questions that touch the very essence of life. Cancer is not simply one disease but a vast family of conditions that affect millions worldwide, crossing all borders, ages, and cultures.
Yet, despite its gravity, the story of cancer is not only about despair. It is also a story of resilience, discovery, and hope. It is about the human body’s extraordinary complexity, the brilliance of scientific research, and the courage of those who confront it. To understand cancer is to understand both the vulnerabilities and the strengths of human biology.
This article explores cancer in its many dimensions: what causes it, how it manifests, how doctors diagnose it, and how it can be treated. It is a journey into one of the most profound challenges of modern medicine, written with both scientific clarity and emotional depth.
What is Cancer?
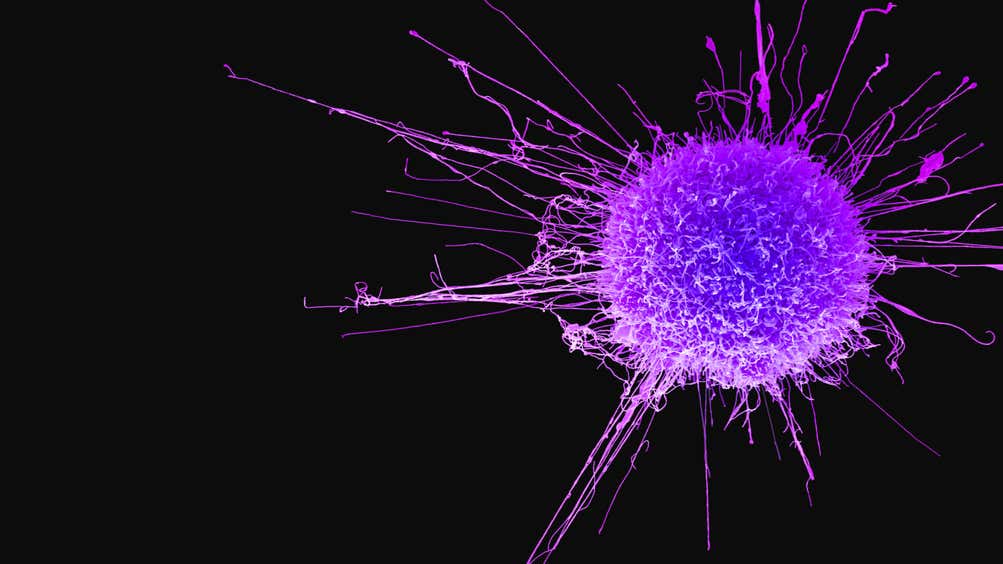
Cancer is a disease of unregulated growth. At its core, it begins when cells—normally obedient units in the body’s vast community—stop following the rules. Instead of growing, dividing, and dying in an orderly fashion, cancer cells ignore signals to stop, evade programmed cell death, and begin multiplying uncontrollably.
A healthy human body consists of trillions of cells, all following genetic instructions that ensure harmony. In cancer, these instructions are corrupted. Mutations in DNA, whether inherited or acquired, change the behavior of cells. Instead of working for the good of the organism, cancer cells become selfish, consuming resources and spreading harm.
Over time, these cells can form tumors—abnormal masses of tissue that can invade nearby structures and spread to distant organs, a process known as metastasis. While not all cancers form solid tumors (leukemia, for instance, affects the blood and bone marrow), the unifying feature of cancer is disobedience to the body’s normal checks and balances.
The Causes of Cancer: Why Cells Rebel
Genetic Mutations
At the heart of cancer lies damage to DNA, the instruction manual of life. Mutations can occur spontaneously during cell division or be triggered by environmental factors. These genetic changes may activate oncogenes (genes that drive cell growth) or inactivate tumor suppressor genes (genes that normally stop growth or repair DNA damage).
Environmental and Lifestyle Factors
While mutations can be random, many arise from external exposures:
- Tobacco smoke is one of the strongest carcinogens, linked to lung, throat, and bladder cancers.
