In the ongoing battle against viruses, scientists have made a significant breakthrough that could change the way we fight infections. But this time, the approach is not about targeting the virus directly—it’s about focusing on the body’s own defenses. Researchers at the Department of Energy’s Pacific Northwest National Laboratory (PNNL) have discovered a new way to protect the body from a range of viral invaders, from the common cold to COVID-19, by fortifying the very cells that viruses hijack.
The idea might sound simple, but it’s a radical shift in how we think about treating viral infections. Instead of trying to stop a specific virus in its tracks, the team aims to fortify the body’s defenses to stop not just one virus, but many. This new approach could lead to treatments that prevent viruses from taking over cells in the first place, making it harder for them to spread or mutate.
“The virus thrives by taking over the cellular machinery of its host, hijacking normal processes to churn out copies of itself,” said John Melchior, a biochemist and a corresponding author of a paper published in the Journal of Proteome Research. “We want to identify and then fortify the molecular complexes that are susceptible to many invading viruses—to stop viruses before they have a chance to take over the cell.”
This concept of turning the body’s own machinery against viruses marks an exciting new frontier in viral defense. By manipulating the control points within the cell, the researchers aim to block the virus from completing its mission. If successful, it would be a major step forward in the fight to combat multiple types of viral infections with a single drug.
Targeting the Cell, Not the Virus
Traditionally, antiviral drugs are designed to target the virus itself—trying to block it from infecting cells, preventing it from replicating, or stopping it from spreading. While this method has its merits, viruses can evolve quickly, leading to drug resistance and making it harder to stay one step ahead.
The new approach proposed by Melchior, virologist Amy Sims, and their team shifts the focus. Instead of targeting the virus directly, they aim to target the processes inside our own cells that the virus relies on to reproduce. This strategy could potentially block not just one virus, but many.
“This approach offers a pathway for using a single drug to stop multiple types of viruses,” said Sims, the co-corresponding author of the study. “When you target only the virus, it can produce strains that readily escape antiviral medications. But by targeting key functions in the host cell that the virus needs to replicate, and by turning off those host functions, we hope to eliminate the escape route most viruses use to cause disease.”
The team’s breakthrough builds on a newer technique that allows scientists to pinpoint not just which proteins are abundant in a cell, but how those proteins change shape when the cell is infected. This technique, called limited proteolysis-based mass spectrometry (LiP-MS), tracks how proteins’ shapes shift in response to viral infection, giving researchers a more detailed map of how viruses interact with human cells at a molecular level.
By focusing on how proteins in our cells are altered during viral infections, the team identified several key proteins that viruses hijack to replicate themselves. These discoveries offer a new way to stop viruses before they can spread, not just in individual cells, but in the body as a whole.
A Sneak Peek into How the Virus Hijacks the Cell
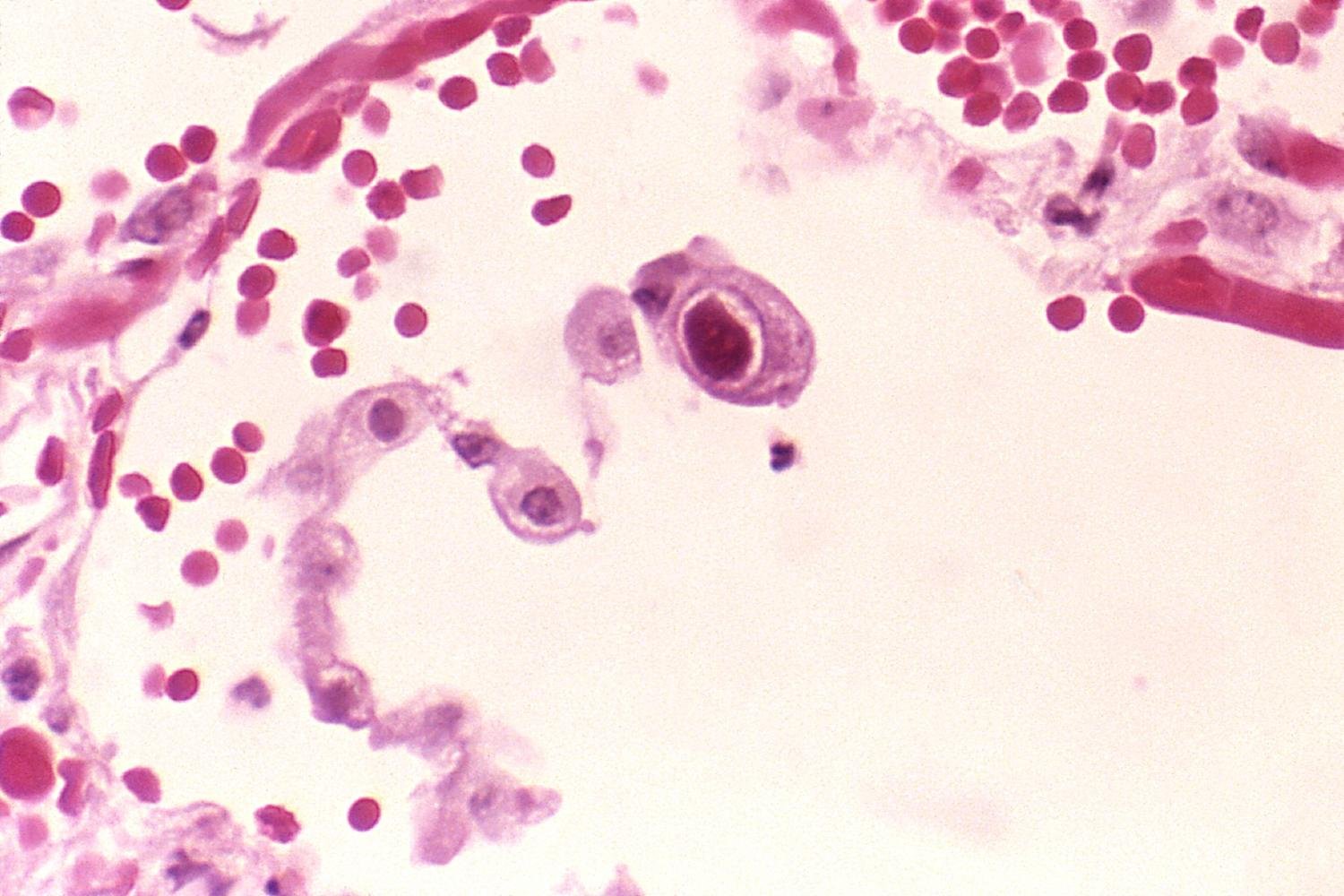
In their study, the researchers examined human cells infected with the common cold virus, HCoV-229E, which belongs to the same family of coronaviruses as MERS-CoV and SARS-CoV-2. This virus, while often mild, provides valuable insight into how viruses manipulate human cells.
