When the world first encountered COVID-19, the immediate focus was survival—avoiding infection, finding treatments, and developing vaccines. But as the years passed, it became clear that for many, the story didn’t end with recovery. Long after the virus left their bodies, people reported fatigue, breathlessness, brain fog, and an unsettling feeling that something inside them had changed. Now, new research suggests that one of those hidden changes may lie deep within our blood vessels.
A study published in the European Heart Journal reveals that COVID-19, particularly in women, may accelerate the aging of blood vessels by about five years. This is not just a medical curiosity—it could mean a higher risk of heart attack, stroke, and other cardiovascular diseases for millions of people worldwide.
Why Blood Vessel Aging Matters
As we grow older, our arteries naturally lose some of their elasticity. Flexible, youthful arteries allow blood to flow easily, but stiff arteries increase pressure on the heart and raise the risk of serious cardiovascular events. Doctors call this process “vascular aging,” and it usually progresses slowly over decades.
The new findings suggest COVID-19 speeds up that process. In other words, a woman in her 40s who experienced COVID might now have the blood vessels of someone in her mid-40s—or worse, if her infection was severe. That’s a silent but important shift, because even small increases in arterial stiffness translate into measurable increases in risk.
Professor Rosa Maria Bruno, from Université Paris Cité in France and the study’s lead author, put it plainly: “We believe that this may result in what we call early vascular aging, meaning that your blood vessels are older than your chronological age and you are more susceptible to heart disease.”
How the Study Was Conducted
The research team examined 2,390 people from 16 different countries, including Austria, Brazil, France, Italy, the UK, and the US. Participants were grouped based on whether they never had COVID, had a mild infection treated at home, were hospitalized, or had been admitted to intensive care.
To measure vascular aging, scientists used a device that calculates carotid-femoral pulse wave velocity (PWV)—a test that measures how quickly a pulse of blood travels between the neck and the leg. The faster the pulse wave travels, the stiffer the arteries.
These measurements were taken six months after infection and again at 12 months. The results were compared across groups, while also accounting for age, sex, and other health factors.
What the Researchers Found
The results were striking. Compared to people who had never had COVID, those who were infected showed stiffer arteries—even if their infection was mild. And the effect was much stronger in women.
For women, the increase in PWV was about 0.55 meters per second after a mild infection, 0.60 if hospitalized, and 1.09 if they had been in intensive care. An increase of just 0.5 meters per second is considered clinically meaningful and roughly equivalent to aging blood vessels by five years.
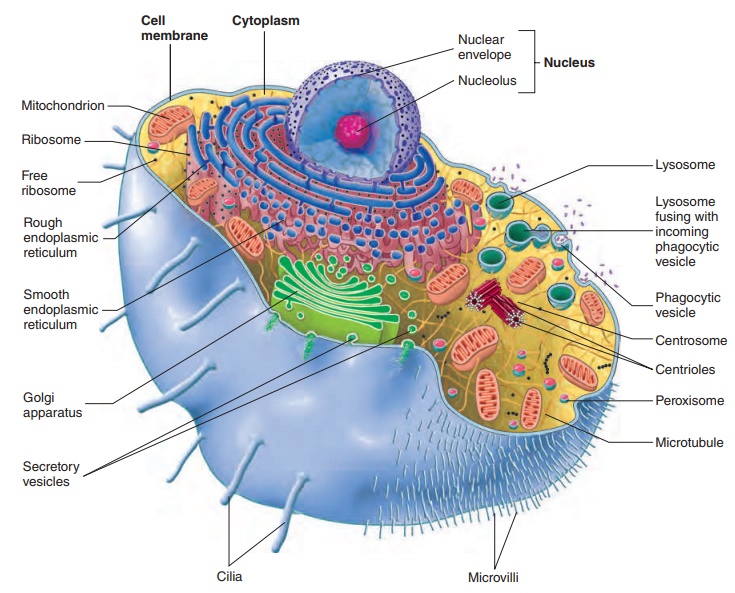
Professor Bruno explained that the virus uses ACE2 receptors, found on the inner lining of blood vessels, to enter cells. This can directly damage the vascular system. In addition, the body’s immune and inflammatory responses may worsen the problem. Women, who tend to mount stronger immune responses, may experience more vessel damage after infection, which could explain the sex difference.
The Role of Long COVID
The study also found that people with long COVID symptoms—persistent fatigue, shortness of breath, and brain fog—were more likely to have accelerated vascular aging. This suggests that the same processes contributing to lingering symptoms may also be silently reshaping cardiovascular health.
While this is concerning, the researchers also offered a glimmer of hope: over time, some improvement was seen. The stiffening of blood vessels seemed to stabilize or even slightly reverse after a year, suggesting the body may gradually heal.
Vaccination as a Protective Factor
One of the more encouraging findings was that people who had been vaccinated before contracting COVID tended to have less stiffening of their arteries compared to those who were unvaccinated. This reinforces what scientists have long suspected: vaccines not only protect against severe illness in the short term but may also help prevent long-term complications.
What This Means for Heart Health
The implications of this research are profound. Millions of people worldwide have had COVID, and if even a portion of them experience accelerated vascular aging, there could be a ripple effect on cardiovascular disease rates in the coming decades.
But the message is not one of despair. Arterial stiffness is something doctors can measure, monitor, and treat. Lifestyle changes such as exercise, healthy diet, stress reduction, and quitting smoking all help improve vascular health. In addition, common medications like blood pressure and cholesterol-lowering drugs are known to reduce arterial stiffness.
Professor Bruno emphasized: “For people with accelerated vascular aging, it is important to do whatever possible to reduce the risk of heart attacks and strokes.”
A New Frontier in Post-COVID Care
The findings raise important questions for the future. Should routine vascular age testing become part of post-COVID checkups? How long do these vascular changes last, and do they always stabilize, or do some people continue to worsen? And crucially, can targeted therapies reverse the damage?
Dr. Behnood Bikdeli of Harvard Medical School, writing in an editorial accompanying the study, warned that while the acute crisis of the pandemic has faded, a new challenge is unfolding: the long-term burden of post-COVID syndrome. He highlighted that up to 40% of COVID survivors may develop persistent symptoms lasting months or years. Among these survivors, vascular aging could be an unseen but dangerous consequence.
Looking Ahead
COVID-19 has left scientists, doctors, and patients with a new mystery: how a respiratory virus can leave fingerprints on the heart and blood vessels long after the infection is gone.
What this study makes clear is that our battle with COVID is not only about preventing infection—it’s about understanding and protecting long-term health. For women in particular, the risk of accelerated vascular aging underscores the importance of vigilance, follow-up care, and proactive steps to safeguard cardiovascular well-being.
COVID-19 may be fading from the headlines, but inside the human body, its effects may echo for years to come. The challenge now is to recognize those echoes and act before they turn into a wave of preventable heart disease.
More information: Rosa Maria Bruno et al, Accelerated vascular ageing after COVID-19 infection: the CARTESIAN study, European Heart Journal (2025). DOI: 10.1093/eurheartj/ehaf430