In late 2019, the world stood on the brink of an event that would change every aspect of human life. What began as a mysterious cluster of pneumonia-like cases in Wuhan, China, quickly spiraled into one of the most devastating pandemics in modern history. Within weeks, countries closed borders, cities fell silent under lockdowns, and billions of people found themselves united in fear, uncertainty, and resilience against an invisible enemy—COVID-19.
COVID-19, caused by the novel coronavirus SARS-CoV-2, reshaped societies, tested healthcare systems, and reminded humanity of its fragility and interconnectedness. It was not merely a medical crisis—it became a social, economic, and psychological phenomenon that will be studied for generations. But behind the headlines, the panic, and the heartbreak lies a story of science: how the virus emerged, how it spread, how it attacks the body, and how humans fought back with knowledge, medicine, and innovation.
To understand COVID-19, we must explore its causes, recognize its symptoms, grasp the tools of diagnosis, and examine the treatments that saved millions of lives.
The Cause: SARS-CoV-2, the Invisible Invader
Origins of the Virus
COVID-19 is caused by SARS-CoV-2, a coronavirus belonging to the same family as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome). Coronaviruses are named for their crown-like spikes visible under electron microscopes. These spikes are not just decoration—they are molecular keys that allow the virus to unlock and enter human cells.
Though research continues, the prevailing theory is that SARS-CoV-2 originated in animals, possibly bats, and made the leap to humans through an intermediate host. Such “spillover events” are not new—HIV, influenza, and Ebola all emerged from animals. What made SARS-CoV-2 unique was its combination of high transmissibility and potential severity.
How the Virus Infects
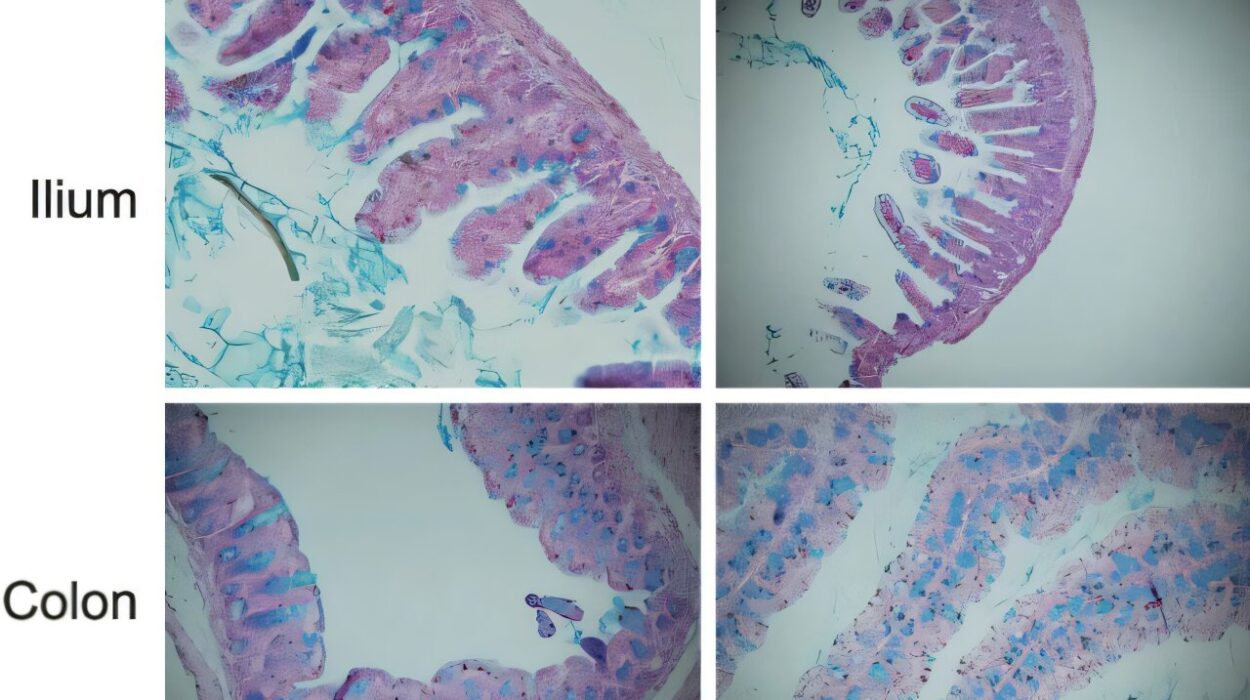
The viral spikes bind to a receptor called ACE2, found on the surface of many human cells, especially in the lungs, heart, kidneys, and intestines. Once attached, the virus enters the cell, hijacks its machinery, and turns it into a factory for producing more viruses. This process spreads rapidly, overwhelming tissues and triggering an immune response.
In some individuals, the immune system mounts a measured defense that clears the virus. In others, the response spirals out of control, causing inflammation that damages the lungs and other organs—a phenomenon known as a “cytokine storm.” This imbalance between viral replication and immune response explains why COVID-19 can be mild in some but deadly in others.