One of the molecular targets they uncovered is Nop-56, a protein that helps the body distinguish between normal and rogue RNA strands. Normally, Nop-56 tags RNA with a chemical stamp of approval, signaling to the ribosome that it’s legitimate. With that signal, the ribosome can create the protein the RNA codes for. However, when the cold virus hijacks Nop-56, the process is corrupted. Instead of normal proteins being made, the virus redirects the system to churn out its own proteins, which can be used to create more copies of the virus.
Another important target identified by the team is the spliceosome C-complex. This molecular machine helps cells edit RNA strands by removing unnecessary sections. When the virus takes control of this assembly, it can divert the cell’s resources away from making essential proteins and instead produce viral ones that will help it replicate and spread.
Picture a factory that, in times of peace, manufactures essential supplies for the country’s defense. But in the event of an invasion, the factory gets taken over and repurposed to churn out weapons for the enemy. That’s essentially what happens when a virus invades the body—cellular machinery is hijacked to build the virus rather than the body’s normal proteins.
The Promise of a Broad-Spectrum Defense
The PNNL team believes that their research opens the door to developing drugs that could block not just one virus but many. By targeting the key cellular processes viruses rely on, they hope to prevent viruses from mutating and escaping treatment. Unlike current antiviral drugs that are tailored to specific viruses, these drugs could be effective against a wide range of viral pathogens.
“We hope our work provides a list of common molecular targets that sets the foundation for the development of drugs that could block not just one but many viruses that cause disease,” said Snigdha Sarkar, a postdoctoral fellow and first author of the study. “Viruses can mutate quickly, and that poses a problem when targeting a virus directly. That obstacle is removed if you target proteins that many viruses rely upon in the host.”
With the team now exploring existing antiviral compounds and utilizing artificial intelligence to identify potential new drugs, the path forward looks promising. This combination of cutting-edge research and innovative technology may soon lead to therapies that protect us from a broad spectrum of viral infections.
Why This Research Matters
This research is more than just a step forward in understanding how viruses invade human cells—it has the potential to revolutionize how we think about viral infections. By focusing on the host cell’s vulnerabilities, rather than chasing after specific viruses, the PNNL team is opening up an entirely new approach to antiviral drug development.
If successful, this strategy could lead to treatments that work against a range of viruses, from the common cold to more severe diseases like COVID-19, without the risk of resistance that plagues current antiviral drugs. In a world where viruses mutate and spread with alarming speed, this could be a game-changer—offering us a new line of defense, not just for today, but for the future.
As the research progresses and the potential of this approach is realized, we may soon find ourselves better equipped to stop viral infections before they take hold—protecting not just individuals, but entire communities from the next wave of viral threats.
More information: Snigdha Sarkar et al, Human Coronavirus-229E Hijacks Key Host-Cell RNA-Processing Complexes for Replication, Journal of Proteome Research (2025). DOI: 10.1021/acs.jproteome.5c00400