- Radiation, whether from the sun’s ultraviolet rays or medical imaging, can damage DNA.
- Chemicals such as asbestos, benzene, and pesticides have been tied to cancer development.
- Diet and obesity also play major roles, with processed meats, excessive alcohol, and sedentary lifestyles increasing risk.
Infections
Certain viruses and bacteria contribute to cancer by inserting their own genetic material into human cells or causing chronic inflammation. Human papillomavirus (HPV) is linked to cervical and throat cancers, while hepatitis B and C can lead to liver cancer.
Heredity
Some individuals inherit genetic mutations that predispose them to cancer. Mutations in the BRCA1 and BRCA2 genes, for example, significantly increase the risk of breast and ovarian cancers. While inherited mutations account for only about 5–10% of cancers, they underscore how genetics shapes vulnerability.
The Role of Aging
Cancer is often described as a disease of aging. The longer we live, the more chances there are for DNA damage to accumulate. Combined with declining immune surveillance, this makes older adults more susceptible.
The Symptoms of Cancer: Listening to the Body
Cancer is elusive. In its early stages, it often produces no symptoms, allowing it to grow silently. When symptoms do appear, they vary depending on the type, location, and stage of the cancer. Still, certain warning signs are common across many forms.
- Unexplained weight loss: Rapid loss of weight without changes in diet or exercise may signal cancers of the stomach, lung, or pancreas.
- Fatigue: Not ordinary tiredness, but deep, unrelenting exhaustion that doesn’t improve with rest.
- Pain: Persistent pain in bones, the back, or internal organs may point to tumors pressing on nerves or spreading to new sites.
- Skin changes: Moles that change shape, size, or color can indicate melanoma, while yellowing of the skin may suggest liver involvement.
- Persistent cough or hoarseness: Especially when accompanied by blood in sputum, this can suggest lung or throat cancer.
- Unusual bleeding or discharge: Blood in the stool, urine, or sputum often warrants urgent evaluation.
- Changes in bowel or bladder habits: Prolonged constipation, diarrhea, or urinary changes can indicate colorectal or bladder cancer.
The challenge is that these symptoms can also result from noncancerous conditions. That is why diagnosis requires careful investigation rather than assumptions.
Diagnosis: How Doctors Unmask Cancer
Diagnosing cancer is both science and art. It requires listening to the patient’s history, observing subtle clues, and employing powerful technologies.
Medical History and Physical Examination
The first step is always the conversation. Doctors listen to symptoms, family history, and lifestyle factors, followed by a physical exam to detect lumps, swelling, or other abnormalities.
Imaging Studies
Modern imaging allows physicians to peer inside the body without surgery:
- X-rays reveal tumors in bones or lungs.
- CT scans provide detailed cross-sectional images of internal organs.
- MRI uses magnetic fields to visualize soft tissues, invaluable for brain and spinal tumors.
- PET scans highlight metabolic activity, since cancer cells often consume more sugar than normal cells.
Laboratory Tests
Blood tests can detect tumor markers—substances produced by cancer cells or by the body in response to cancer. For example, PSA levels may be elevated in prostate cancer, while CA-125 is linked to ovarian cancer.
Biopsy
A biopsy, the removal and examination of tissue under a microscope, remains the gold standard of diagnosis. Pathologists look for abnormal cell structures, growth patterns, and genetic mutations.
Molecular and Genetic Testing
With advances in precision medicine, doctors now analyze the genetic profile of tumors to guide treatment. For instance, lung cancers with EGFR mutations may respond to targeted drugs that block those pathways.
The Treatment of Cancer: Battling the Rogue Cells
Cancer treatment is one of medicine’s most complex fields, combining surgery, radiation, chemotherapy, targeted drugs, immunotherapy, and supportive care. The choice depends on the cancer type, stage, genetic features, and the patient’s overall health.
