Few health conditions cast as long and heavy a shadow across the globe as heart disease. Often called the “silent killer,” it is responsible for more deaths each year than any other illness. Behind every statistic lies a story: a mother suddenly gone too soon, a grandfather struggling to climb stairs, a young athlete shocked by a diagnosis, or a family left grieving. Heart disease is not just a medical condition—it is a deeply human experience that disrupts lives, burdens families, and tests the strength of entire healthcare systems.
To understand heart disease is to look closely at one of the most extraordinary organs in the human body: the heart. Roughly the size of a fist, it beats about 100,000 times a day, pumping blood through nearly 60,000 miles of blood vessels. This unceasing rhythm is what sustains life. When disease interrupts that rhythm—through blocked arteries, weakened muscle, or electrical malfunctions—the results can be devastating.
And yet, heart disease is not inevitable. It is influenced by lifestyle, environment, genetics, and medical care. By exploring its causes, symptoms, diagnosis, and treatments, we can not only understand the disease but also learn how to prevent and manage it, preserving the most vital rhythm we all share.
What is Heart Disease?
The term “heart disease” does not describe a single illness but a family of conditions that affect the structure and function of the heart. It includes coronary artery disease (the most common type), arrhythmias, heart failure, cardiomyopathies, valvular diseases, and congenital heart defects.
Coronary artery disease (CAD) alone accounts for the majority of cases. In CAD, the blood vessels that supply the heart with oxygen-rich blood become narrowed or blocked by fatty deposits known as plaques. This process, called atherosclerosis, is slow, silent, and progressive—but when a plaque ruptures, it can trigger a heart attack, a potentially fatal event.
Other forms of heart disease may not involve the arteries at all but rather the heart’s muscle, valves, or electrical system. Despite their differences, all share a common thread: they reduce the heart’s ability to pump blood efficiently, robbing the body of oxygen and energy.
Causes of Heart Disease
The causes of heart disease are complex and multifactorial. They involve a combination of modifiable lifestyle choices, underlying health conditions, environmental exposures, and genetic predispositions.
Atherosclerosis and Its Triggers
At the heart of most cases of coronary artery disease lies atherosclerosis—the buildup of fatty deposits inside arteries. These deposits are made up of cholesterol, cellular waste, calcium, and fibrin. Over time, plaques stiffen the arteries, restricting blood flow and increasing the risk of rupture and clot formation.
Several factors accelerate atherosclerosis:
- High blood pressure (hypertension): Constant pressure damages the arterial walls, making them more vulnerable to plaque buildup.
- High cholesterol: Excess low-density lipoprotein (LDL), often called “bad cholesterol,” contributes to plaque formation, while low levels of high-density lipoprotein (HDL), the “good cholesterol,” hinder the body’s ability to clear excess cholesterol.
- Smoking: Chemicals in tobacco damage blood vessels, reduce oxygen supply, and promote clotting.
- Diabetes: High blood sugar harms blood vessels and increases the risk of plaque buildup.
- Obesity: Excess fat tissue promotes inflammation, raises cholesterol, and contributes to hypertension and diabetes—all of which feed heart disease.
Lifestyle and Behavioral Factors
Choices we make daily play a critical role in shaping heart health. Diets high in processed foods, saturated fats, and added sugars fuel cardiovascular risk. Sedentary lifestyles weaken the heart and circulation. Chronic stress keeps blood pressure elevated and hormones imbalanced, while alcohol and drug abuse place additional strain on the heart muscle.
Genetic and Familial Influence
Sometimes, heart disease runs in families. Inherited traits can increase cholesterol levels, blood clotting tendencies, or structural abnormalities of the heart. Familial hypercholesterolemia, for instance, is a genetic disorder that results in dangerously high cholesterol levels from birth. While lifestyle matters greatly, some individuals are predisposed to heart disease regardless of healthy habits.
Environmental and Socioeconomic Factors
Health does not exist in isolation—it is shaped by environment and society. People living in polluted areas face higher cardiovascular risks. Socioeconomic status also matters; limited access to nutritious food, safe exercise spaces, and quality healthcare fuels disparities in heart health. Stress from financial insecurity or discrimination further compounds the burden.