Symptoms: The Many Faces of COVID-19
COVID-19 proved to be a chameleon-like disease. Some infected people never showed symptoms, while others developed life-threatening illness. This unpredictability made containment and treatment challenging.
Common Symptoms
The most frequently reported symptoms included:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Loss of taste or smell
- Sore throat
- Congestion or runny nose
- Headache
These symptoms typically appeared within 2 to 14 days after exposure, reflecting the virus’s incubation period.
Severe Manifestations
In severe cases, COVID-19 progressed to pneumonia, acute respiratory distress syndrome (ARDS), multi-organ failure, and death. Patients struggling to breathe often required supplemental oxygen or mechanical ventilation. The lungs, once inflamed and filled with fluid, could no longer efficiently exchange oxygen—a critical hallmark of severe disease.
The Role of “Long COVID”
Even after recovery, many individuals continued to experience lingering symptoms, a condition termed “Long COVID.” These included chronic fatigue, brain fog, shortness of breath, chest pain, and difficulty concentrating. Long COVID highlighted that survival did not always mean a full return to health. For some, the virus left an enduring mark.
Diagnosis: Unmasking the Virus
Diagnosing COVID-19 quickly and accurately was essential to slowing its spread and protecting lives. In the early days of the pandemic, the absence of reliable tests contributed to widespread transmission. Over time, several methods emerged to detect the virus or confirm past infection.
Molecular Testing (RT-PCR)
The gold standard was the reverse transcription polymerase chain reaction (RT-PCR) test. This technique detects the virus’s genetic material in nasal or throat swabs. RT-PCR is highly sensitive and specific, meaning it can accurately confirm infection even when viral levels are low. However, it requires specialized equipment and trained personnel, making widespread deployment challenging in resource-limited settings.
Antigen Testing
Antigen tests detect viral proteins rather than genetic material. They are faster and cheaper than PCR, often delivering results in minutes. However, they are less sensitive, meaning false negatives are more common—especially in people with low viral loads. Still, antigen tests proved invaluable for mass screening, especially in schools, workplaces, and airports.
Antibody Testing
Antibody (serology) tests detect immune responses to SARS-CoV-2 rather than the virus itself. They cannot diagnose active infection but can reveal whether someone was previously infected. Antibody tests were critical for understanding how widely the virus had spread and for estimating population-level immunity.
Imaging and Clinical Assessment
Chest X-rays and CT scans revealed characteristic patterns in COVID-19 pneumonia, such as “ground-glass opacities.” While not definitive, imaging helped assess severity and guided treatment decisions.
Treatment: Fighting Back Against COVID-19
At the beginning of the pandemic, treatment options were limited. Doctors relied on supportive care—oxygen, fluids, and mechanical ventilation for the critically ill. But as research accelerated at an unprecedented pace, new therapies emerged.
Supportive Care
Most patients with mild to moderate illness were treated at home with rest, hydration, and over-the-counter medications to relieve fever and pain. For hospitalized patients, oxygen therapy became a cornerstone. In intensive care units, ventilators supported patients with ARDS when their lungs could no longer function independently.
Antiviral Medications
Several antiviral drugs showed promise. Remdesivir, initially developed for Ebola, was repurposed and found to shorten recovery time in hospitalized patients. Later, oral antivirals such as Paxlovid (nirmatrelvir/ritonavir) were developed, reducing the risk of severe illness when given early.
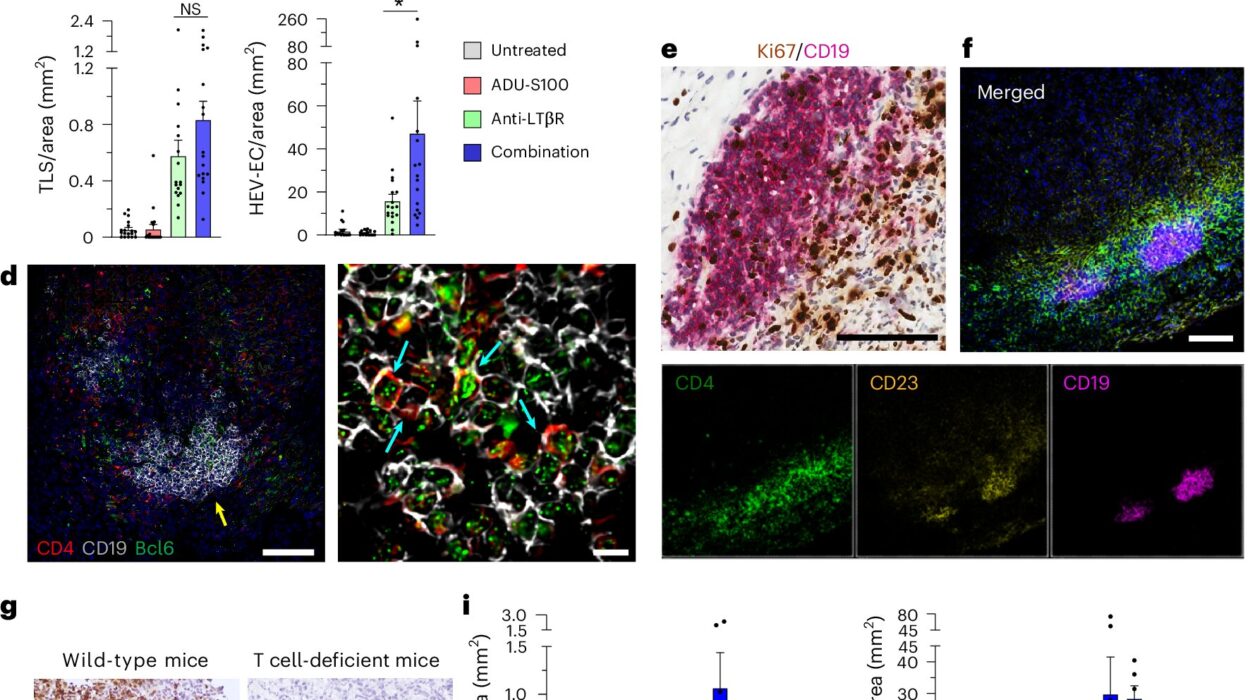
Anti-Inflammatory Treatments
Recognizing that severe COVID-19 often resulted from an overactive immune response, doctors turned to anti-inflammatory drugs. Dexamethasone, a corticosteroid, reduced mortality in patients requiring oxygen or ventilation. This was a turning point, demonstrating that calming the immune system could be as crucial as fighting the virus itself.