Surgery
For localized cancers, surgery can remove the tumor and sometimes cure the disease. Advances in minimally invasive techniques, robotic surgery, and reconstructive procedures have reduced complications and improved outcomes.
Radiation Therapy
Radiation uses high-energy beams to destroy cancer cells by damaging their DNA. It can be delivered externally or internally (brachytherapy). Precision techniques such as intensity-modulated radiation therapy (IMRT) minimize damage to surrounding tissues.
Chemotherapy
Once the cornerstone of cancer treatment, chemotherapy involves drugs that kill rapidly dividing cells. While effective, it also harms healthy cells, leading to side effects like nausea, hair loss, and fatigue. New regimens aim to balance potency with tolerability.
Targeted Therapy
Unlike chemotherapy, targeted drugs act on specific molecules driving cancer growth. Examples include trastuzumab for HER2-positive breast cancer or imatinib for chronic myeloid leukemia. These therapies are often more precise and less toxic.
Immunotherapy
One of the most revolutionary advances, immunotherapy harnesses the body’s own immune system to fight cancer. Checkpoint inhibitors, for instance, “release the brakes” on immune cells, enabling them to attack tumors. CAR T-cell therapy, meanwhile, engineers a patient’s own immune cells to hunt down cancer.
Hormone Therapy
For hormone-sensitive cancers like breast or prostate cancer, drugs can block hormones or reduce their levels, slowing tumor growth.
Palliative and Supportive Care
Not all treatments aim at cure. Sometimes the focus shifts to controlling symptoms, improving quality of life, and supporting patients emotionally and physically. Pain relief, nutrition, counseling, and integrative therapies all form part of comprehensive cancer care.
Living with Cancer: Beyond the Medical Battle
A cancer diagnosis reshapes life. It affects not only the body but also the mind, emotions, relationships, and sense of identity. Patients may face fear of recurrence, changes in appearance, or challenges in daily functioning. Families, too, experience emotional strain, balancing hope with uncertainty.
Support systems—friends, family, therapists, and support groups—are crucial. They provide not only practical help but also the comfort of shared understanding. Many patients also find resilience through spirituality, creative expression, or advocacy, transforming their struggle into a source of strength.
Prevention: The Power of Choices
While not all cancers can be prevented, lifestyle choices significantly reduce risk. Avoiding tobacco, moderating alcohol, maintaining a healthy weight, exercising regularly, and eating a balanced diet rich in fruits and vegetables all support cellular health. Vaccines such as HPV and hepatitis B provide protection against infection-related cancers.
Early detection is equally vital. Regular screenings—Pap smears, mammograms, colonoscopies, prostate checks—catch cancers when they are most treatable. Public awareness campaigns and accessible healthcare systems make a profound difference in outcomes.
The Future of Cancer Medicine
The battle against cancer is far from over, but the horizon is filled with promise. Advances in genomics, nanotechnology, and artificial intelligence are paving the way for earlier detection and personalized treatments. Liquid biopsies, which detect cancer DNA in blood, may soon allow for noninvasive screening of multiple cancers at once.
Artificial intelligence is helping pathologists analyze images more accurately, while 3D bioprinting may one day allow scientists to model tumors and test drugs outside the body. The dream is not only to treat cancer more effectively but to prevent or even eradicate it.
Conclusion: From Darkness to Light
Cancer is a formidable adversary, but it is not invincible. It is a reminder of life’s fragility but also of human resilience and ingenuity. For every story of loss, there are stories of survival, breakthroughs, and moments of profound courage.
To understand cancer is to see both the enemy and the path forward: the mutations that fuel it, the symptoms that reveal it, the science that diagnoses it, and the treatments that combat it. It is to recognize that cancer is not just a biological disease but a human experience—one that demands compassion as much as it does innovation.
And while the journey may be long, every step in research, prevention, and treatment brings us closer to a world where cancer no longer inspires fear, but respect for the progress humanity has made against it.