Symptoms of Heart Disease
Heart disease often develops quietly, with few or no symptoms in its early stages. This is why it is frequently called a silent killer. Yet, as the disease progresses, the body sends warning signals that should never be ignored.
Common Warning Signs
- Chest pain or discomfort (angina): Often described as pressure, squeezing, or fullness in the chest. It may radiate to the arm, neck, jaw, or back.
- Shortness of breath: Difficulty breathing during activity or at rest indicates the heart is struggling to pump efficiently.
- Fatigue: Persistent, unexplained tiredness may point to reduced oxygen delivery.
- Palpitations: Irregular, rapid, or pounding heartbeats may signal arrhythmias.
- Swelling in the legs, ankles, or abdomen: A hallmark of heart failure as fluid accumulates.
Symptoms of Heart Attack
A heart attack, or myocardial infarction, occurs when blood flow to part of the heart is blocked, starving it of oxygen. Symptoms include:
- Sudden chest pain or tightness
- Pain radiating to the left arm, neck, or jaw
- Shortness of breath
- Cold sweats
- Nausea or vomiting
- Lightheadedness or fainting
It’s worth noting that women, older adults, and people with diabetes may experience atypical symptoms, such as fatigue, indigestion-like discomfort, or dizziness rather than classic chest pain. These subtle signs are often overlooked, leading to delayed treatment.
Symptoms of Arrhythmias
When the heart’s electrical system malfunctions, arrhythmias arise. Symptoms include palpitations, dizziness, fainting, or in severe cases, sudden cardiac arrest. Some arrhythmias are harmless, but others can be life-threatening.
Diagnosis of Heart Disease
Detecting heart disease requires a careful blend of patient history, physical examination, and diagnostic testing. Early and accurate diagnosis can save lives.
Medical History and Physical Exam
Doctors begin with a detailed medical history, asking about symptoms, lifestyle habits, family history, and risk factors such as smoking or diabetes. A physical exam may reveal signs like high blood pressure, abnormal heart sounds, or swelling in the extremities.
Blood Tests
Blood tests measure cholesterol, triglycerides, blood sugar, and markers of inflammation such as C-reactive protein. In cases of suspected heart attack, enzymes like troponin are checked to detect heart muscle damage.
Electrocardiogram (ECG or EKG)
An ECG records the electrical activity of the heart. It reveals irregular rhythms, signs of previous heart attacks, and areas of poor blood flow.
Echocardiogram
This ultrasound test uses sound waves to create images of the heart in motion. It helps assess pumping strength, valve function, and structural abnormalities.
Stress Testing
Stress tests evaluate how the heart responds to exertion. The patient walks on a treadmill or pedals a stationary bike while heart activity is monitored, revealing problems not visible at rest.
Cardiac Catheterization and Angiography
In this invasive procedure, a thin tube (catheter) is threaded through blood vessels to the heart. Dye is injected, and X-ray images show blockages in the coronary arteries. This remains the gold standard for diagnosing coronary artery disease.
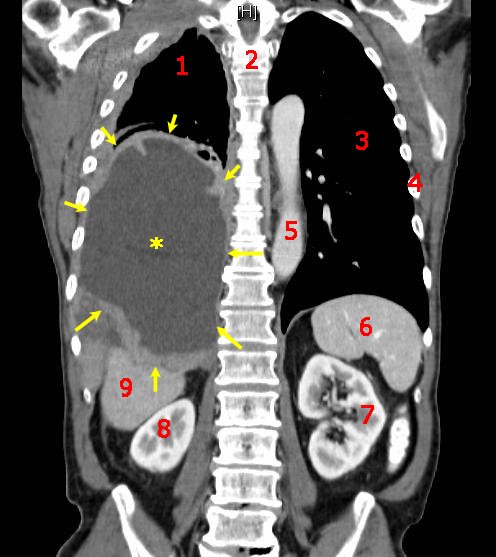
Advanced Imaging
Technologies such as CT scans, MRI, and nuclear imaging provide detailed pictures of heart anatomy, blood flow, and tissue health, offering a comprehensive view when other tests are inconclusive.