Monoclonal Antibodies
Engineered monoclonal antibodies targeted the virus’s spike protein, neutralizing it before it could infect cells. Drugs like bamlanivimab and casirivimab-imdevimab were given to high-risk patients early in infection to prevent progression to severe disease. Their effectiveness varied as new viral variants emerged, but they saved countless lives in the early waves.
Vaccines: The Game Changer
Perhaps the greatest triumph against COVID-19 was the rapid development of vaccines. Using novel mRNA technology (Pfizer-BioNTech and Moderna) and viral vector platforms (AstraZeneca and Johnson & Johnson), scientists delivered effective vaccines within a year—a feat once thought impossible.
Vaccines trained the immune system to recognize the spike protein, preparing the body to respond quickly if exposed to the actual virus. They dramatically reduced severe illness, hospitalization, and death. Boosters were later developed to address waning immunity and new variants.
The Role of Global Cooperation
The speed of vaccine development was not just a triumph of science but also of global collaboration. Researchers shared data across borders, governments poured billions into research, and manufacturing scaled at unprecedented levels. Despite challenges in distribution and hesitancy, vaccines remain humanity’s most powerful weapon against COVID-19.
The Social and Emotional Toll
While the virus attacked the body, the pandemic attacked societies. Lockdowns disrupted economies, isolated families, and fueled mental health crises. Anxiety, depression, and loneliness surged. Healthcare workers endured exhaustion, trauma, and burnout on the frontlines. Children lost months of schooling, and vulnerable populations bore the brunt of economic hardships.
Yet, amid the suffering, stories of resilience emerged. Communities organized food drives, neighbors supported one another, and scientists achieved breakthroughs that will shape medicine for decades. The pandemic revealed both the vulnerabilities and the strength of the human spirit.
Variants: The Virus Evolves
As the virus spread, it mutated, giving rise to variants with new properties. The Alpha, Delta, and Omicron variants became household names. Delta caused more severe illness, while Omicron spread with unprecedented speed but often led to milder outcomes.
Variants challenged vaccines and treatments, forcing scientists to adapt quickly. Booster shots, updated vaccines, and combination therapies became essential tools in staying ahead of viral evolution.
Lessons Learned and the Road Ahead
COVID-19 was not humanity’s first pandemic, nor will it be the last. But it left profound lessons:
- Preparedness matters: Investments in public health infrastructure, surveillance, and rapid response systems are essential.
- Science saves lives: The unprecedented pace of research and vaccine development showed what is possible when resources and collaboration align.
- Health is interconnected: The pandemic highlighted how individual behaviors, community actions, and global cooperation are intertwined.
- Mental health cannot be ignored: Addressing psychological well-being is as important as treating physical illness.
The fight against COVID-19 continues, but humanity is better equipped than before. Through vigilance, innovation, and compassion, we can shape a healthier, more resilient future.
Conclusion: Beyond the Virus
COVID-19 was more than a medical event; it was a mirror reflecting the strengths and weaknesses of humanity. It revealed the vulnerability of global systems, the courage of healthcare workers, the fragility of economies, and the resilience of communities. It tested science, politics, and human compassion all at once.
At its core, the story of COVID-19 is a story of cause and effect—of a virus crossing into humans, of symptoms ranging from mild to deadly, of diagnosis evolving from scarce tests to rapid tools, and of treatments advancing from supportive care to vaccines.
But it is also a story of humanity—our fear, our grief, our perseverance, and our triumphs. While the scars of the pandemic will remain, so will the knowledge that even in the darkest times, science, solidarity, and the human spirit can light the way forward.