Treatment of Heart Disease
Treating heart disease requires a multifaceted approach, combining lifestyle changes, medications, medical procedures, and long-term management. The goal is not only to relieve symptoms but also to prevent progression, improve quality of life, and extend lifespan.
Lifestyle Modifications
Lifestyle change is the cornerstone of prevention and treatment. These adjustments often yield results as powerful as medication:
- Dietary changes: Emphasizing fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting processed foods, sodium, and sugars.
- Exercise: Regular physical activity strengthens the heart, improves circulation, lowers blood pressure, and reduces stress.
- Weight management: Achieving a healthy weight eases strain on the heart and lowers risks of diabetes and hypertension.
- Smoking cessation: Quitting smoking rapidly reduces cardiovascular risk.
- Stress reduction: Mindfulness, meditation, and counseling can alleviate stress’s damaging effects on the heart.
Medications
Doctors often prescribe medications to control risk factors, ease symptoms, and prevent complications:
- Statins: Lower cholesterol and stabilize plaques.
- Antihypertensives: Including ACE inhibitors, beta-blockers, and calcium channel blockers to lower blood pressure.
- Antiplatelet drugs: Such as aspirin, to reduce clot formation.
- Anticoagulants: Prevent dangerous blood clots in patients with atrial fibrillation or artificial valves.
- Diuretics: Reduce fluid buildup in heart failure.
- Antiarrhythmics: Help control abnormal heart rhythms.
Medical Procedures and Surgeries
When lifestyle changes and medications are not enough, medical intervention is necessary.
- Angioplasty and stenting: A balloon is used to open blocked arteries, and a stent (tiny mesh tube) is placed to keep them open.
- Coronary artery bypass grafting (CABG): Surgeons create new pathways around blocked arteries using blood vessels from elsewhere in the body.
- Valve repair or replacement: Damaged valves are repaired or replaced with mechanical or biological valves.
- Implantable devices: Pacemakers regulate slow heart rhythms; implantable cardioverter-defibrillators (ICDs) prevent sudden cardiac death.
- Heart transplant: In end-stage heart failure, a donor heart may be the only option.
Long-Term Management and Rehabilitation
Cardiac rehabilitation programs help patients recover from heart attacks or surgeries. They combine supervised exercise, education, counseling, and support, empowering patients to live healthier lives and reduce the risk of recurrence.
Living with Heart Disease
A diagnosis of heart disease is not the end of the road. Many people live long, fulfilling lives after diagnosis by adhering to treatment plans, staying active, and building strong support networks. Emotional health plays a vital role here; depression and anxiety are common after cardiac events, but with counseling and support, individuals can regain confidence and purpose.
Community also matters. Family encouragement, peer support groups, and access to quality healthcare all contribute to better outcomes. Heart disease, while daunting, can be managed with resilience, knowledge, and the right resources.
The Future of Heart Disease Care
Medicine is advancing rapidly, and with it comes hope for better prevention and treatment. Personalized medicine, guided by genetic testing, promises therapies tailored to each individual. Stem cell research explores the possibility of regenerating damaged heart tissue. Wearable devices and artificial intelligence are enabling continuous monitoring and earlier detection of problems.
Public health initiatives are equally important. Campaigns to reduce smoking, promote healthy diets, and improve healthcare access have already saved millions of lives. The next frontier lies in addressing social determinants of health, ensuring that heart health is not a privilege but a right for all.
Conclusion: Protecting the Rhythm of Life
The heart is more than a pump—it is a symbol of life, love, and resilience. When it falters, the effects ripple far beyond the body. But heart disease, though formidable, is not unbeatable. By understanding its causes, recognizing its symptoms, seeking timely diagnosis, and embracing effective treatments, we can protect the rhythm that sustains us.
Every heartbeat is a gift. Protecting it—through healthier choices, compassionate care, and collective effort—is one of the most important responsibilities we carry, both for ourselves and for the generations that follow.